Mindfulness Meditation in Chronic Pain Management: Difference between revisions
No edit summary |
No edit summary |
||
| Line 8: | Line 8: | ||
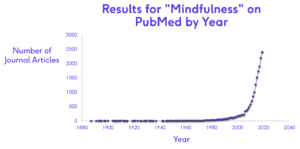
Evidence for the use of mindfulness has grown rapidly since its introduction to the Western world around 1979, with more than 2500 studies currently available on mindfulness (Figure 1). | Evidence for the use of mindfulness has grown rapidly since its introduction to the Western world around 1979, with more than 2500 studies currently available on mindfulness (Figure 1). | ||
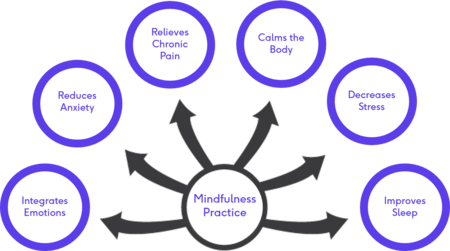
Mindfulness-Based Interventions (MBI) are showing promising results in supporting mental health needs even in the absence of psychological disorders and have become a more popular, cost-effective method to provide the support.<ref>Dunning D.L., Griffiths K., Kuyken W., Crane C., Foulkes L., Parker J., Dalgleish T. [https://acamh.onlinelibrary.wiley.com/doi/pdf/10.1111/jcpp.12980 Research Review: The effects of mindfulness‐based interventions on cognition and mental health in children and adolescents–a meta‐analysis of randomized controlled trials]. Journal of Child Psychology and Psychiatry. 2019; 60(3), pp.244-258. DOI:10.1111/jcpp.12980 </ref><ref>Nunes A, Castro SL, Limpo T. [https://sci-hub.se/https://link.springer.com/article/10.1007/s12671-020-01410-w?wt_mc=Internal.Event.1.SEM.ArticleAuthorOnlineFirst&utm_source=ArticleAuthorOnlineFirst&utm_medium=email&utm_content=AA_en_06082018&ArticleAuthorOnlineFirst_20200524 A review of mindfulness-based apps for children]. Mindfulness. 2020 Sep;11(9):2089-101. DOI:10.1007/s12671-020-01410-w </ref> The benefits of MBI are well established and include:<ref>Spinelli C, Wisener M, Khoury B. [https://sci-hub.se/https://pubmed.ncbi.nlm.nih.gov/30929705/ Mindfulness training for healthcare professionals and trainees: A meta-analysis of randomized controlled trials]. Journal of Psychosomatic Research. 2019 May 1;120:29-38. DOI:10.1016/j.jpsychores.2019.03.003 </ref><ref>Marusak HA, Elrahal F, Peters CA, Kundu P, Lombardo MV, Calhoun VD, Goldberg EK, Cohen C, Taub JW, Rabinak CA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5610942/pdf/nihms905400.pdf Mindfulness and dynamic functional neural connectivity in children and adolescents]. Behavioural brain research. 2018 Jan 15;336:211-8. DOI:10.1016/j.bbr.2017.09.010 </ref><ref>Geronimi EM, Arellano B, Woodruff-Borden J. [https://sci-hub.se/https://journals.sagepub.com/doi/abs/10.1177/1359104519833737 Relating mindfulness and executive function in children]. Clinical child psychology and psychiatry. 2020 Apr;25(2):435-45. DOI:10.1177/135910451983373 </ref><ref>Zeidan F, Baumgartner JN, Coghill RC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6728003/pdf/painreports-4-e759.pdf The neural mechanisms of mindfulness-based pain relief: a functional magnetic resonance imaging-based review and primer.] Pain reports. 2019 Jul;4(4). DOI:10.1097/PR9.0000000000000759 </ref> | Mindfulness-Based Interventions (MBI) are showing promising results in supporting mental health needs even in the absence of psychological disorders and have become a more popular, cost-effective method to provide the support.<ref>Dunning D.L., Griffiths K., Kuyken W., Crane C., Foulkes L., Parker J., Dalgleish T. [https://acamh.onlinelibrary.wiley.com/doi/pdf/10.1111/jcpp.12980 Research Review: The effects of mindfulness‐based interventions on cognition and mental health in children and adolescents–a meta‐analysis of randomized controlled trials]. Journal of Child Psychology and Psychiatry. 2019; 60(3), pp.244-258. DOI:10.1111/jcpp.12980 </ref><ref>Nunes A, Castro SL, Limpo T. [https://sci-hub.se/https://link.springer.com/article/10.1007/s12671-020-01410-w?wt_mc=Internal.Event.1.SEM.ArticleAuthorOnlineFirst&utm_source=ArticleAuthorOnlineFirst&utm_medium=email&utm_content=AA_en_06082018&ArticleAuthorOnlineFirst_20200524 A review of mindfulness-based apps for children]. Mindfulness. 2020 Sep;11(9):2089-101. DOI:10.1007/s12671-020-01410-w </ref> The benefits of MBI are well established and include:<ref>Spinelli C, Wisener M, Khoury B. [https://sci-hub.se/https://pubmed.ncbi.nlm.nih.gov/30929705/ Mindfulness training for healthcare professionals and trainees: A meta-analysis of randomized controlled trials]. Journal of Psychosomatic Research. 2019 May 1;120:29-38. DOI:10.1016/j.jpsychores.2019.03.003 </ref><ref>Marusak HA, Elrahal F, Peters CA, Kundu P, Lombardo MV, Calhoun VD, Goldberg EK, Cohen C, Taub JW, Rabinak CA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5610942/pdf/nihms905400.pdf Mindfulness and dynamic functional neural connectivity in children and adolescents]. Behavioural brain research. 2018 Jan 15;336:211-8. DOI:10.1016/j.bbr.2017.09.010 </ref><ref>Geronimi EM, Arellano B, Woodruff-Borden J. [https://sci-hub.se/https://journals.sagepub.com/doi/abs/10.1177/1359104519833737 Relating mindfulness and executive function in children]. Clinical child psychology and psychiatry. 2020 Apr;25(2):435-45. DOI:10.1177/135910451983373 </ref><ref name=":0">Zeidan F, Baumgartner JN, Coghill RC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6728003/pdf/painreports-4-e759.pdf The neural mechanisms of mindfulness-based pain relief: a functional magnetic resonance imaging-based review and primer.] Pain reports. 2019 Jul;4(4). DOI:10.1097/PR9.0000000000000759 </ref> | ||
* Decreased anxiety and depression | * Decreased anxiety and depression | ||
* Relieve of stress and psychological distress | * Relieve of stress and psychological distress | ||
| Line 22: | Line 22: | ||
== Cognitive Changes associated with Mindfulness == | == Cognitive Changes associated with Mindfulness == | ||
The greatest impact of mindfulness is its effect on the neural plasticity of the brain. Several changes in brain activation has been documented with the practice of mindfulness, allowing us to also “see” the benefits of MBI as is evident on functional Magnetic Resonance Imaging (fMRI) | The greatest impact of mindfulness is its effect on the neural plasticity of the brain. Several changes in brain activation has been documented with the practice of mindfulness, allowing us to also “see” the benefits of MBI as is evident on functional Magnetic Resonance Imaging (fMRI).<ref name=":1">Tang YY, Hölzel BK, Posner MI. [https://www.researchgate.net/profile/Britta_Holzel/publication/273774412_The_neuroscience_of_mindfulness_meditation/links/550ca4970cf27526109679f3/The-neuroscience-of-mindfulness-meditation.pdf The neuroscience of mindfulness meditation]. Nature Reviews Neuroscience. 2015 Apr;16(4):213-25. DOI:10.1038/nrn3916 </ref><ref>Bauer CC, Caballero C, Scherer E, West MR, Mrazek MD, Phillips DT, Whitfield-Gabrieli S, Gabrieli JD. Mindfulness training reduces stress and amygdala reactivity to fearful faces in middle-school children. Behavioral Neuroscience. 2019 Dec;133(6):569. DOI:10.1037/bne0000337</ref> However, the study designs vary greatly with the use of different MBI and therefore the locations of the reported effects are diverse and spread over multiple regions of the brain.<ref name=":1" /> The brain regions most consistently altered with MBI are included in Table 1.<ref name=":1" /><ref>Young KS, van der Velden AM, Craske MG, Pallesen KJ, Fjorback L, Roepstorff A, Parsons CE. [https://mindfulness.au.dk/fileadmin/mindfulness.au.dk/Artikler/Young_et_al_2017_The_impact...pdf The impact of mindfulness-based interventions on brain activity: A systematic review of functional magnetic resonance imaging studies]. Neuroscience & Biobehavioral Reviews. 2018 Jan 1;84:424-33. DOI: 10.1016/j.neubiorev.2017.08.003 </ref><ref name=":2">Gotink RA, Meijboom R, Vernooij MW, Smits M, Hunink MM. [http://www.teradanismanlik.com/resim/upload/141f.pdf 8-week mindfulness based stress reduction induces brain changes similar to traditional long-term meditation practice–a systematic review]. Brain and cognition. 2016 Oct 1;108:32-41. DOI:10.1016/j.bandc.2016.07.001 </ref><ref>Zimmerman B, Finnegan M, Paul S, Schmidt S, Tai Y, Roth K, Chen Y, Husain FT. [https://www.frontiersin.org/articles/10.3389/fnins.2019.00747/full Functional brain changes during mindfulness-based cognitive therapy associated with tinnitus severity]. Frontiers in neuroscience. 2019 Jul 24;13:747. DOI:10.3389/fnins.2019.00747 </ref> | ||
Table 1: Neural changes associated with mindfulness practice | '''Table 1:''' Neural changes associated with mindfulness practice | ||
{| class="wikitable" | {| class="wikitable" | ||
|Region of the brain | |Region of the brain | ||
| Line 85: | Line 85: | ||
|} | |} | ||
Greater stress is associated with greater amygdala activation. Down-regulation of the amygdala is what underscores the reduction in stress seen with MBSR | Greater stress is associated with greater amygdala activation. Down-regulation of the amygdala is what underscores the reduction in stress seen with Mindfulness-Based Stress Reduction (MBSR).<ref name=":2" /> Mindfulness is therefore not simply about paying attention. The way in which we use this focus of the mind ultimately changes the function and the structure of the brain.<ref>Siegel DJ. [https://watermark.silverchair.com/nsm034.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAp0wggKZBgkqhkiG9w0BBwagggKKMIIChgIBADCCAn8GCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQMbISSiq4dS3manEbUAgEQgIICUHRiv5gnzsGXA0UG2n8Qpzyh1JHay5CJyUFxfPxMox0j-acapPGov2uIDlUp1SlUBwRs3IJmW_Vz2tRzZEMKSMp3TRVxSHB1eLe1dwYzkrsw1RzPvHHPc6CJeRNs3bkauP5IuqddmKcEG9rgR01SvIM_lhL9TSSQ6uRzwhY9SWtk0t2rqh8VccK80IsW0ipGEBpPBs85N-FcoxgOjstjDcDtWi_P1eslnrzzZMiptApkiUoqZBxtXLckcKrn7Cn68K_DWkndZK1B0M78RVNSwApPxOZ5HB9wCewZH3C_48Rge6d5vxjO_NgvEo3kny_d-izNfU_7zZgeijQKvSlJOp__rKZ221KII6uODYMjpV-M-IAkrj2R99zNXCsw49eEMKTxsjhd-sCL3RV-OYSkYAfQLJq2LwAZ4k4NPph2jJ3IiwaOtCG5aEXlI19gAQZhhqsQQVwzTKAxbzQ7yaPgS63aD9KfqjUetLOwvNCu9lCtYqxc4jruA4lOxXXQlTjPKet7fNp-XasJDq2zsn20FRzDJRX60OZz50bQ7wrbtng6JoUuYwxQD2hj-i4O8lZ_Rh8v8P-gXsMT4JV2uZaLTUH7f1jlChiaefbz8YmKepkLVp-6pBJxOoIPdSFxnmOmkuAR2-kYrXVvqIIXr-6z701MhiHuZhdbY_Z3mKnASV9XROFX2cInxuVAgIx0I6x8wJ9tEO_BpOFr6oltzQ1YQ3RO30H8Lm_3ZFEMRX-aHjHuHjcZAy3NsJ7vG_zdYc1XtVDmQmz_fxng3jBWyHg2_Sk Mindfulness training and neural integration: Differentiation of distinct streams of awareness and the cultivation of well-being]. Social cognitive and affective neuroscience. 2007 Dec 1;2(4):259-63. DOI:10.1093/scan/nsm034 </ref> Just as we can train our muscles to grow, we can “train” our brains as is evident in the studies about mindfulness. | ||
== Mindfulness and Pain == | == Mindfulness and Pain == | ||
Chronic pain poses a significant therapeutic challenge and has been declared a public health problem, placing burdens not only on those experiencing pain, but also society as a whole ( | Chronic pain poses a significant therapeutic challenge and has been declared a public health problem, placing burdens not only on those experiencing pain, but also society as a whole.<ref name=":3">Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD. [https://www.jpain.org/action/showPdf?pii=S1526-5900%2816%2900018-3 The role of psychosocial processes in the development and maintenance of chronic pain]. The Journal of Pain. 2016 Sep 1;17(9): T70-92. DOI:10.1016/j.jpain.2016.01.001 </ref><ref name=":4">Smith SL, Langen WH. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7735497/ A systematic review of mindfulness practices for improving outcomes in chronic low back pain]. International Journal of Yoga. 2020 Sep;13(3):177. DOI:10.4103/ijoy.IJOY_4_20 </ref> Chronic pain is estimated to affect more than 100 million adults at any given time in the United States, with chronic back pain being the most commonly reported chronic pain complaint.<ref name=":0" /><ref name=":3" /><ref name=":4" /><ref name=":5">McClintock AS, McCarrick SM, Garland EL, Zeidan F, Zgierska AE. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6437625/pdf/acm.2018.0351.pdf Brief mindfulness-based interventions for acute and chronic pain: A systematic review.] The Journal of Alternative and Complementary Medicine. 2019 Mar 1;25(3):265-78. DOI:10.1089/acm.2018.0351 </ref> Chronic pain is also one of the primary causes of disability and decreased quality of life, resulting in a cost of more than $600 billion dollars annually in the United States alone.<ref name=":3" /><ref name=":5" /> Opioid medication is frequently prescribed in order to manage pain and its potential consequences, which contributed to many other problems including the “opioid epidemic” of opioid misuse, addiction and opioid-related deaths due to patients overdosing.<ref name=":4" /><ref name=":5" /> Mindfulness, as a nonpharmacologic option, is receiving increased interest in the management of pain.<ref name=":0" /><ref name=":5" /><ref>Ngamkham S, Holden JE, Smith EL. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6371675/pdf/APJON-6-161.pdf A systematic review: mindfulness intervention for cancer-related pain]. Asia-Pacific journal of oncology nursing. 2019 Apr;6(2):161. DOI:10.4103/apjon.apjon_67_18 </ref> | ||
Chronic pain is complex in nature, involving many physical and psychological factors | Chronic pain is complex in nature, involving many physical and psychological factors.<ref name=":4" /><ref name=":6">Zeidan F, Emerson NM, Farris SR, Ray JN, Jung Y, McHaffie JG, Coghill RC. [https://www.jneurosci.org/content/jneuro/35/46/15307.full.pdf Mindfulness meditation-based pain relief employs different neural mechanisms than placebo and sham mindfulness meditation-induced analgesia]. Journal of Neuroscience. 2015 Nov 18;35(46):15307-25. DOI:10.1523/JNEUROLSCI.2542-15.2015 </ref> It is associated with sleep disturbances, obesity and weight gain, chronic fatigue, limited physical functionality and decreased quality of life.<ref name=":4" /> Individuals suffering from a variety of chronically painful conditions are also at an increased risk for anxiety, depression and other affective disorders.<ref name=":3" /><ref name=":5" /><ref name=":7">Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Colaiaco B, Maher AR, Shanman RM, Sorbero ME, Maglione MA. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5368208/pdf/12160_2016_Article_9844.pdf Mindfulness meditation for chronic pain: systematic review and meta-analysis]. Annals of Behavioral Medicine. 2017 Apr 1;51(2):199-213. DOI:10.1007/s12160-016-9844-2 </ref> The International Association for the Study of Pain (IASP) defines pain as “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”<ref>International Association for the Study of Pain. [https://www.iasp-pain.org/terminology?navItemNumber=576 IASP Terminology.] Last Updated: December 14, 2017. [Accessed 29 March 2021]. </ref> Treatment of pain should therefore also be multifaceted to address both the sensory component as well as the affective/emotional experience of pain. Treatments targeted at the negative affect associated with chronic pain are therefore hypothesised to not only positively influence the emotional distress but also influence the frequency and intensity of pain.<ref name=":3" /> Mindfulness as a multifaceted intervention is therefore ideally placed to have a positive effect on pain and pain affect without the negative effects associated with pharmacological interventions such as opioids.<ref name=":0" /><ref name=":3" /><ref name=":5" /><ref name=":8">Elvery N, Jensen MP, Ehde DM, Day MA. [https://sci-hub.se/10.1097/AJP.0000000000000430 Pain catastrophizing, mindfulness, and pain acceptance]. The Clinical journal of pain. 2017 Jun 1;33(6):485-95. DOI:10.1097/AJP.0000000000000430 </ref> | ||
MBSR is consistently showing positive improvements in pain management | MBSR is consistently showing positive improvements in pain management.<ref name=":3" /><ref name=":4" /><ref name=":6" /> Several studies have looked at the effect of MBI on various chronic conditions and various chronically painful conditions including chronic low back pain (LBP).<ref name=":9">Niazi AK, Niazi SK. [https://sci-hub.se/10.4297/najms.2011.320 Mindfulness-based stress reduction: a non-pharmacological approach for chronic illnesses.] North American journal of medical sciences. 2011 Jan;3(1):20. DOI:10.4297/najms.2011.320 </ref> Several of these studies can be found in Table 2. | ||
Table 2. Studies on the effect of MBI | |||
'''Table 2'''. Studies on the effect of MBI | |||
{| class="wikitable" | {| class="wikitable" | ||
|Study | |Study | ||
| Line 101: | Line 102: | ||
|Results | |Results | ||
|- | |- | ||
|Niazi | |Niazi<ref name=":9" /> | ||
|2011 | |2011 | ||
|Systematic review | |Systematic review | ||
| Line 109: | Line 110: | ||
|Improvement in chronic conditions | |Improvement in chronic conditions | ||
|- | |- | ||
|Zeidan et al | |Zeidan et al<ref name=":10">Zeidan F, Martucci KT, Kraft RA, Gordon NS, McHaffie JG, Coghill RC. [https://sci-hub.se/10.1523/jneurosci.5791-10.2011 Brain mechanisms supporting the modulation of pain by mindfulness meditation]. J Neurosci. 2011 Apr 6;31(14):5540-8. DOI:10.1523/JNEUROSCI.5791-10.2011. </ref> | ||
|2011 | |2011 | ||
|15 participants | |15 participants | ||
| Line 117: | Line 118: | ||
Reduced pain unpleasantness (57%) | Reduced pain unpleasantness (57%) | ||
|- | |- | ||
|Zeidan et al | |Zeidan et al<ref name=":6" /> | ||
|2015 | |2015 | ||
|75 participants | |75 participants | ||
| Line 125: | Line 126: | ||
Reduced pain unpleasantness (44%) | Reduced pain unpleasantness (44%) | ||
|- | |- | ||
|Morone et al | |Morone et al<ref>Morone NE, Greco CM, Moore CG, Rollman BL, Lane B, Morrow LA, Glynn NW, Weiner DK. [http://jama.jamanetwork.com/article.aspx?doi=10.1001/jamainternmed.2015.8033&utm_campaign=articlePDF%26utm_medium=articlePDFlink%26utm_source=articlePDF%26utm_content=jamainternmed.2015.8033 A mind-body program for older adults with chronic low back pain: a randomized clinical trial]. JAMA internal medicine. 2016 Mar 1;176(3):329-37. DOI:10.1001/jamainternmed.2015.8033 </ref> | ||
|2016 | |2016 | ||
|282 participants with chronic LBP | |282 participants with chronic LBP | ||
| Line 131: | Line 132: | ||
|Significant improvements in disability and quality of life | |Significant improvements in disability and quality of life | ||
|- | |- | ||
|Cherkin et al | |Cherkin et al<ref>Cherkin, D.C., Sherman, K.J., Balderson, B.H., Cook, A.J., Anderson, M.L., Hawkes, R.J., Hansen, K.E. and Turner, J.A., 2016. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4914381/pdf/nihms781082.pdf Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial]. Jama, 315(12), pp.1240-1249. DOI:10.1001/jama.2016.2323. </ref> | ||
|2016 | |2016 | ||
|Randomised controlled trial | |Randomised controlled trial | ||
| Line 145: | Line 146: | ||
|MBST and CBT equivalent in reducing pain and improving function showing greater improvements compared to usual care | |MBST and CBT equivalent in reducing pain and improving function showing greater improvements compared to usual care | ||
|- | |- | ||
|Zgierska et al | |Zgierska et al<ref>Zgierska AE, Burzinski CA, Cox J, Kloke J, Stegner A, Cook DB, Singles J, Mirgain S, Coe CL, Bačkonja M. [https://watermark.silverchair.com/pnw006.pdf?token=AQECAHi208BE49Ooan9kkhW_Ercy7Dm3ZL_9Cf3qfKAc485ysgAAAq0wggKpBgkqhkiG9w0BBwagggKaMIIClgIBADCCAo8GCSqGSIb3DQEHATAeBglghkgBZQMEAS4wEQQMa7U0rfkE07zEWOB9AgEQgIICYObCiYqjXs3LQm1EETzMWO3SA3mCBziLZzvJ9TCGmeLenfV3eiB7aH2rSd9G82owZ99f_bA_EtSoNnslk-bu4MQMfzhZb74n4xbjVKNEJXO8ZNJWVGU8jif-SaOjNacEOc7H3R0xqJbXa9OLZf8Kt8m1oG8iNY1LAJA22rlUHoB_fUcx99FETdLQz-24ZuZ-DlwCMHNDDGPcz9xX42M0_twb5Rmk8ScT27gg0Ke9wLGjhaqrjmS6qmfjQjhOkHSGQ3j-mmcp0tK8ROsJnZbUHQMWVUrfs9dXDQZP_G5VBzRYU2CYnQ-au_mBAJwTOaLZhWuF13loCbhQIAv0LCooGVCGgHAglxzf0jQa4CZ1E9-OjIB99JNAreOXwoPkul2Sk84EPmukO8SRUmPuZsUbleNze5PtCjgz3CuQQVLzJOL60iyqgGP0ziUDLU3xp_wJ5yntkQcNYNlNGyVj1Y8XjL08v3pCo_aVmuj1OHy9A2ALd3yseLerVcEkEKSzBR1ODHnTlDPlHEZHyYsK02aDbclCIct1X2Z4zn2wkygZFac3MdEyTXWa34PNnoUa9TqqMwTxOmOn_gJwVd1-kZ9QlG-vS1MuzkyXEu8CLP76cF0yL1NAci60u7GbTzQkCYbwLHYk0xmp_jUYbnEcZ2x2uaIgW_A7lVAjyjj3vO6RWCEKMFOGUn8LvAwojT08VxWnlbhv__8v5R8BEzFJUZ3-M8b9RpMT2S28frYmV1XBRPcnuin3qbRVEZgHCPuZvWXRzFWKlC_Gx_6MKwlohNFj9olXvOQqBF2niFqc2GvGL_fe Mindfulness meditation and cognitive behavioral therapy intervention reduces pain severity and sensitivity in opioid-treated chronic low back pain: pilot findings from a randomized controlled trial]. Pain Medicine. 2016 Oct 1;17(10):1865-81. DOI: 10.1093/pm/pnw006 </ref> | ||
|2016 | |2016 | ||
|35 participants with chronic LBP | |35 participants with chronic LBP | ||
| Line 153: | Line 154: | ||
|Significant decrease in pain intensity (short and long-term) | |Significant decrease in pain intensity (short and long-term) | ||
|- | |- | ||
|Anheyer | |Anheyer et al<ref>Anheyer D, Haller H, Barth J, Lauche R, Dobos G, Cramer H. [https://sci-hub.se/10.7326/M16-1997 Mindfulness-based stress reduction for treating low back pain: a systematic review and meta-analysis.] Annals of internal medicine. 2017 Jun 6;166(11):799-807. DOI: 10.7326/m16-1997 </ref> | ||
|2017 | |2017 | ||
|Systematic review & Meta-analysis | |Systematic review & Meta-analysis | ||
| Line 161: | Line 162: | ||
|MBSR associated with short-term improvements in pain intensity and physical functioning | |MBSR associated with short-term improvements in pain intensity and physical functioning | ||
|- | |- | ||
|Banth & Ardebil | |Banth & Ardebil<ref name=":11">Banth S, Ardebil MD. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4479890/ Effectiveness of mindfulness meditation on pain and quality of life of patients with chronic low back pain]. International journal of yoga. 2015 Jul;8(2):128. DOI:10.4103/0973-6131.158476 </ref> | ||
|2018 | |2018 | ||
|88 patients with NSCLBP | |88 patients with NSCLBP | ||
| Line 167: | Line 168: | ||
|MBSR significant reduction in pain and improvement in physical and mental quality of life | |MBSR significant reduction in pain and improvement in physical and mental quality of life | ||
|- | |- | ||
|Smith & | |Smith & Langen<ref name=":4" /> | ||
|2020 | |2020 | ||
|Systematic review | |Systematic review | ||
| Line 177: | Line 178: | ||
|Improvement in pain scores and quality of life after mindfulness interventions | |Improvement in pain scores and quality of life after mindfulness interventions | ||
|- | |- | ||
|Qaseem et al | |Qaseem et al <ref>Qaseem A, Wilt TJ, McLean RM, Forciea MA. [https://www.acpjournals.org/doi/full/10.7326/M16-2367?journalCode=aim Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians]. Annals of internal medicine. 2017 Apr 4;166(7):514-30. DOI: 10.7326/M16-2367. </ref> | ||
|2017 | |2017 | ||
|Systematic review to establish practice guidelines | |Systematic review to establish practice guidelines | ||
| Line 184: | Line 185: | ||
|} | |} | ||
MBIs are suggested to have greater effects on pain-related catastrophizing, especially in the presence of high levels of pain intensity, compared to traditional cognitive behavioural therapy (CBT) approaches | MBIs are suggested to have greater effects on pain-related catastrophizing, especially in the presence of high levels of pain intensity, compared to traditional cognitive behavioural therapy (CBT) approaches.<ref name=":3" /><ref name=":8" /> In general, participants practicing mindfulness (especially MBSR) for chronic pain, displayed significantly improved outcomes of pain measures as well as quality of life and mental health measures compared to matched control groups.<ref name=":4" /> Patients with chronic pain who engaged in mindfulness practice were generally found to be able to find new ways of living with and accepting pain, resulting in a less negative impact on their daily lives.<ref name=":4" /> The need for methodologically sound studies on MBI for patients with chronic pain is however reiterated in many studies.<ref name=":7" /> | ||
== Mechanism of Pain Reduction through Mindfulness Practice == | == Mechanism of Pain Reduction through Mindfulness Practice == | ||
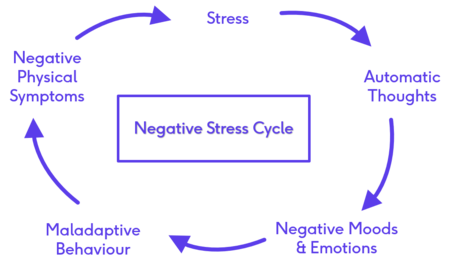
Exploring the mechanisms by which mindfulness influences stress and pain, necessitate an explanation of the negative stress cycle | Exploring the mechanisms by which mindfulness influences stress and pain, necessitate an explanation of the negative stress cycle that develops as a result of the long-term and unrelenting presence of stress and pain.<ref name=":12">Shrey Vazir. Mindful Meditation in Chronic Pain Management. Physioplus Course. 2021</ref> The negative stress cycle is set off by the occurrence of a stressful event which is often not relenting. The patient enters into a cycle of automatic thoughts about this event (the stress/pain) which leads to negative moods and emotions, ultimately resulting in maladaptive behaviours which often end up sustaining this cycle by worsening their symptoms (Figure 3).<ref name=":3" /><ref name=":12" /> | ||
[[File:Negative Stress Cycle .png|frameless|450x450px]] | [[File:Negative Stress Cycle .png|frameless|450x450px]] | ||
| Line 193: | Line 194: | ||
Figure 3. The Negative Stress Cycle | Figure 3. The Negative Stress Cycle | ||
The practice of mindfulness is able to break this cycle by interrupting the “automatic thoughts” stage achieved through turning off the autopilot mode of living and guiding the awareness back to the present moment with an attitude of non-judgement and non-reactance. | The practice of mindfulness is able to break this cycle by interrupting the “automatic thoughts” stage achieved through turning off the autopilot mode of living and guiding the awareness back to the present moment with an attitude of non-judgement and non-reactance.<ref name=":4" /><ref name=":12" /> MBSR proposes that mindfulness practice “will allow for the “uncoupling” of the bottom-up, afferent, sensory-driven components of pain from the top-down, psychological, cortically-driven components of pain”.<ref name=":4" /> This suggests that awareness can result in a dissociation between the physical sensation of pain from the emotions and thoughts previously attached to pain.<ref name=":4" /><ref name=":11" /> The goal of mindfulness, therefore, is not to eliminate the stress or pain, but to teach the patient self-awareness and alternate responses to stress and pain by embracing the pain, accepting the moment for what it is.<ref name=":4" /><ref name=":12" /> By making peace with the pain, the patient is able to better manage the pain with fewer negative coping responses (including fear and anxiety).<ref name=":4" /><ref name=":11" /><ref name=":12" /> | ||
Pain reduction through mindfulness meditation also utilises different neural mechanisms as compared to placebo analgesia | Pain reduction through mindfulness meditation also utilises different neural mechanisms as compared to placebo analgesia.<ref name=":6" /> Besides its proposed influence on pain affect, mindfulness-based pain relief also engages brain mechanisms involved in mediating the cognitive modulation of pain, which include:<ref name=":0" /><ref name=":5" /><ref name=":6" /><ref name=":10" /> | ||
* decreased activity in neural regions associated with low-level nociceptive processing (eg thalamus) | * decreased activity in neural regions associated with low-level nociceptive processing (eg thalamus) | ||
* Increased activity in neural regions associated with interoceptive awareness (eg right anterior insula) | * Increased activity in neural regions associated with interoceptive awareness (eg right anterior insula) | ||
* Top-down executive control (eg ACC) | * Top-down executive control (eg ACC) | ||
* Cognitive reappraisal of sensory information (eg orbitofrontal cortex) | * Cognitive reappraisal of sensory information (eg orbitofrontal cortex) | ||
The ultimate strength of mindfulness lies in the neural changes it causes. Keeping in mind that “nerves that fire together, wire together”, repetitive practice of mindfulness meditation leads to changes in neural pathways resulting in a more calm, accepting disposition towards life | The ultimate strength of mindfulness lies in the neural changes it causes. Keeping in mind that “nerves that fire together, wire together”, repetitive practice of mindfulness meditation leads to changes in neural pathways resulting in a more calm, accepting disposition towards life.<ref name=":12" /> | ||
Several studies have found that long-term meditation practice can lead to increased pain threshold values and lower pain sensitivity even while the practitioners are not engaged in mindfulness practice | Several studies have found that long-term meditation practice can lead to increased pain threshold values and lower pain sensitivity even while the practitioners are not engaged in mindfulness practice.<ref name=":0" /> Grant et al<ref name=":13">Grant JA, Courtemanche J, Rainville P. [https://sci-hub.se/10.1016/j.pain.2010.10.006 A non-elaborative mental stance and decoupling of executive and pain-related cortices predicts low pain sensitivity in Zen meditators]. PAIN®. 2011 Jan 1;152(1):150-6. DOI:10.1016/j.pain.2010.10.006 </ref> studied Zen meditators using fMRI and found that long-term meditators had distinct neural pathways which predicted their low pain sensitivity. These neural pathways suggest a reduction in cognitive-emotional and evaluative processing during aversive stimulation which relates to reduced connectivity (greater “decoupling”) between the cognitive and evaluative areas of pain processing and the sensory component of pain processing.<ref name=":0" /><ref name=":12" /><ref name=":13" /> These Zen meditators still preserved the capacity to feel the pain on a sensory level, but displayed reduced affective appraisal, or less activation in the evaluative and emotional areas of the brain, related to the painful event.<ref name=":0" /><ref name=":13" /> These pathways also correspond well to the psychological construct (present moment, non-judgemental awareness) of mindfulness which resulted in the meditators possessing quieter and less reactive brains.<ref name=":13" /> | ||
== Key messages == | == Key messages == | ||
Revision as of 22:57, 31 March 2021
Original Editor - User Name
Top Contributors - Merinda Rodseth, Kim Jackson, Vidya Acharya, Jess Bell, Tarina van der Stockt and Lucinda hampton
Introduction[edit | edit source]
Evidence for the use of mindfulness has grown rapidly since its introduction to the Western world around 1979, with more than 2500 studies currently available on mindfulness (Figure 1).
Mindfulness-Based Interventions (MBI) are showing promising results in supporting mental health needs even in the absence of psychological disorders and have become a more popular, cost-effective method to provide the support.[1][2] The benefits of MBI are well established and include:[3][4][5][6]
- Decreased anxiety and depression
- Relieve of stress and psychological distress
- Increased coping abilities
- Alleviation of pain
- Decreased negative affect
- Enhanced cognitive control
- Emotion regulation
Figure 2. Benefits of Mindfulness Practice
Cognitive Changes associated with Mindfulness[edit | edit source]
The greatest impact of mindfulness is its effect on the neural plasticity of the brain. Several changes in brain activation has been documented with the practice of mindfulness, allowing us to also “see” the benefits of MBI as is evident on functional Magnetic Resonance Imaging (fMRI).[7][8] However, the study designs vary greatly with the use of different MBI and therefore the locations of the reported effects are diverse and spread over multiple regions of the brain.[7] The brain regions most consistently altered with MBI are included in Table 1.[7][9][10][11]
Table 1: Neural changes associated with mindfulness practice
| Region of the brain | Effect with MBI | Function of the region |
| Insula and sensory cortices | Increased activation | Body awareness (interoception)
Emotional processing Self-awareness Interpersonal experience |
| Anterior cingulate cortex (ACC) | Increased activation | Higher order cognitive processes
Attention and attention regulation Self and emotional regulation Cognitive distancing - associated with non-judgemental acceptance |
| Prefrontal cortex | Increased activation | Higher order cognitive processes
Attention and attention regulation Emotion regulation Meta-awareness & reappraisal Reasoning and decision making Functional connectivity with the salience network Downregulation of amygdala responses |
| Hippocampus | Increased activation
Increased volume |
Memory processes |
| Amygdala | Decreased activation
Decrease in volume/size |
Fight-or-flight reaction
Fear response Stress response Adds emotional value to sensory input - emotional processing |
Greater stress is associated with greater amygdala activation. Down-regulation of the amygdala is what underscores the reduction in stress seen with Mindfulness-Based Stress Reduction (MBSR).[10] Mindfulness is therefore not simply about paying attention. The way in which we use this focus of the mind ultimately changes the function and the structure of the brain.[12] Just as we can train our muscles to grow, we can “train” our brains as is evident in the studies about mindfulness.
Mindfulness and Pain[edit | edit source]
Chronic pain poses a significant therapeutic challenge and has been declared a public health problem, placing burdens not only on those experiencing pain, but also society as a whole.[13][14] Chronic pain is estimated to affect more than 100 million adults at any given time in the United States, with chronic back pain being the most commonly reported chronic pain complaint.[6][13][14][15] Chronic pain is also one of the primary causes of disability and decreased quality of life, resulting in a cost of more than $600 billion dollars annually in the United States alone.[13][15] Opioid medication is frequently prescribed in order to manage pain and its potential consequences, which contributed to many other problems including the “opioid epidemic” of opioid misuse, addiction and opioid-related deaths due to patients overdosing.[14][15] Mindfulness, as a nonpharmacologic option, is receiving increased interest in the management of pain.[6][15][16]
Chronic pain is complex in nature, involving many physical and psychological factors.[14][17] It is associated with sleep disturbances, obesity and weight gain, chronic fatigue, limited physical functionality and decreased quality of life.[14] Individuals suffering from a variety of chronically painful conditions are also at an increased risk for anxiety, depression and other affective disorders.[13][15][18] The International Association for the Study of Pain (IASP) defines pain as “An unpleasant sensory and emotional experience associated with, or resembling that associated with, actual or potential tissue damage.”[19] Treatment of pain should therefore also be multifaceted to address both the sensory component as well as the affective/emotional experience of pain. Treatments targeted at the negative affect associated with chronic pain are therefore hypothesised to not only positively influence the emotional distress but also influence the frequency and intensity of pain.[13] Mindfulness as a multifaceted intervention is therefore ideally placed to have a positive effect on pain and pain affect without the negative effects associated with pharmacological interventions such as opioids.[6][13][15][20]
MBSR is consistently showing positive improvements in pain management.[13][14][17] Several studies have looked at the effect of MBI on various chronic conditions and various chronically painful conditions including chronic low back pain (LBP).[21] Several of these studies can be found in Table 2.
Table 2. Studies on the effect of MBI
| Study | Year | Participants and design | Intervention | Results |
| Niazi[21] | 2011 | Systematic review
18 studies looking at chronic illness (cancer, hypertension, diabetes, HIV/AIDS, chronic pain, skin disorders) |
MBSR alone or with other treatments | Improvement in chronic conditions |
| Zeidan et al[22] | 2011 | 15 participants | 4days mindfulness meditation training | Reduction in pain intensity (40%)
Reduced pain unpleasantness (57%) |
| Zeidan et al[17] | 2015 | 75 participants | 4 groups: Mindfulness meditation, placebo, sham meditation and control | Mindfulness meditation group - significant reduction in pain intensity (27%)
Reduced pain unpleasantness (44%) |
| Morone et al[23] | 2016 | 282 participants with chronic LBP | MBSR and control group (8 weeks, 1.5 hrs once weekly) | Significant improvements in disability and quality of life |
| Cherkin et al[24] | 2016 | Randomised controlled trial
342 participants with chronic LBP |
Cognitive behavioural therapy (CBT)
MBSR 8 weekly 2-hour groups Control group (usual care) |
MBST and CBT equivalent in reducing pain and improving function showing greater improvements compared to usual care |
| Zgierska et al[25] | 2016 | 35 participants with chronic LBP | Meditation cognitive therapy and control (8 weeks, 2hrs/w)
Control/usual care group |
Significant decrease in pain intensity (short and long-term) |
| Anheyer et al[26] | 2017 | Systematic review & Meta-analysis
7 RCTs with patients with LBP |
MBSR associated with short-term improvements in pain intensity and physical functioning | |
| Banth & Ardebil[27] | 2018 | 88 patients with NSCLBP | MBSR (8 sessions) and control (usual care) | MBSR significant reduction in pain and improvement in physical and mental quality of life |
| Smith & Langen[14] | 2020 | Systematic review
12 studies in patients with chronic LBP |
Mindfulness-based interventions
Control groups |
Improvement in pain scores and quality of life after mindfulness interventions |
| Qaseem et al [28] | 2017 | Systematic review to establish practice guidelines | MBSR recommended for patients with chronic LBP |
MBIs are suggested to have greater effects on pain-related catastrophizing, especially in the presence of high levels of pain intensity, compared to traditional cognitive behavioural therapy (CBT) approaches.[13][20] In general, participants practicing mindfulness (especially MBSR) for chronic pain, displayed significantly improved outcomes of pain measures as well as quality of life and mental health measures compared to matched control groups.[14] Patients with chronic pain who engaged in mindfulness practice were generally found to be able to find new ways of living with and accepting pain, resulting in a less negative impact on their daily lives.[14] The need for methodologically sound studies on MBI for patients with chronic pain is however reiterated in many studies.[18]
Mechanism of Pain Reduction through Mindfulness Practice[edit | edit source]
Exploring the mechanisms by which mindfulness influences stress and pain, necessitate an explanation of the negative stress cycle that develops as a result of the long-term and unrelenting presence of stress and pain.[29] The negative stress cycle is set off by the occurrence of a stressful event which is often not relenting. The patient enters into a cycle of automatic thoughts about this event (the stress/pain) which leads to negative moods and emotions, ultimately resulting in maladaptive behaviours which often end up sustaining this cycle by worsening their symptoms (Figure 3).[13][29]
Figure 3. The Negative Stress Cycle
The practice of mindfulness is able to break this cycle by interrupting the “automatic thoughts” stage achieved through turning off the autopilot mode of living and guiding the awareness back to the present moment with an attitude of non-judgement and non-reactance.[14][29] MBSR proposes that mindfulness practice “will allow for the “uncoupling” of the bottom-up, afferent, sensory-driven components of pain from the top-down, psychological, cortically-driven components of pain”.[14] This suggests that awareness can result in a dissociation between the physical sensation of pain from the emotions and thoughts previously attached to pain.[14][27] The goal of mindfulness, therefore, is not to eliminate the stress or pain, but to teach the patient self-awareness and alternate responses to stress and pain by embracing the pain, accepting the moment for what it is.[14][29] By making peace with the pain, the patient is able to better manage the pain with fewer negative coping responses (including fear and anxiety).[14][27][29]
Pain reduction through mindfulness meditation also utilises different neural mechanisms as compared to placebo analgesia.[17] Besides its proposed influence on pain affect, mindfulness-based pain relief also engages brain mechanisms involved in mediating the cognitive modulation of pain, which include:[6][15][17][22]
- decreased activity in neural regions associated with low-level nociceptive processing (eg thalamus)
- Increased activity in neural regions associated with interoceptive awareness (eg right anterior insula)
- Top-down executive control (eg ACC)
- Cognitive reappraisal of sensory information (eg orbitofrontal cortex)
The ultimate strength of mindfulness lies in the neural changes it causes. Keeping in mind that “nerves that fire together, wire together”, repetitive practice of mindfulness meditation leads to changes in neural pathways resulting in a more calm, accepting disposition towards life.[29]
Several studies have found that long-term meditation practice can lead to increased pain threshold values and lower pain sensitivity even while the practitioners are not engaged in mindfulness practice.[6] Grant et al[30] studied Zen meditators using fMRI and found that long-term meditators had distinct neural pathways which predicted their low pain sensitivity. These neural pathways suggest a reduction in cognitive-emotional and evaluative processing during aversive stimulation which relates to reduced connectivity (greater “decoupling”) between the cognitive and evaluative areas of pain processing and the sensory component of pain processing.[6][29][30] These Zen meditators still preserved the capacity to feel the pain on a sensory level, but displayed reduced affective appraisal, or less activation in the evaluative and emotional areas of the brain, related to the painful event.[6][30] These pathways also correspond well to the psychological construct (present moment, non-judgemental awareness) of mindfulness which resulted in the meditators possessing quieter and less reactive brains.[30]
Key messages[edit | edit source]
- Mindfulness and neuroscience research has exploded in recent years
- Mindfulness has many benefits, especially for stress-reduction
- Through the wonder of neuroplasticity, mindfulness has shown to have a direct effect on our physiology and our psychology
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ Dunning D.L., Griffiths K., Kuyken W., Crane C., Foulkes L., Parker J., Dalgleish T. Research Review: The effects of mindfulness‐based interventions on cognition and mental health in children and adolescents–a meta‐analysis of randomized controlled trials. Journal of Child Psychology and Psychiatry. 2019; 60(3), pp.244-258. DOI:10.1111/jcpp.12980
- ↑ Nunes A, Castro SL, Limpo T. A review of mindfulness-based apps for children. Mindfulness. 2020 Sep;11(9):2089-101. DOI:10.1007/s12671-020-01410-w
- ↑ Spinelli C, Wisener M, Khoury B. Mindfulness training for healthcare professionals and trainees: A meta-analysis of randomized controlled trials. Journal of Psychosomatic Research. 2019 May 1;120:29-38. DOI:10.1016/j.jpsychores.2019.03.003
- ↑ Marusak HA, Elrahal F, Peters CA, Kundu P, Lombardo MV, Calhoun VD, Goldberg EK, Cohen C, Taub JW, Rabinak CA. Mindfulness and dynamic functional neural connectivity in children and adolescents. Behavioural brain research. 2018 Jan 15;336:211-8. DOI:10.1016/j.bbr.2017.09.010
- ↑ Geronimi EM, Arellano B, Woodruff-Borden J. Relating mindfulness and executive function in children. Clinical child psychology and psychiatry. 2020 Apr;25(2):435-45. DOI:10.1177/135910451983373
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 Zeidan F, Baumgartner JN, Coghill RC. The neural mechanisms of mindfulness-based pain relief: a functional magnetic resonance imaging-based review and primer. Pain reports. 2019 Jul;4(4). DOI:10.1097/PR9.0000000000000759
- ↑ 7.0 7.1 7.2 Tang YY, Hölzel BK, Posner MI. The neuroscience of mindfulness meditation. Nature Reviews Neuroscience. 2015 Apr;16(4):213-25. DOI:10.1038/nrn3916
- ↑ Bauer CC, Caballero C, Scherer E, West MR, Mrazek MD, Phillips DT, Whitfield-Gabrieli S, Gabrieli JD. Mindfulness training reduces stress and amygdala reactivity to fearful faces in middle-school children. Behavioral Neuroscience. 2019 Dec;133(6):569. DOI:10.1037/bne0000337
- ↑ Young KS, van der Velden AM, Craske MG, Pallesen KJ, Fjorback L, Roepstorff A, Parsons CE. The impact of mindfulness-based interventions on brain activity: A systematic review of functional magnetic resonance imaging studies. Neuroscience & Biobehavioral Reviews. 2018 Jan 1;84:424-33. DOI: 10.1016/j.neubiorev.2017.08.003
- ↑ 10.0 10.1 Gotink RA, Meijboom R, Vernooij MW, Smits M, Hunink MM. 8-week mindfulness based stress reduction induces brain changes similar to traditional long-term meditation practice–a systematic review. Brain and cognition. 2016 Oct 1;108:32-41. DOI:10.1016/j.bandc.2016.07.001
- ↑ Zimmerman B, Finnegan M, Paul S, Schmidt S, Tai Y, Roth K, Chen Y, Husain FT. Functional brain changes during mindfulness-based cognitive therapy associated with tinnitus severity. Frontiers in neuroscience. 2019 Jul 24;13:747. DOI:10.3389/fnins.2019.00747
- ↑ Siegel DJ. Mindfulness training and neural integration: Differentiation of distinct streams of awareness and the cultivation of well-being. Social cognitive and affective neuroscience. 2007 Dec 1;2(4):259-63. DOI:10.1093/scan/nsm034
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 13.8 Edwards RR, Dworkin RH, Sullivan MD, Turk DC, Wasan AD. The role of psychosocial processes in the development and maintenance of chronic pain. The Journal of Pain. 2016 Sep 1;17(9): T70-92. DOI:10.1016/j.jpain.2016.01.001
- ↑ 14.00 14.01 14.02 14.03 14.04 14.05 14.06 14.07 14.08 14.09 14.10 14.11 14.12 14.13 Smith SL, Langen WH. A systematic review of mindfulness practices for improving outcomes in chronic low back pain. International Journal of Yoga. 2020 Sep;13(3):177. DOI:10.4103/ijoy.IJOY_4_20
- ↑ 15.0 15.1 15.2 15.3 15.4 15.5 15.6 McClintock AS, McCarrick SM, Garland EL, Zeidan F, Zgierska AE. Brief mindfulness-based interventions for acute and chronic pain: A systematic review. The Journal of Alternative and Complementary Medicine. 2019 Mar 1;25(3):265-78. DOI:10.1089/acm.2018.0351
- ↑ Ngamkham S, Holden JE, Smith EL. A systematic review: mindfulness intervention for cancer-related pain. Asia-Pacific journal of oncology nursing. 2019 Apr;6(2):161. DOI:10.4103/apjon.apjon_67_18
- ↑ 17.0 17.1 17.2 17.3 17.4 Zeidan F, Emerson NM, Farris SR, Ray JN, Jung Y, McHaffie JG, Coghill RC. Mindfulness meditation-based pain relief employs different neural mechanisms than placebo and sham mindfulness meditation-induced analgesia. Journal of Neuroscience. 2015 Nov 18;35(46):15307-25. DOI:10.1523/JNEUROLSCI.2542-15.2015
- ↑ 18.0 18.1 Hilton L, Hempel S, Ewing BA, Apaydin E, Xenakis L, Newberry S, Colaiaco B, Maher AR, Shanman RM, Sorbero ME, Maglione MA. Mindfulness meditation for chronic pain: systematic review and meta-analysis. Annals of Behavioral Medicine. 2017 Apr 1;51(2):199-213. DOI:10.1007/s12160-016-9844-2
- ↑ International Association for the Study of Pain. IASP Terminology. Last Updated: December 14, 2017. [Accessed 29 March 2021].
- ↑ 20.0 20.1 Elvery N, Jensen MP, Ehde DM, Day MA. Pain catastrophizing, mindfulness, and pain acceptance. The Clinical journal of pain. 2017 Jun 1;33(6):485-95. DOI:10.1097/AJP.0000000000000430
- ↑ 21.0 21.1 Niazi AK, Niazi SK. Mindfulness-based stress reduction: a non-pharmacological approach for chronic illnesses. North American journal of medical sciences. 2011 Jan;3(1):20. DOI:10.4297/najms.2011.320
- ↑ 22.0 22.1 Zeidan F, Martucci KT, Kraft RA, Gordon NS, McHaffie JG, Coghill RC. Brain mechanisms supporting the modulation of pain by mindfulness meditation. J Neurosci. 2011 Apr 6;31(14):5540-8. DOI:10.1523/JNEUROSCI.5791-10.2011.
- ↑ Morone NE, Greco CM, Moore CG, Rollman BL, Lane B, Morrow LA, Glynn NW, Weiner DK. A mind-body program for older adults with chronic low back pain: a randomized clinical trial. JAMA internal medicine. 2016 Mar 1;176(3):329-37. DOI:10.1001/jamainternmed.2015.8033
- ↑ Cherkin, D.C., Sherman, K.J., Balderson, B.H., Cook, A.J., Anderson, M.L., Hawkes, R.J., Hansen, K.E. and Turner, J.A., 2016. Effect of mindfulness-based stress reduction vs cognitive behavioral therapy or usual care on back pain and functional limitations in adults with chronic low back pain: a randomized clinical trial. Jama, 315(12), pp.1240-1249. DOI:10.1001/jama.2016.2323.
- ↑ Zgierska AE, Burzinski CA, Cox J, Kloke J, Stegner A, Cook DB, Singles J, Mirgain S, Coe CL, Bačkonja M. Mindfulness meditation and cognitive behavioral therapy intervention reduces pain severity and sensitivity in opioid-treated chronic low back pain: pilot findings from a randomized controlled trial. Pain Medicine. 2016 Oct 1;17(10):1865-81. DOI: 10.1093/pm/pnw006
- ↑ Anheyer D, Haller H, Barth J, Lauche R, Dobos G, Cramer H. Mindfulness-based stress reduction for treating low back pain: a systematic review and meta-analysis. Annals of internal medicine. 2017 Jun 6;166(11):799-807. DOI: 10.7326/m16-1997
- ↑ 27.0 27.1 27.2 Banth S, Ardebil MD. Effectiveness of mindfulness meditation on pain and quality of life of patients with chronic low back pain. International journal of yoga. 2015 Jul;8(2):128. DOI:10.4103/0973-6131.158476
- ↑ Qaseem A, Wilt TJ, McLean RM, Forciea MA. Noninvasive treatments for acute, subacute, and chronic low back pain: a clinical practice guideline from the American College of Physicians. Annals of internal medicine. 2017 Apr 4;166(7):514-30. DOI: 10.7326/M16-2367.
- ↑ 29.0 29.1 29.2 29.3 29.4 29.5 29.6 Shrey Vazir. Mindful Meditation in Chronic Pain Management. Physioplus Course. 2021
- ↑ 30.0 30.1 30.2 30.3 Grant JA, Courtemanche J, Rainville P. A non-elaborative mental stance and decoupling of executive and pain-related cortices predicts low pain sensitivity in Zen meditators. PAIN®. 2011 Jan 1;152(1):150-6. DOI:10.1016/j.pain.2010.10.006