Autonomic Dysreflexia: Difference between revisions
No edit summary |
No edit summary |
||
| Line 6: | Line 6: | ||
== Introduction == | == Introduction == | ||
Autonomic dysreflexia is a condition that emerges soon after a [[Spinal Cord Injury]], usually when the damage has occurred at or above the T6 level. It is generally defined as a syndrome in susceptible Spinal Cord injured patients that incorporates a sudden, exaggerated reflexive increase in blood pressure in response to a stimulus, usually bladder or bowel distension, originating below the level of the neurological injury. It is also sometimes known as autonomic hyperreflexia, hypertensive autonomic crisis, sympathetic hyperreflexia, autonomic [[Spasticity]], paroxysmal hypertension, mass reflex, and viscero-autonomic stress syndrome. | Autonomic dysreflexia is a condition that emerges soon after a [[Spinal Cord Injury]], usually when the damage has occurred at or above the T6 level. It is generally defined as a syndrome in susceptible Spinal Cord injured patients that incorporates a sudden, exaggerated reflexive increase in blood pressure in response to a stimulus, usually bladder or bowel distension, originating below the level of the neurological injury. It is also sometimes known as autonomic hyperreflexia, hypertensive autonomic crisis, sympathetic hyperreflexia, autonomic [[Spasticity]], paroxysmal hypertension, mass reflex, and viscero-autonomic stress syndrome<ref name=":0">Allen KJ, Leslie SW. [https://pubmed.ncbi.nlm.nih.gov/29494041/ Autonomic dysreflexia]. InStatPearls [Internet] 2022 Feb 14. StatPearls publishing.</ref>. [[Guillain-Barre Syndrome|Guillain–Barré Syndrome]] may also cause autonomic dysreflexia<ref>Autonomic Dysreflexia https://medlineplus.gov/ency/article/001431.htm</ref>. | ||
Dysregulation of the [[Autonomic Nervous System]] leads to an uncoordinated sympathetic response that may result in a potentially life-threatening hypertensive episode when there is a noxious stimulus below the level of the spinal cord injury. It is usually accompanied by a severe headache, bradycardia, and facial flushing, along with pallor, cold skin, and sweating in the lower part of the body. It is significant because it is a potentially lethal disorder that occurs in about half or more of the potentially susceptible individuals but can usually be easily alleviated by prompt recognition and relatively simple corrective procedures by caregivers<ref>Cowan H, Lakra C, Desai M. [https://pubmed.ncbi.nlm.nih.gov/33008797/ Autonomic dysreflexia in spinal cord injury]. bmj. 2020 Oct 2;371.</ref>. | |||
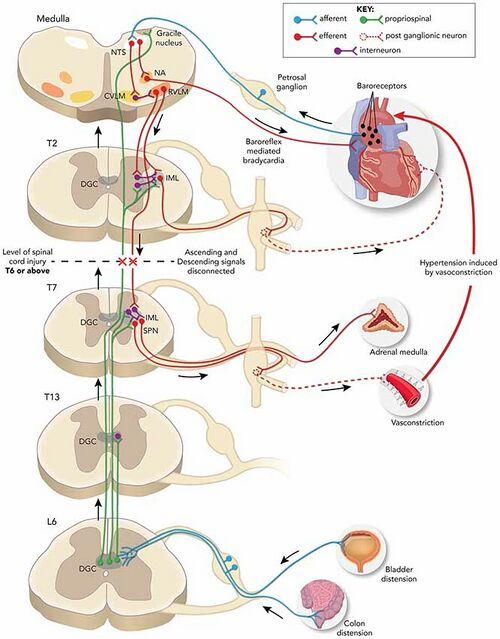
== Pathophysiology == | |||
[[File:AutoDys2019.jpeg|center|thumb|639x639px|Autonomic Dysreflexia]] | [[File:AutoDys2019.jpeg|center|thumb|639x639px|Autonomic Dysreflexia]] | ||
== Etiology == | == Etiology == | ||
The etiology is a spinal cord injury, almost always at or above the T6 level. Objectively, an episode is defined as an increase in systolic blood pressure of at least 25 mm Hg or more above baseline<ref name=":1">[https://pubmed.ncbi.nlm.nih.gov/34353860/ Lakra] C, Swayne O, Christofi G, Desai M. [https://pubmed.ncbi.nlm.nih.gov/34353860/ Autonomic dysreflexia in spinal cord injury. Practical neurology.] 2021 Dec 1;21(6):532-8.</ref>. A significant episode would usually have a systolic blood pressure of at least 150 mmHg or more than 40mmHg above the patient's baseline. The higher the injury level, the greater the severity of the cardiovascular dysfunction. The severity and frequency of autonomic dysreflexia episodes are also associated with the completeness of the spinal cord injury as well as the level. Patients with a complete spinal cord injury are more than three times more likely to develop autonomic dysreflexia than those with incomplete injuries (91% to 27%)<ref>Del Fabro AS, Mejia M, Nemunaitis G. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5810793/ An investigation of the relationship between autonomic dysreflexia and intrathecal baclofen in patients with spinal cord injury.] The journal of spinal cord medicine. 2018 Jan 2;41(1):102-5. | |||
BibTeXEndNoteRefManRefWorks</ref>. | |||
Although autonomic dysreflexia has been described in the first days or weeks after the original trauma, it generally does not develop until after the period of spinal shock when reflexes have recovered<ref name=":1" />. The earliest reported case appeared on the fourth-day post-injury. Most of the patients (92%) who will ultimately develop autonomic dysreflexia will do so within the first year after their injury. | |||
== Clinical Presentation == | == Clinical Presentation == | ||
Acute autonomic dysreflexia is characterised by severe Paroxysmal [[Hypertension]] associated with throbbing [[Headaches and Dizziness|Headaches]], profuse sweating, nasal stuffiness, Piloerection above the level of injury, flushing of the skin above the level of the lesion, [[bradycardia]],cool, pale skin below the level of injury because of severe vasoconstriction, visual disturbances, dizziness and anxiety or feeling of doom, which is sometimes accompanied by cognitive impairment<ref name=":2">Khastgir J, Drake MJ, Abrams P. [https://pubmed.ncbi.nlm.nih.gov/17472540/ Recognition and effective management of autonomic dysreflexia in spinal cord injuries. Expert opinion on pharmacotherapy.] 2007 May 1;8(7):945-56.</ref><ref name=":0" /><ref name=":1" />. | |||
The initial presenting symptom is typically a severe [[headache]]. The headache is usually sudden, severe, throbbing, and bilateral. It may be frontal, temporal, or occipital. This is caused by significant vasodilation superior to the level of injury. When this cerebral vasodilation is combined with dangerously high blood pressure, a potentially lethal stroke may occur. Symptoms may not necessarily correlate with the severity of the blood pressure elevation<ref name=":0" />. | |||
[[Hypertension]] may be asymptomatic or severe enough to cause a hypertensive crisis complicated by pulmonary edema, left ventricular dysfunction, retinal detachment, intracranial hemorrhage, seizures, or death. Patients with T6 level injuries tend to have systolic blood pressures between 90 and 110 mmHg, but readings should be compared with the patient's usual baseline levels. [[Bradycardia]] may also range from minor to resulting in cardiac arrest. Tachycardia is less common than bradycardia but may also occur along with cardiac arrhythmias and atrial fibrillation or flutter. If the patient has coronary artery disease, an episode of autonomic dysreflexia may cause a myocardial infarction<ref name=":1" />. | |||
'''Any patient with [[paraplegia]] or quadriplegia who complains of a severe [[headache]] or is found unconscious should immediately undergo screening for possible autonomic dysreflexia by checking their blood pressure and comparing it to their baseline level. Systolic blood pressure >150 mmHg or >40 mmHg above baseline should be considered highly suggestive of autonomic dysreflexia and appropriate measures should be taken'''<ref name=":0" />'''.''' | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
The initial presenting complaint is usually a severe headache, typically described as throbbing. Susceptible individuals, usually with spinal cord lesions at or above T6, who complain of a severe headache should immediately have their blood pressure checked. If elevated, a presumptive diagnosis of autonomic dysreflexia can be made.[5] Prompt recognition and correction of the disorder, usually just by irrigating or changing their urinary Foley catheter, can be immediately life-saving. Unfortunately, the vast majority of nurses, emergency room staff, and physiotherapists are unfamiliar with autonomic dysreflexia and are unable to identify or treat it quickly<ref>Kaydok E. [https://pubmed.ncbi.nlm.nih.gov/34855570/ Nurses and physiotherapists’ knowledge levels on autonomic dysreflexia in a rehabilitation hospital.] The journal of spinal cord medicine. 2021 Dec 3:1-5.</ref><ref>Tederko P, Ugniewski K, Bobecka-Wesołowska K, Tarnacka B. [https://pubmed.ncbi.nlm.nih.gov/31403393/ What do physiotherapists and physiotherapy students know about autonomic dysreflexia?. The journal of spinal cord medicine.] 2021 May 4;44(3):418-24.</ref>. This is quite problematic as they are often the first healthcare professionals to witness such an event where early recognition and immediate, proper treatment can literally be the difference between life and death<ref name=":1" />. | |||
Fortunately, most episodes are relatively mild and can be managed at home by the patient and their usual caregivers without acute medical intervention. Severe, life-threatening episodes are rarely encountered by most medical personnel except those who work in specialized tertiary care centers. This means that many medical professionals, even emergency personnel, may rarely see this condition acutely in its most severe form and may therefore not be familiar with its early recognition or immediate treatment protocol<ref name=":2" />. | |||
== Epidemiology == | |||
Autonomic dysreflexia develops in 48% to 70% of patients with a spinal cord injury above the T6 level and is quite unlikely to develop if the injury is below T10<ref>Karlsson AK. [https://pubmed.ncbi.nlm.nih.gov/10432257/ Autonomic dysreflexia. Spinal cord]. 1999 Jun;37(6):383-91.</ref>. It has also been infrequently reported in non-traumatic spinal cord injury cases, such as radiation myelopathy and cisplatin-induced polyneuropathy<ref>Saito H. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7426937/ Autonomic dysreflexia in a case of radiation myelopathy and cisplatin-induced polyneuropathy. Spinal cord series and cases]. 2020 Aug 13;6(1):1-5.</ref>.[13] | |||
Patients prone to this disorder will usually have a documented or personal history of prior episodes, but health professionals need to be alert to an initial presentation without any known prior history of autonomic dysreflexia<ref name=":1" />. | |||
== Diagnosis == | |||
The evaluation includes obtaining a history of previous autonomic dysreflexia episodes with the triggering event if known, monitoring vital signs, and watching for any developing signs and symptoms. The baseline blood pressure should be known and documented for future reference. Many patients with spinal cord injuries will have hypotension. Orthostatic hypotension is found in over 50% of patients with autonomic dysreflexia<ref>Gibbons CH, Freeman R. [https://pubmed.ncbi.nlm.nih.gov/16832073/ Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology.] 2006 Jul 11;67(1):28-32.</ref>. | |||
Start by identifying patients at risk (spinal cord injury at or above the T6 level) and recognize the key initial symptom, which is usually a severe headache from cerebral vasodilation. Should this be encountered, the next step would be to check the blood pressure. If elevated above the patient's usual baseline, then the patient is at high risk for an episode of autonomic dysreflexia. A systolic blood pressure >150 mmHg or >40 mmHg above baseline levels should be considered indicative of autonomic dysreflexia. | |||
The likelihood of autonomic dysreflexia is independently predicted by the level of the spinal cord lesion, whether it is complete or incomplete, and the presence of neurogenic detrusor overactivity<ref name=":0" />. | |||
== Differential Diagnosis == | |||
* Acute glomerulonephritis | |||
* Anxiety | |||
* Cushing's syndrome | |||
* Drug use or overdose (e.g., stimulants, especially alcohol, cocaine, or levothyroxine) | |||
* Hyperaldosteronism | |||
* Hyperthyroidism | |||
* Intracranial hemorrhage | |||
* Ischemic [[stroke]] | |||
* Nephritic and nephrotic syndrome | |||
* Polycystic kidney disease | |||
== Resources == | == Resources == | ||
Revision as of 15:25, 24 April 2022
Top Contributors -
Introduction[edit | edit source]
Autonomic dysreflexia is a condition that emerges soon after a Spinal Cord Injury, usually when the damage has occurred at or above the T6 level. It is generally defined as a syndrome in susceptible Spinal Cord injured patients that incorporates a sudden, exaggerated reflexive increase in blood pressure in response to a stimulus, usually bladder or bowel distension, originating below the level of the neurological injury. It is also sometimes known as autonomic hyperreflexia, hypertensive autonomic crisis, sympathetic hyperreflexia, autonomic Spasticity, paroxysmal hypertension, mass reflex, and viscero-autonomic stress syndrome[1]. Guillain–Barré Syndrome may also cause autonomic dysreflexia[2].
Dysregulation of the Autonomic Nervous System leads to an uncoordinated sympathetic response that may result in a potentially life-threatening hypertensive episode when there is a noxious stimulus below the level of the spinal cord injury. It is usually accompanied by a severe headache, bradycardia, and facial flushing, along with pallor, cold skin, and sweating in the lower part of the body. It is significant because it is a potentially lethal disorder that occurs in about half or more of the potentially susceptible individuals but can usually be easily alleviated by prompt recognition and relatively simple corrective procedures by caregivers[3].
Pathophysiology[edit | edit source]
Etiology[edit | edit source]
The etiology is a spinal cord injury, almost always at or above the T6 level. Objectively, an episode is defined as an increase in systolic blood pressure of at least 25 mm Hg or more above baseline[4]. A significant episode would usually have a systolic blood pressure of at least 150 mmHg or more than 40mmHg above the patient's baseline. The higher the injury level, the greater the severity of the cardiovascular dysfunction. The severity and frequency of autonomic dysreflexia episodes are also associated with the completeness of the spinal cord injury as well as the level. Patients with a complete spinal cord injury are more than three times more likely to develop autonomic dysreflexia than those with incomplete injuries (91% to 27%)[5].
Although autonomic dysreflexia has been described in the first days or weeks after the original trauma, it generally does not develop until after the period of spinal shock when reflexes have recovered[4]. The earliest reported case appeared on the fourth-day post-injury. Most of the patients (92%) who will ultimately develop autonomic dysreflexia will do so within the first year after their injury.
Clinical Presentation[edit | edit source]
Acute autonomic dysreflexia is characterised by severe Paroxysmal Hypertension associated with throbbing Headaches, profuse sweating, nasal stuffiness, Piloerection above the level of injury, flushing of the skin above the level of the lesion, bradycardia,cool, pale skin below the level of injury because of severe vasoconstriction, visual disturbances, dizziness and anxiety or feeling of doom, which is sometimes accompanied by cognitive impairment[6][1][4].
The initial presenting symptom is typically a severe headache. The headache is usually sudden, severe, throbbing, and bilateral. It may be frontal, temporal, or occipital. This is caused by significant vasodilation superior to the level of injury. When this cerebral vasodilation is combined with dangerously high blood pressure, a potentially lethal stroke may occur. Symptoms may not necessarily correlate with the severity of the blood pressure elevation[1].
Hypertension may be asymptomatic or severe enough to cause a hypertensive crisis complicated by pulmonary edema, left ventricular dysfunction, retinal detachment, intracranial hemorrhage, seizures, or death. Patients with T6 level injuries tend to have systolic blood pressures between 90 and 110 mmHg, but readings should be compared with the patient's usual baseline levels. Bradycardia may also range from minor to resulting in cardiac arrest. Tachycardia is less common than bradycardia but may also occur along with cardiac arrhythmias and atrial fibrillation or flutter. If the patient has coronary artery disease, an episode of autonomic dysreflexia may cause a myocardial infarction[4].
Any patient with paraplegia or quadriplegia who complains of a severe headache or is found unconscious should immediately undergo screening for possible autonomic dysreflexia by checking their blood pressure and comparing it to their baseline level. Systolic blood pressure >150 mmHg or >40 mmHg above baseline should be considered highly suggestive of autonomic dysreflexia and appropriate measures should be taken[1].
Diagnostic Procedures[edit | edit source]
The initial presenting complaint is usually a severe headache, typically described as throbbing. Susceptible individuals, usually with spinal cord lesions at or above T6, who complain of a severe headache should immediately have their blood pressure checked. If elevated, a presumptive diagnosis of autonomic dysreflexia can be made.[5] Prompt recognition and correction of the disorder, usually just by irrigating or changing their urinary Foley catheter, can be immediately life-saving. Unfortunately, the vast majority of nurses, emergency room staff, and physiotherapists are unfamiliar with autonomic dysreflexia and are unable to identify or treat it quickly[7][8]. This is quite problematic as they are often the first healthcare professionals to witness such an event where early recognition and immediate, proper treatment can literally be the difference between life and death[4].
Fortunately, most episodes are relatively mild and can be managed at home by the patient and their usual caregivers without acute medical intervention. Severe, life-threatening episodes are rarely encountered by most medical personnel except those who work in specialized tertiary care centers. This means that many medical professionals, even emergency personnel, may rarely see this condition acutely in its most severe form and may therefore not be familiar with its early recognition or immediate treatment protocol[6].
Epidemiology[edit | edit source]
Autonomic dysreflexia develops in 48% to 70% of patients with a spinal cord injury above the T6 level and is quite unlikely to develop if the injury is below T10[9]. It has also been infrequently reported in non-traumatic spinal cord injury cases, such as radiation myelopathy and cisplatin-induced polyneuropathy[10].[13]
Patients prone to this disorder will usually have a documented or personal history of prior episodes, but health professionals need to be alert to an initial presentation without any known prior history of autonomic dysreflexia[4].
Diagnosis[edit | edit source]
The evaluation includes obtaining a history of previous autonomic dysreflexia episodes with the triggering event if known, monitoring vital signs, and watching for any developing signs and symptoms. The baseline blood pressure should be known and documented for future reference. Many patients with spinal cord injuries will have hypotension. Orthostatic hypotension is found in over 50% of patients with autonomic dysreflexia[11].
Start by identifying patients at risk (spinal cord injury at or above the T6 level) and recognize the key initial symptom, which is usually a severe headache from cerebral vasodilation. Should this be encountered, the next step would be to check the blood pressure. If elevated above the patient's usual baseline, then the patient is at high risk for an episode of autonomic dysreflexia. A systolic blood pressure >150 mmHg or >40 mmHg above baseline levels should be considered indicative of autonomic dysreflexia.
The likelihood of autonomic dysreflexia is independently predicted by the level of the spinal cord lesion, whether it is complete or incomplete, and the presence of neurogenic detrusor overactivity[1].
Differential Diagnosis[edit | edit source]
- Acute glomerulonephritis
- Anxiety
- Cushing's syndrome
- Drug use or overdose (e.g., stimulants, especially alcohol, cocaine, or levothyroxine)
- Hyperaldosteronism
- Hyperthyroidism
- Intracranial hemorrhage
- Ischemic stroke
- Nephritic and nephrotic syndrome
- Polycystic kidney disease
Resources[edit | edit source]
add appropriate resources here
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Allen KJ, Leslie SW. Autonomic dysreflexia. InStatPearls [Internet] 2022 Feb 14. StatPearls publishing.
- ↑ Autonomic Dysreflexia https://medlineplus.gov/ency/article/001431.htm
- ↑ Cowan H, Lakra C, Desai M. Autonomic dysreflexia in spinal cord injury. bmj. 2020 Oct 2;371.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Lakra C, Swayne O, Christofi G, Desai M. Autonomic dysreflexia in spinal cord injury. Practical neurology. 2021 Dec 1;21(6):532-8.
- ↑ Del Fabro AS, Mejia M, Nemunaitis G. An investigation of the relationship between autonomic dysreflexia and intrathecal baclofen in patients with spinal cord injury. The journal of spinal cord medicine. 2018 Jan 2;41(1):102-5. BibTeXEndNoteRefManRefWorks
- ↑ 6.0 6.1 Khastgir J, Drake MJ, Abrams P. Recognition and effective management of autonomic dysreflexia in spinal cord injuries. Expert opinion on pharmacotherapy. 2007 May 1;8(7):945-56.
- ↑ Kaydok E. Nurses and physiotherapists’ knowledge levels on autonomic dysreflexia in a rehabilitation hospital. The journal of spinal cord medicine. 2021 Dec 3:1-5.
- ↑ Tederko P, Ugniewski K, Bobecka-Wesołowska K, Tarnacka B. What do physiotherapists and physiotherapy students know about autonomic dysreflexia?. The journal of spinal cord medicine. 2021 May 4;44(3):418-24.
- ↑ Karlsson AK. Autonomic dysreflexia. Spinal cord. 1999 Jun;37(6):383-91.
- ↑ Saito H. Autonomic dysreflexia in a case of radiation myelopathy and cisplatin-induced polyneuropathy. Spinal cord series and cases. 2020 Aug 13;6(1):1-5.
- ↑ Gibbons CH, Freeman R. Delayed orthostatic hypotension: a frequent cause of orthostatic intolerance. Neurology. 2006 Jul 11;67(1):28-32.