Chronic Rotator Cuff Tendinopathy
Original Editor -Mariam Hashem
Top Contributors - Mariam Hashem, Tarina van der Stockt, Kim Jackson and Wanda van Niekerk
Introduction[edit | edit source]
Rotator Cuff Tendinopathy is a common condition representing 30-70% of shoulder pain disorders[1]. This condition is more significant after the age of 50 and can be attributed to multiple factors.
Rotator Cuff Tendinopathy has adverse consequences on the quality of life and is associated with long-term disability, retirement and high rates of chronicity (40-50%)[2].
To develop effective management strategies, clinicians need to understand the factors contributing to the development of chronicity. Structural, gentic, biomechanical and psychosocial factors play an integral role in the development of Chronic Rotator Cuff Tendinopathy. Additionally, the following five factors have been discussed in recent literature and therefore should be considered when addressing this condition:
- Central Nervous System reorganization
- RC Tendons
- Scapula
- Proprioception
- Central Senstization
Central Nervous System Reorganization[edit | edit source]
While structural-oriented treatment may be effective in acute stages of MSD, the outcomes are relatively poor in chronic stages. This propses a question of what are the reasons beyond the development of chronic pain and disability in Rotator Cuff Tendinopathy? This simply leads us to consider CNS-related factors.
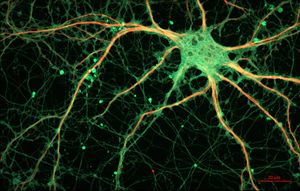
Changes in neuronal structure, organization and properties (Neural plasticity) following MSD can possibly explain altered joint control and persistent pain[3]. Numerous studies have investigated the CNS reorganization associated with different MSD and reported altered perception threshold to sensory stimuli, augmented pain perception and other similar symptoms presented bilaterally and away from the site of injury[4][5][6][7]. A study by Nogomo et al [8] reported cortical reorganization correlating with the magnitude of MS-related pain. Overlap in spatial territory of cortical representation of muscles and alterations in intracortical inhibitory and facilitatory networks were also reported in different studies[9][10]. This supports the hypothesis that structural abnormalities shouldn't always be associated with MS-related symptoms[11].
Selective facilitation of needed muscles and inhibition of others for smooth performance, as well as intermuscular coordination may be disrupted as consequences of CNS reorganization[9][10]. Motor cortical reorganization may persists despite alleviation of pain, leading to modifications in motor strategies to control the affected joint. Eventually, chronicity is likely to occure as a result of the cascades of disruptions.
Understanding maladaptive organizations has great clinical implicaitions. While strength training and endurance training have shown induced angiogenesis in motor cortex and synaptogenesis within spinal cord respectively, skill trianing targets the motor map organization[12]. Rehabilitation strategies should include motor control training in the rehabilitation of chronic RCT[3]. The study of Roy et al [13] features different structural and global approaches to rehabilitate CNS reoganiaztion, including sensorimotor training, pain education and postural exercises.
New therapeuric interventions that aim to modulate neuronal excitability have emerged, however, studies are not sufficient to support their clinical implementation.These include:
- Non-invasive brain stimulations :
- Transcranial direct current stimulation (tDCS)
- Repetitive transcranial magnetic stimulation (rTMS)
- Peripheral neuromuscular stimulations:
- Peripheral electrical stimulation(PES)
- Repetitive peripheral magnetic stimulation(RPMS)
RC Tendons[edit | edit source]
There is a wide debate in the literature regarding shoulder pain terinology. Whether it is a rotator cuff tendinopathy, subacromial pain syndome or subacromial pain impinegemnt syndrome we have to acknowledge the fact the shoulder pain is multifactorial and can be deriven from multiple reasons.
However, in a clinical setting it is better to have objective measures to diffrentiate between rotator cuff tendinopathy and subacromial pain syndrome. This is particularly helpful for rehabilitation decision making[3].
Tendon overload/degenration is likely to be a cause of subacromial pain. Tendons, especially Supraspinatus tendon, also could be compressed mechanically in the subacromial space. However, bony pathologies cannot be attributed as the sole cause of pain. Surgical approaches combined with rehabilitation was found to be no more effective than rehabilitation alone. Therefore, researchers suggest abandoning the ''impingement'' terminology[14].
Intrinsic factors contributing to RC tendons degenration/loading are:
- Vascularity
- Morphology
- Mechanical
- Ageing
- Genetic
Neovascularization, refering to increased blood supply in tendons causing pain, was evident in the lower limb. Kardouni JR[15] reported increased supraspinatus vascularity. Despite this finding, we still need more studies to confirm neovascularity as a contributing factor to RCT. The less vascularity in shoulder tendons and the difficulty in obtaining daignostic images similar to lower limb tendons propse challenges to study this factor [3].
Although there is a wide agreement towards adapting the terminology ''Tendinopathy'' instead of '' tendenitis'', inflammation was reported by Dean BJ[16]. Tendon thickning was also present in tendinopathy as a result of abnormal collagen laydown. however, it starts thinning with progresive tendon disease which may lead to tear. But thickneing isn't always a sign of tendinopathy as it was evident in overhead athletes and spinal cord injuries[3].
In healthy subjects, the distance between the Acromion and Humerus (AHD) is between 10-15 mm. A smaller AHD was observed (7-8 mm)
Compression is likely to be the reason of pain in three circumstances[3]:
- Thicker tendon e.g: overuse or disease
- Smaller distance between Acromion and Humerus AHD (7-8mm). Normally AHD= 10-15 mm.
- Occupation ratio: Supraspinatus Tendon:AHD. If hte tendon occupies > AHD.
AHD is at its smallest between 0-90°. Therefore pain above 90° is likely to be of other reasons.
RCT could be classified as Partial thickness and Full thickness tear. Partial thickness tear could be articular, bursal or mid-substance.
In Full thickness, the tendon may still be intact.
For rehabilitation decision making pruposes, diagnosing shoulder pain could be classified as following:
- Subacromial Pain Syndrome:
- SPS
- Partial Thickness RC tear
- Full Thickness Rotator Cuff Tear (FT-RCT)
Recommendations for Diagnosis[3][edit | edit source] |
||
|---|---|---|
| Subacromial Pain Syndrome (SPS) | Full Thickness Tear (FT-RCT) | |
| Confirm (Rule In): Specifity ≥ 80%. Likelihood ratio ≥ 2.0. | Single Tests[17][18][19][20]:
1-Painful Arc 2-Resisted External Rotation (Pain or Weakness) 3-Full can 4- Drop Arm. Combo Tests[21]: 1-Hawkins 2-Pianful Arc 3-ER resistance. All 3+: +LR of 10.56 All 3-: -LR of 0.17 |
Single Test[17][18][19][20]:
1-Painful Arc 2-Resisted ER 3-Drop Arm 4-ER lag-massive tear 5-Atrophy(infraspinatus) 6-IR lag& lift off 7-Belly off-subscapularis Combo Tests[22]: 1- Age ≥ 65 yo 2-ER marked weakness 3- Night Pain All 3 + :+LR of 9.84 All 3 - : -LR of 0.54 |
| Screen out (Rule Out) : Senstivity ≥ 80%. LR ≤ 0.5 | Single Tests:
1-Painful Arc 2-Resisted ER: Pain or Weakness 3-Hawkins 4-Neer 5-Full Can 6-Empty can ComboTets[23]: 3/5 1-Hawkins 2-Neer 3-Painful Arc 4-Empty Can 5-ER resistance If ≥ 3+ /5 : +LR of 2.93 If < 3+ / 5: - LR of 0.34 |
Single Tests:
1-Resisted ER→marked weakness 2-IR lag and lift off 3-Full Can 4-Empty Can Combo Tests[21]: 1-Drop Arm 2-Painful Arc 3-ERRT All 3 + R/In: + LR of 15.57 All 3 - R/Out: -LR of 0.16 |
| [24] | [25] |
| [26] | [27] |
| [28] | [29] |
| [30] | [31] |
| [32] | [33] |
Scapula[edit | edit source]
In healthy individuals, scapular movement is controled through balnced activation patterns as follows:
- Prime Movers
- Dynamic Stabilizers
- Postural Muscles
Alterd muscle activation patterns in scapula in relation to RCT can be summarized in the following table[34][35][36]:
| Hypoactive muscles | Hyperactive muscles | Hypo or Hyperactive muscles | |
|---|---|---|---|
| Lower Trapezius
Middle Trapezius Serratus Anterior |
Pectoralis Minor
Levator Scapula |
Upper Trapezius
Rhomboid |
Since Scapula plays an integral role in bridging shoulder complex to the spine[37], overloading the RC tendons to maintain GH stability is possible.Therefor it is essential to integrate scapular rehabilitation in the RCT management program[3].
When it comes to deciding which scapular-focused exercise to include in the rehabilitaiton program, clinicians should consider the following[38]:
1- Neuromuscluar Coordination and correcting scapular position conciously.
2-Restoring muscle balance is rather than strenghting.
3-Integrating functional-specific or sport-specific exercises.
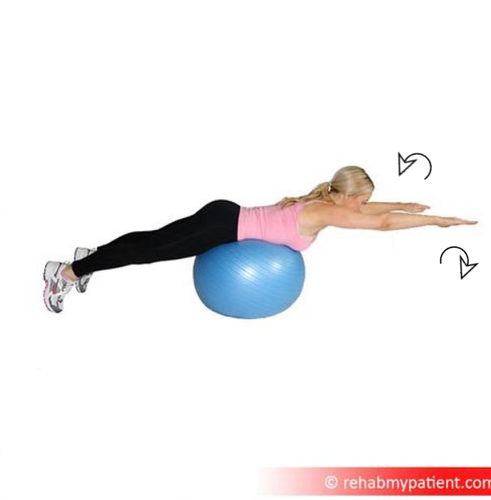
Recommendations for balancing muscle activation patterns[3][36][39]:
- To address middle and lower trapezius muscles hypoactivity/weakness, it is recommended to add exteral rotation in different positions e.g;diagonal pattern and with shoulder elevation.
- Elevation Exercises are preferred over isolated protraction when targeting serratus asnterior muscle.
- Adding external rotation component and/or performing exercises in lying position with head resting are suggested for decreasing upper trapezuis hyperactivity.
- Open chain exercises has been shown to decrease hyperactivity of pectoralis minor.
- Overhead exercises in in closed chain position such as overhead retractions, overhead shrugging and wall slide are recommended to decrease levator scapula hyperactivity.
Integrating core and periphral muscles could be helpful in RCT rehabilitaiton, considering kinetic chain roe of the scapula. Serratus Anterior activation could be targeted by concious contraction of core abdominal muscles[40] and during high load exercises.
Proprioception[edit | edit source]
When deciding to include scapular-focused management program, clinincians should be aware of the effectiveness of the program as supported by evidence, patient's functional aspiations and demands, level of tissue irritability and the assumed muscle activation levels during the exercise[3].
Central Senstization[edit | edit source]
References[edit | edit source]
- ↑ Oliva F, Piccirilli E, Bossa M, Via AG, Colombo A, Chillemi C, Gasparre G, Pellicciari L, Franceschetti E, Rugiero C, Scialdoni A. IS Mu. LT-rotator cuff tears guidelines. Muscles, ligaments and tendons journal. 2015 Oct;5(4):227.
- ↑ Kuijpers T, van der Windt DA, Boeke AJ, Twisk JW, Vergouwe Y, Bouter LM, van der Heijden GJ. Clinical prediction rules for the prognosis of shoulder pain in general practice. Pain. 2006 Feb 1;120(3):276-85.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 WCPT 2017: Rotator Cuff Tendinopathy (FS-16). [Presentation]. World Confideration for Physical Therapy 2 July 2017. [27 Sep 2018] Available from: https://www.youtube.com/watch?v=driyaw7ALDg
- ↑ Wilder-Smith OH, Tassonyi E, Arendt-Nielsen L. Preoperative back pain is associated with diverse manifestations of central neuroplasticity. Pain. 2002 Jun 1;97(3):189-94.
- ↑ Jensen R, Kvale A, Baerheim A. Is pain in patellofemoral pain syndrome neuropathic?. The Clinical journal of pain. 2008 Jun 1;24(5):384-94.
- ↑ Latremoliere A, Woolf CJ. Central sensitization: a generator of pain hypersensitivity by central neural plasticity. The Journal of Pain. 2009 Sep 1;10(9):895-926.
- ↑ Pelletier R, Higgins J, Bourbonnais D. Is neuroplasticity in the central nervous system the missing link to our understanding of chronic musculoskeletal disorders?. BMC musculoskeletal disorders. 2015 Dec;16(1):25.
- ↑ Ngomo S, Mercier C, Bouyer LJ, Savoie A, Roy JS. Alterations in central motor representation increase over time in individuals with rotator cuff tendinopathy. Clinical Neurophysiology. 2015 Feb 1;126(2):365-71.
- ↑ 9.0 9.1 Schabrun SM, Hodges PW, Vicenzino B, Jones E, Chipchase LS. Novel adaptations in motor cortical maps: the relation to persistent elbow pain. Med Sci Sports Exerc. 2015 Apr 1;47(4):681-90.
- ↑ 10.0 10.1 Burns E, Chipchase LS, Schabrun SM. Altered function of intracortical networks in chronic lateral epicondylalgia. European Journal of Pain. 2016 Aug;20(7):1166-75.
- ↑ Lewis J, McCreesh K, Roy JS, Ginn K. Rotator cuff tendinopathy: navigating the diagnosis-management conundrum. journal of orthopaedic & sports physical therapy. 2015 Nov;45(11):923-37.
- ↑ Adkins DL, Boychuk J, Remple MS, Kleim JA. Motor training induces experience-specific patterns of plasticity across motor cortex and spinal cord. Journal of applied physiology. 2006 Dec;101(6):1776-82.
- ↑ Roy JS, Bouyer LJ, Langevin P, Mercier C. Beyond the Joint: The Role of Central Nervous System Reorganizations in Chronic Musculoskeletal Disorders. journal of orthopaedic & sports physical therapy. 2017 Nov;47(11):817-21.
- ↑ Cools AM, Michener LA. Shoulder pain: can one label satisfy everyone and everything?.
- ↑ Kardouni JR, Seitz AL, Walsworth MK, Michener LA. Neovascularization prevalence in the supraspinatus of patients with rotator cuff tendinopathy. Clinical Journal of Sport Medicine. 2013 Nov 1;23(6):444-9.
- ↑ Dean BJ, Gettings P, Dakin SG, Carr AJ. Are inflammatory cells increased in painful human tendinopathy? A systematic review. Br J Sports Med. 2015 Aug 5:bjsports-2015.
- ↑ 17.0 17.1 Hermans J, Luime JJ, Meuffels DE, Reijman M, Simel DL, Bierma-Zeinstra SM. Does this patient with shoulder pain have rotator cuff disease?: The Rational Clinical Examination systematic review. Jama. 2013 Aug 28;310(8):837-47.
- ↑ 18.0 18.1 Hanchard NC, Lenza M, Handoll HH, Takwoingi Y. Physical tests for shoulder impingements and local lesions of bursa, tendon or labrum that may accompany impingement. The Cochrane database of systematic reviews. 2013 Apr 1.
- ↑ 19.0 19.1 Hegedus EJ, Goode AP, Cook CE, Michener L, Myer CA, Myer DM, Wright AA. Which physical examination tests provide clinicians with the most value when examining the shoulder? Update of a systematic review with meta-analysis of individual tests. Br J Sports Med. 2012 Nov 1;46(14):964-78.
- ↑ 20.0 20.1 Alqunaee M, Galvin R, Fahey T. Diagnostic accuracy of clinical tests for subacromial impingement syndrome: a systematic review and meta-analysis. Archives of physical medicine and rehabilitation. 2012 Feb 1;93(2):229-36.
- ↑ 21.0 21.1 Park HB, Yokota A, Gill HS, El Rassi G, McFarland EG. Diagnostic accuracy of clinical tests for the different degrees of subacromial impingement syndrome. JBJS. 2005 Jul 1;87(7):1446-55.
- ↑ Litaker D, Pioro M, Bilbeisi HE, Brems J. Returning to the bedside: using the history and physical examination to identify rotator cuff tears. Journal of the American Geriatrics Society. 2000 Dec;48(12):1633-7.
- ↑ Michener LA, Walsworth MK, Doukas WC, Murphy KP. Reliability and diagnostic accuracy of 5 physical examination tests and combination of tests for subacromial impingement. Archives of physical medicine and rehabilitation. 2009 Nov 1;90(11):1898-903.
- ↑ Painful Arc Syndrome/Shoulder Impingement. Available from:https://www.youtube.com/watch?v=engHP9OA92U
- ↑ Examination of the Rotator Cuff/Infraspinatus Test/Clinical Examination. Available from: https://www.youtube.com/watch?v=R67cIKM3EAM
- ↑ Full Can Test/Shoulder Impingement. Available from: https://www.youtube.com/watch?v=NuBOHdm20cc
- ↑ Drop Arm Tets/Sign/Supraspinatus Tear. Available from:https://www.youtube.com/watch?v=JXgRBeqToik
- ↑ Hawkins Kennedy Test/Shoulder Impingement. Available from:https://www.youtube.com/watch?v=6GkKB2oXi3o
- ↑ Neer Test/Shoulder Impingement. Available from: https://www.youtube.com/watch?v=bXA8cblZUok
- ↑ Jobe/Empty Can Test/Shoulder Impingement. Available from:https://www.youtube.com/watch?v=5BjDQ-jcBek
- ↑ Lateral Rotation Lag Sign/Infraspinatus Weakness. Available from: https://www.youtube.com/watch?v=iUTxEAOrEMY
- ↑ Internal Rotation Lag Sign/Subscapularis Tear. Available from: https://www.youtube.com/watch?v=FbxrdmtjwN8
- ↑ Lift Off Sign/Subscapularis Weakness. Available from:https://www.youtube.com/watch?v=AgkTH52_PBI
- ↑ Castelein B, Cools A, Parlevliet T, Cagnie B. Modifying the shoulder joint position during shrugging and retraction exercises alters the activation of the medial scapular muscles. Manual therapy. 2016 Feb 1;21:250-5.
- ↑ Cools AM, Dewitte V, Lanszweert F, Notebaert D, Roets A, Soetens B, Cagnie B, Witvrouw EE. Rehabilitation of scapular muscle balance: which exercises to prescribe?. The American journal of sports medicine. 2007 Oct;35(10):1744-51.
- ↑ 36.0 36.1 Struyf F, Cagnie B, Cools A, Baert I, Van Brempt J, Struyf P, Meeus M. Scapulothoracic muscle activity and recruitment timing in patients with shoulder impingement symptoms and glenohumeral instability. Journal of Electromyography and Kinesiology. 2014 Apr 1;24(2):277-84.
- ↑ Cools AM, Struyf F, De Mey K, Maenhout A, Castelein B, Cagnie B. Rehabilitation of scapular dyskinesis: from the office worker to the elite overhead athlete. Br J Sports Med. 2013 May 17:bjsports-2013.
- ↑ Cools A. The role of the scapula in shoulder rehabilitation [Research meeting]. Available from:http://www.schoudernetwerkvlaanderen.be/wp-content/uploads/2017/07/3.-Ann-Cools-The-Role-of-The-Scapula.pdf
- ↑ Borms D, Ackerman I, Smets P, Van den Berge G, Cools AM. Biceps disorder Rehabilitation for the Athlete: a Continuum of moderate-to High-Load Exercises. The American journal of sports medicine. 2017 Mar;45(3):642-50.
- ↑ Toro AS, Cools AM, de Oliveira AS. Instruction and feedback for conscious contraction of the abdominal muscles increases the scapular muscles activation during shoulder exercises. Manual therapy. 2016 Sep 1;25:11-8.