Contracted Pelvis: Difference between revisions
(added texts) |
No edit summary |
||
| Line 23: | Line 23: | ||
* The obstetric conjugate: Measured from the sacral promontory to the point bulging the most on the back of the symphysis pubis, located about 1 cm below its upper border. It measures 10.5 cm on average; it is the lesser anteroposterior diameter. | * The obstetric conjugate: Measured from the sacral promontory to the point bulging the most on the back of the symphysis pubis, located about 1 cm below its upper border. It measures 10.5 cm on average; it is the lesser anteroposterior diameter. | ||
* The diagonal conjugate: Measured between the sacral promontory and the lower edge of the pubic symphysis, measuring an average of 12.5. | * The diagonal conjugate: Measured between the sacral promontory and the lower edge of the pubic symphysis, measuring an average of 12.5. | ||
{{#ev:youtube|kTwxNTFP-YA|300}}<ref>Human Anatomy Education. Female bony pelvis: 3-Pelvimetry. Available from: http://www.youtube.com/watch?v=kTwxNTFP-YA [last accessed 21/2/2023]</ref> | |||
Revision as of 20:59, 22 February 2023
Introduction[edit | edit source]
Contracted pelvis considered rare in the developed world, is still prevalent in some developing countries.[1] Labour Dystocia is the most common complication associated with contracted pelvis which leads to increased incidence of perinatal and maternal morbidity as well as mortality.
It is described as one with reduced pelvic dimensions or shape that is sufficiently abnormal to cause difficulty in the delivery of a normal-sized fetus during labour [2]
The female pelvis[edit | edit source]
In obstetrics, the shape, type and diameter of the female pelvis determines the course and outcome of labour.[2][3] The pelvis is made up of the sacrum, the coccyx, and two os coxae Each os coxae is made up of the ischium, the ilium, and the pubis. The pelvis is formed inferiorly between the sacrum and the coccyx (sacrococcygeal symphysis), posteriorly between the sacrum and each ilium (sacroiliac joint), and anteriorly between the pubic bodies (pubic symphysis). [4]
The pelvic cavity is divided into the true pelvis and the false pelvis by the pelvic inlet.[4]
The pelvic inlet, is the anatomical limit between the true pelvis below and the false pelvis above and its regarded as the door way to the birth canal in obstetrics[5]. The pelvic inlet involves three of the four units of which the bone pelvis is composed. The pelvic brim involves the first sacral segment, the iliac and pubis portion, but not the ischium. The dimensions of the pelvic inlet is determined by the general shape of the female pelvis.[5]
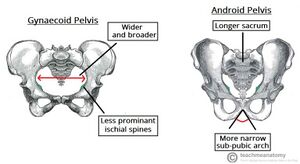
The shape of the pelvic inlet depends on the general shape of the pelvis. Caldwell and Moloy classified the female pelvis into 4 basic pelvic types which are, in order of frequency, gynecoid (∼50%), android, anthropoid, and platypelloid.[3][6]
The gynecoid pelvis is the most suitable for vaginal birth, the anthropoid pelvis is acceptably favorable. While the android and platypelloid are known to be suboptimal.[3][1]
The diameters of the pelvic inlet can be defined as
The anteroposterior (or "conjugate") diameter which is the distance between the pubic symphysis and the sacral promontory. Three distances are:
- The anatomical conjugate or true: Measured between the sacral promontory and the upper edge of the pubic symphysis and measures an average of 11.0 cm
- The obstetric conjugate: Measured from the sacral promontory to the point bulging the most on the back of the symphysis pubis, located about 1 cm below its upper border. It measures 10.5 cm on average; it is the lesser anteroposterior diameter.
- The diagonal conjugate: Measured between the sacral promontory and the lower edge of the pubic symphysis, measuring an average of 12.5.
Causes[edit | edit source]
Diagnostic Procedures[edit | edit source]
add text here relating to diagnostic tests for the condition
Outcome Measures[edit | edit source]
add links to outcome measures here (see Outcome Measures Database)
Management / Interventions
[edit | edit source]
add text here relating to management approaches to the condition
Differential Diagnosis
[edit | edit source]
add text here relating to the differential diagnosis of this condition
Resources
[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ 1.0 1.1 Bhosale A, Fonseca M, Nandanwar YS. Obstructed Labour Due to Contracted Pelvis in a Grand Multiparous Woman. Bombay Hospital Journal. 2010;52(1):139.
- ↑ 2.0 2.1 Amiel GJ. Contracted pelvis and disproportion. InEssential Obstetric Practice 1981 (pp. 167-175). Dordrecht: Springer Netherlands.
- ↑ 3.0 3.1 3.2 Salk I, Cetin M, Salk S, Cetin A. Determining the incidence of gynecoid pelvis using three-dimensional computed tomography in nonpregnant multiparous women. Medical Principles and Practice. 2016;25(1):40-8.
- ↑ 4.0 4.1 Lewis CL, Laudicina NM, Khuu A, Loverro KL. The human pelvis: variation in structure and function during gait. The Anatomical Record. 2017 Apr;300(4):633-42.
- ↑ 5.0 5.1 Siccardi MA, Imonugo O, Valle C. Anatomy, Abdomen and Pelvis, Pelvic Inlet.
- ↑ Caldwell WE, Moloy HC. Anatomical variations in the female pelvis and their effect in labor with a suggested classification. American Journal of Obstetrics and Gynecology. 1933 Oct 1;26(4):479-505.
- ↑ Human Anatomy Education. Female bony pelvis: 3-Pelvimetry. Available from: http://www.youtube.com/watch?v=kTwxNTFP-YA [last accessed 21/2/2023]