Beta-Blockers
Introduction[edit | edit source]
Beta-blockers are a broad class of medications that are used for various clinical benefits but also carry the potential for adverse effects[1].
Beta blockers uses range from lowering blood pressure to improving heart failure (once a mainstay for treating high blood pressure, beta blockers have been elbowed aside by newer drugs, such as ACE inhibitors, and older ones, such as thiazide diuretics).
Beta receptors (tiny proteins) sit on the outer surface of many cells. There are three main types.
- Beta-1 receptors are found almost exclusively in heart cells.
- Beta-2 receptors reside mostly in lung and blood vessel cells, though heart cells also have some.
- Beta-3 receptors are located on fat cells.[2]
Beta receptors latch onto chemical messengers released by the nervous system and initiate sympathetic activation eg the heart beats faster, blood vessels constrict, the airways relax, and the kidneys increase production of a protein that boosts blood pressure.
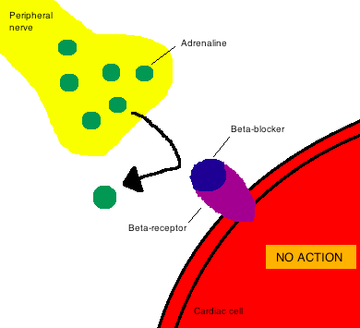
Beta blockers subvert these processes by settling onto beta receptors and preventing the chemical messengers from binding to their receptors eg slows the heart, improves the conduction of electrical signals in the heart, relaxes blood vessels, and lowers blood pressure[2].
Image 1: Beta-blockers cause a competitive inhibition of the β-receptor, which counters the effects of catecholamines. Catecholamines are hormones made by your adrenal glands eg adrenalin. The adrenal glands send catecholamines into the blood when a person is physically or emotionally stressed[3].
Function[edit | edit source]
Beta-blockers, as a class of medications, are essential drugs and are first-line treatments in many acute and chronic conditions.[1] There are two types of beta receptors in the body drugs are target:
- Beta-1 receptors, which are present in the heart
- Beta-2 receptors, which are present in vascular smooth muscle and the muscle lining the airways.
More than a dozen beta blockers have been approved for use in the United States (see table). They fall into three main groups.
- Nonselective. These are first-generation beta blockers. They will block some of both beta 1 and beta 2 receptors. They can slow not only cardiac output, but also the renal and other systems. You may lower blood pressure but risk kidney or breathing problems[4].
- Cardioselective. A number of beta blockers are designed to block only beta-1 receptors in heart cells. Since they don't affect beta-2 receptors in blood vessels and the lungs, cardioselective beta blockers are safer for people with lung disorders.
- Third-generation. Some beta blockers do more than block beta receptors. eg. Labetalol blocks alpha receptors, too. This further helps relax blood vessels. Nebivolol stimulates the inner lining of blood vessels (the endothelium) to generate nitric oxide, which helps the vessels relax. Carvedilol does both[2].
Uses[edit | edit source]
Hypertension: Beta blockers are commonly prescribed to treat hypertension.
Angina: Decreasing the rate lowers myocardial oxygen demand. Decreasing blood pressure leads to a decrease in afterload, which decreases the workload of the heart, which also lowers myocardial oxygen demand.
Dysrhythmias: Beta blockers are often used to control the rate in atrial fibrillation.
Myocardial infarction: When given within 24-hours of onset, beta blockers reduce cardiac workload and improve likelihood of survival.
Heart failure: Beta blockers are used in coordination with other medications to slow the progression of heart failure. Metoprolol and carvedilol are the main ones used to slow the heart rate (giving the heart time to “rest” between beats) and lower blood pressure, which decreases afterload and, therefore, the workload of the heart.
Migraines: Some beta blockers (such as atenolol, metoprolol, timolol and propranolol) are used to help prevent migraines by inhibiting arterial dilation in the brain.
Glaucoma: Ophthalmic solutions are used to decrease eye pressures, though the mechanisms are not fully understood[5].
Beta Blockers And CHF[edit | edit source]
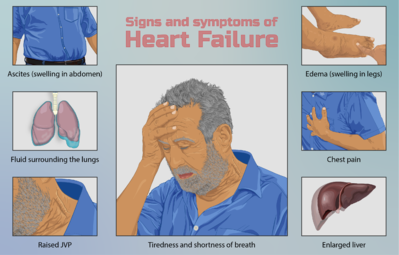
Beta blockers are considered the primary drugs for the pharmacological management of CHF. These drugs provide their beneficial effect by decreasing the excessive activity of the sympathetic nervous system which is characteristic of CHF. Increased sympathetic nervous system activity is a neurohormonal compensation involving the renin-angiotensin system that occurs in CHF patients in order to increase cardiac output of the failing heart and maintain blood pressure. While initially beneficial, these compensations place an ultimately damaging degree of stress on the already failing heart[6].
As their name suggests, the clinically useful beta blockers used to treat CHF bind to beta-adrenergic receptors on the myocardium, blocking the effects of norepinephrine and epinephrine. By this mechanism, beta blockers normalize sympathetic activity reducing heart rate, cardiac contraction force, and angina. These beta blockers are specifically known as beta-1 cardioselective blockers. Another class of beta blockers, beta-2 blockers, are bronchoconstrictors, and thus provide no real clinical value.
Two FDA approved beta blockers commonly used to treat CHF are Carvedilol and Metoprolol, although there are many others that may be used with the discretion of the treating physician[7].
- Carvedilol is taken orally, with dosages ranging from 3.125 mg taken twice daily to a maximal dose of 50 mg taken twice daily. The half-life of carvedilol is 7-10 hours and it is metabolized extensively and excreted in feces via bile with less than 2% excreted unchanged in the urine[8].
- Metoprolol is taken orally starting at dosages of 12.5-25 mg once a day, which can be doubled every two weeks up to 200 mg daily. Metoprolol has a half-life of 3-7 hours and is mostly metabolized by the liver[9].
Side effects[edit | edit source]
A primary potential side effect of beta blockers is bradycardia or an abnormally slow heart rate, which may exacerbate the failing heart’s ability to pump enough blood. Additionally, symptoms of fatigue, weakness, and dizziness are also side effects of beta blockers[8].
Physiotherapy implications [edit | edit source]
While beta blockers may allow patients to participate in therapy less inhibited by angina and with reduced stress on the heart, exercise programs must be prescribed with extreme caution and monitored carefully. Beta blockers may render conventional aerobic workload guidelines inappropriate as they typically decrease maximal heart rate, and consequently have the potential to mislead the therapist prescribing an exercise program.
Beta blockers block conduction at the AV Node, decrease heart rate and lower blood pressure. Watch your patient for bradycardia and hypotension[5]
Heart rate and blood pressure should be monitored frequently, and the patient should be assessed for signs of fatigue, dizziness, and weakness prior to the initiation of the therapy session and monitored throughout.
Resources[edit | edit source]
- ↑ 1.0 1.1 Farzam K, Jan A. Beta blockers. StatPearls [Internet]. 2020 Jul 8.Available:https://www.ncbi.nlm.nih.gov/books/NBK532906/ (accessed 6.4.2021)
- ↑ 2.0 2.1 2.2 Harvard Edu. Beta Blockers: Jack of all trades Available from: https://www.health.harvard.edu/heart-health/beta-blockers-cardiac-jacks-of-all-trades(accessed 4.6.2021)
- ↑ Web med Catecholamines Available:https://www.webmd.com/heart-disease/catecholamines-test-facts (accessed 6.4.2021)
- ↑ Health FAQ beta 1 vs Beta 2 Available from:https://health-faq.com/heart-disease/beta-1-blockers-vs-beta-2-blockers/ (accessed 6.4.2021)
- ↑ 5.0 5.1 Straight a nursing Beta blockers Available:https://www.straightanursingstudent.com/beta-blockers/ (accessed 4.6.2021)
- ↑ King, M. Kingery J, Casey B. Diagnosis and evaluation of heart failure. Am Fam Physician. 2012;85:1161-1168
- ↑ Ciccone, C. D. (2016). Pharmacology in rehabilitation (5th ed.). Philadelphia: F.A. Davis Company.
- ↑ 8.0 8.1 U.S. Food and Drug Administration (FDA). COREG (carvedilol) tablets for oral use. Available online at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/020297s037lbl.pdf. Issued 1995. Last accessed 11/29/18.
- ↑ U.S. Food and Drug Administration (FDA). LOPRESSOR (metoprolol tartrate tablet, injection, solution). Available online at: https://www.accessdata.fda.gov/drugsatfda_docs/label/2008/017963s062,018704s021lbl.pdf. Last Revised 02/2008. Last accessed 11/29/18.