Overview of Prostate Cancer
Top Contributors - Stacy Schiurring, Kim Jackson, Lucinda hampton and Jess Bell
Introduction[edit | edit source]
Prostate cancer affects the prostate gland, which is part of the male reproductive system and functions to create seminal fluid.
- In 2020, there were an estimated 1.4 million new cases of prostate cancer and 375,000 prostate cancer related deaths worldwide[1]
- Prostate cancer was the second most frequent cancer and the fifth leading cause of cancer death among men[1]
- It was the most frequently diagnosed cancer in men in over one-half of the countries of the world[1]
- Differences in prostate cancer diagnostic practices are most likely the greatest contributor to the worldwide variation in prostate cancer incidence rates[1]
- The majority of men diagnosed with prostate cancer have a slow growing variation of the disease that is nonthreatening to their natural life expectancy and can be safely monitored without need for medical intervention[2]
- For those men diagnosed with metastatic prostate cancer, only 28% will survive beyond five years of diagnosis[2]
- The prognosis worsens if the cancer has a chance to spread, metastasis rapidly involves the lymphatic system, lungs, bone marrow, liver or adrenal glands[2]
The treatment of prostate cancer is a common entryway into the speciality area of men's health physiotherapy because these patients can be effectively treated without competency in the full scope of men's health skills such as the internal examination and use of real-time ultrasound.[3] Please follow these links to learn more about physiotherapy assessment and treatment of men's health conditions.
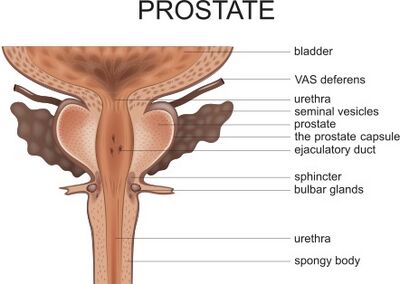
Anatomy Review[edit | edit source]
- The prostate is a gland located immediately below the internal urethral sphincter and surrounds the commencement of the urethra. The external urethral sphincter is immediately below the prostate. It is situated in the pelvic cavity: below the lower part of the symphysis pubis, above the superior fascia of the urogenital diaphragm, and in front of the rectum. It can be palpated, especially when enlarged.[4] It is about the size of a walnut.[3]
- The prostate is perforated by both the urethra and the ejaculatory ducts. The ejaculatory ducts open into the prostatic portion of the urethra.[4]
- Arterial supply: internal pudendal, inferior vesical, and middle hemorrhoidal.[4]
- Innervation: receives sympathetic input via the hypogastric nerve and parasympathetic input via the pelvic nerve. The hypogastric and pelvic nerves also provide sensory inputs to the gland.[5]
- The prostate gland is divided into three anatomical lobes: two anterior and one median[2]
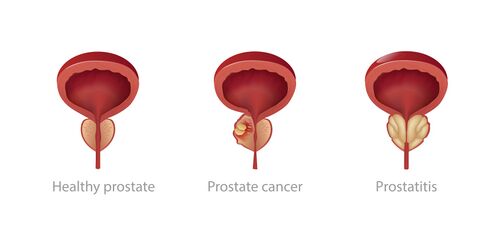
- Knowing the anatomy of the prostate is central to the understanding of both benign and malignant prostatic pathologies. This is because the area of the prostate the pathology originates is a defining characteristic of each of the three main prostate diseases. The three main diseases of the prostate are:[2]
- Benign prostate hyperplasia (BPH)
- Prostate cancer
- Chronic prostatitis
- Knowing the anatomy of the prostate is central to the understanding of both benign and malignant prostatic pathologies. This is because the area of the prostate the pathology originates is a defining characteristic of each of the three main prostate diseases. The three main diseases of the prostate are:[2]
Characteristics/Clinical Presentation[edit | edit source]
Early prostate cancer may be asymptomatic, routine screenings of prostate cancer are commonly being done on asymptomatic men.
Clinical Signs and Symptoms:
- Difficulty starting urination
- Weak or interrupted flow of urine
- Frequent urination, especially at night
- Difficulty emptying the bladder completely
- Pain or burning during urination
- Blood in the urine or semen
- Pain in the back, hips, or pelvis that doesn’t go away
- Painful ejaculation or orgasm[3]
It is important to note that these signs and symptoms may also be present with other noncancerous prostate-related disease conditions such as BPH or prostatitis. If a patient presents with the above symptoms, referral to a medical doctor or urologist is urgently recommended for proper diagnosis.
Cancer is one condition that can affect the prostate and cause enlargement of the gland. When the prostate enlarges, it can compress the urethra and cause difficulties with urine flow. An enlarged prostate is not always lead to a diagnosis of prostate cancer, rather that further testing in indicated for proper differential diagnosis.[3]
If a patient reports symptoms of sexual dysfunction, it is important to ask about the timeline of their issues. It is of greater concern if the sexual dysfunction issue involves orgasm and ejaculation, and have occurred within the previous few months. A referral should be made for differential diagnosis.[3]
Tumor Staging[edit | edit source]
- The diagnosis of prostate cancer is established via a biopsy of the prostate gland
- A small piece of the prostate gland is removed and examined under a microscope for cancer cells. If cancer cells are found then a Gleason score will be determined from the biopsy. A Gleason score indicates how likely the cancer is to spread. It ranges from 2–10, the lower the score the less likely it is that cancer will spread
- False-negative results often occur; therefore, multiple biopsies may be done before prostate cancer can be detected and confirmed
Stage I: Cancer cannot be felt during a digital rectal exam, but it may be found during surgery being done for another reason. Cancer has not yet spread to other areas.
Stage II: Cancer can be felt during a digital rectal exam or discovered during a biopsy. Cancer has not yet spread.
Stage III :Cancer has spread to nearby tissue
Stage IV: Cancer has spread to lymph nodes or to other parts of the body
Prostate Cancer Risk Factors[edit | edit source]
While the prevalence of prostate cancer is common, relatively little is known about its etiology.[1] There are several known risk factors that have been shown to indicate an increase in the risk of developing this type of cancer, however many patients with one or more risk factors never get cancer, while others who get cancer may have had few or no known risk factors.
The following are risk factors for prostate cancer according to the American Cancer Society:
- Age: rare in men under 40yo, chance rises rapidly after age 50. About 6 in 10 cases of prostate cancer are found in men older than 65.
- Race/ethnicity: develops more often in African American men and in Caribbean men of African ancestry, less often in Asian American and Hispanic/Latino men than in non-Hispanic whites. The reasons for these racial and ethnic differences are unclear.
- Geography: most common in North America, northwestern Europe, Australia, and on Caribbean islands. It is less common in Asia, Africa, Central America, and South America. The reasons for this are not clear.
- Family history: seems to run in some families, which suggests there may be a genetic factor in some cases. However, most prostate cancers occur in patients without a family history of it.
- Gene changes: several inherited gene mutations seem to raise prostate cancer risk a small percentage.
Factors with less clear effects on prostate cancer risk:
- Diet: the exact role of diet in prostate cancer is unclear. Some studies suggest that men who consume a lot of dairy or calcium (through food or supplements) may have a higher risk of developing prostate cancer.
- Obesity: there may be a weak link between obesity and risk of developing more aggressive prostate cancer. The reasons for this are not clear.
- Smoking: some research has linked smoking to a possible small increased risk of dying from prostate cancer, but further research is indicated.
- Chemical exposures: the National Academy of Medicine considers there to be “limited/suggestive evidence” of a link between Agent Orange exposure and developing prostate cancer.
- Inflammation of the prostate: there is a possible link between prostatitis and an increased risk of developing prostate cancer. This is an area of ongoing research.
- Sexually transmitted infections: there is a possible link between sexually transmitted infections such as gonorrhea or chlamydia and increased risk of prostate cancer.
- Vasectomy: some studies have suggested that there is an increased risk for prostate cancer after undergoing a vasectomy.
Prostate Cancer Tests and Screenings[edit | edit source]
A patient will often receive a routine digital rectal exam and or prostate screening antigen (PSA) test. If either of these screenings give the medical provider concern about a potential diagnosis of prostate cancer, they will order a biopsy and or an MRIto confirm the diagnosis. Overall health status is important when making medical decisions, patients should talk to their healthcare provider about the pros and cons of being tested and treated for prostate cancer.
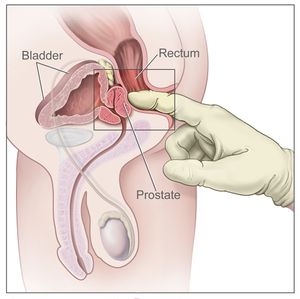
Digital Rectal Examination[edit | edit source]
- An exam in which the doctor inserts a finger into the rectum to allow the ability to palpate the back of the prostate gland to assess for enlargement or abnormal growths.
- There is a lack of evidence to support the efficacy of DRE. The majority of patients diagnosed with prostate cancer have abnormal PSA levels, but normal DRE results.
- This test may still be included in screening because even though it is less effective than a PSA blood test overall it may still be able to detect cancer in men that may demonstrate normal PSA levels
Prostate-Specific Antigen (PSA) Test[edit | edit source]
- A blood test used to test for elevated levels of PSA, which occurs with any changes in the prostate.
- The risk of disease increases as the PSA level increases; however, a normal level of PSA has not been determined.
- No PSA level guarantees the absence of prostate cancer.
- There are several factors that may increase PSA levels.
- Although PSA remains the gold-standard exam for possible prostate cancer diagnosis it contributes significantly to over-treatment of men with less aggressive prostate cancer. This is a significant issue, as medical treatments for prostate cancer are associated with side effects that can have a significant negative impact on a patient's quality of life[2], such as sexual dysfunction and urinary incontinence.[3]
Factors that might raise PSA levels include:
- Enlarged prostate
- Prostatitis
- Older age: PSA levels normally increase slowly with age
- Ejaculation: can increase PSA a short time, therefore some doctors suggest that men abstain from ejaculation for a day or two before testing.
- Riding a bicycle: studies suggest that cycling may temporarily raise PSA levels
- Certain medicines: taking male hormones such as testosterone, or other medicines that raise testosterone levels
raise PSA levels
Factors that might lower PSA levels (even if a man has prostate cancer):
- 5-alpha reductase inhibitors: drugs used to treat BPH or urinary symptoms, such as finasteride (Proscar or Propecia) or dutasteride (Avodart), can lower PSA levels
- Herbal mixtures: some dietary supplements might mask a high PSA level
- Certain medicines: research has suggested that long-term medicine use may lower PSA levels. These medications can include: aspirin, statins, and thiazide diuretics (such as hydrochlorothiazide). More research is needed to confirm these findings.
Biopsy[edit | edit source]
- The diagnosis of prostate cancer is established via a biopsy of the prostate gland and may be indicated for individuals who have elevated PSA levels.
- A small piece of the prostate gland is removed and examined under a microscope for cancer cells. If cancer cells are found then a Gleason score will be determined from the biopsy.
- A biopsy will confirm if a patient has prostate cancer. If prostate cancer is found on a biopsy, this test can also help tell how likely it is that the cancer will grow and spread quickly.[8]
- MRI can also be used to diagnose prostate cancer.[3]
Treatment Options[edit | edit source]
The first decision in managing prostate cancer is determining whether any treatment at all is needed. Prostate cancer, especially low-grade tumors, often grow so slowly that frequently no treatment is required particularly in elderly patients and those with comorbidities that would reasonably limit life expectancy to 10 additional years or less.
The interprofessional team can optimize the treatment of these patients through communication and coordination of care. Primary care providers, urologists, oncologists, radiation oncologists, and nurse practitioners provide diagnoses and care plans. The interprofessional team can improve outcomes for patients with prostate cancer through use of the biopsychosocial treatment model.
There are two main options for treatment of prostate cancer: surgical and radiation, however there are new technologies coming out and research being done continuously. Often the decision between surgical and radiation treatments comes down to potential side-effects, it is important to discuss these side-effects with patients when making treatment decisions as they have a strong effect on quality of life post-procedure.[3]
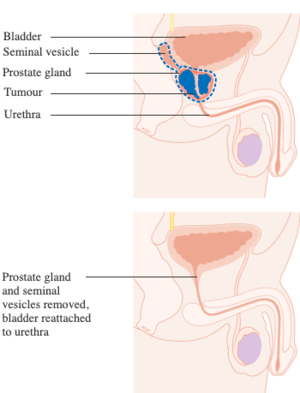
Surgical Interventions[edit | edit source]
Prostatectomy: This involves the removal of the prostate gland. A radical prostatectomy is the removal of the prostate gland and some surrounding tissue. A prostatectomy is a completed and lengthy surgery, lasting 4-6 hours.[3]
Types of prostatectomies:[3]
- Open prostatectomy
- Laparoscopic prostatectomy
- Robot-assisted prostatectomy
Potential side-effects of prostatectomy:
- Post-surgical pain: usually resolves quickly
- High likelihood of urinary incontinence: most likely stress incontinence. Majority of patients recover their continence with therapy interventions.
- Sexual dysfunction: only 30-40% of patients will regain sexual functioning. Patients will be anejaculate with orgasm due to removal of seminal vesicles with prostatectomy; penile changes such as penile shortening and curvature changes. Some patients may loose the ability to achieve an erection if the cavernous nerves could not be sparred during the surgical intervention.
Radiation[edit | edit source]
Use of high-energy radiation to try to destroy the cancer cells. There are two types of radiation therapy that differ by how radiation is applied to a diseased prostate:[3]
- External beam radiation therapy: the radiation is directed into the cancer cells from the outside of the body. Can have more side-effects due to radiation effecting the tissue surrounding the prostate, including the rectum, as it travels through the body.
- Brachytherapy (Internal radiation therapy): Radioactive pellets surgically implanted into the cancerous area to try to destroy the cells from the inside of the body. Radiation is contained in a specific area to destroy only targeted cells, causing less general tissue damage.
Potential side-effects of radiation treatment:
- Side-effects often do not appear until 2-5 years after treatment due to radiation build-up in tissues surrounding the prostate with gradual tissue decay/destruction. Not all patients who receive radiation treatment will develop side-effects.
- Urinary incontinence: most likely urge incontinence due to development of bladder irritation.
- Sexual dysfunction: changes in ejaculatory function and quantity due to fibrotic tissue changes post-radiation; penile changes such as penile shortening and curvature changes.
Active Surveillance[edit | edit source]
Many low-risk cases can now be followed with active surveillance. Under active surveillance, patients are usually required to have regular, periodic PSA testing and at least one additional biopsy 12 to 18 months after the original diagnosis.
Treatment of Advanced Prostate Cancer[edit | edit source]
- Androgen Deprivation Therapy
- Orchidectomy
These patients have little to no prospect of sexual function return due to the lack of test
Role of Physiotherapy[edit | edit source]
The role of physiotherapy in the treatment of people with prostate cancer is to improve the likelihood of successful outcomes following surgical or radiation treatments to provide the highest level of quality life possible. This is done by providing:[3]
- Pre-treatment pelvic floor rehab
- Post-treatment pelvic floor rehab
- Encouraging active and fit lifestyles
- Behavioural modification
- Lifestyle modification
- Addressing both incontinence and sexual dysfunction issues for best likelihood of return of function
The physiotherapist can play a role in recognizing any treatment regret, depression, and or anxiety in this patient population, and guide them to manage "life after prostate cancer" with the interdisciplinary team as part of the biopsychosocial model.[3]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, Bray F. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: a cancer journal for clinicians. 2021 May;71(3):209-49.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Tonry C, Finn S, Armstrong J, Pennington SR. Clinical proteomics for prostate cancer: understanding prostate cancer pathology and protein biomarkers for improved disease management. Clinical Proteomics. 2020 Dec;17(1):1-31.
- ↑ 3.00 3.01 3.02 3.03 3.04 3.05 3.06 3.07 3.08 3.09 3.10 3.11 3.12 Roscher, P. Men's Health. Overview of Prostate Cancer. Physioplus. 2022
- ↑ 4.0 4.1 4.2 Gray H. Anatomy of the human body. Philadelphia: Lea & Febiger, 1918; Bartleby. com, 2000.
- ↑ White CW, Xie JH, Ventura S. Age-related changes in the innervation of the prostate gland: implications for prostate cancer initiation and progression. Organogenesis. 2013 Jul 1;9(3):206-15.
- ↑ Centers for Disease Control and Prevention. What Are the Symptoms of Prostate Cancer? Available from: https://www.cdc.gov/cancer/prostate/basic_info/symptoms.htm (accessed 14/04/2022).
- ↑ 7.0 7.1 American Cancer Society. Prostate Cancer Risk Factors. Available from: https://www.cancer.org/cancer/prostate-cancer/causes-risks-prevention/risk-factors.html (accessed 16/04/2022).
- ↑ 8.0 8.1 8.2 American Cancer Society. Screening Tests for Prostate Cancer. Available from: https://www.cancer.org/cancer/prostate-cancer/detection-diagnosis-staging/tests.html(accessed 16/04/2022).