Dance Injuries of the Foot and Ankle: Difference between revisions
m (Protected "Dance Injuries of the Foot and Ankle": Course Page ([Edit=⧼protect-level-ppadmin⧽] (indefinite) [Move=⧼protect-level-ppadmin⧽] (indefinite))) |
Kim Jackson (talk | contribs) m (Text replacement - "[[Extracorporeal Shockwave Therapy (ESWT)" to "[[Extracorporeal Shockwave Therapy ") |
||
| (27 intermediate revisions by 4 users not shown) | |||
| Line 2: | Line 2: | ||
== Introduction == | == Introduction == | ||
85% of dancers will have some form of musculoskeletal injury during career and | Approximately 85% of dancers will have some form of musculoskeletal injury during their career and around 50% of these occur in the ankle or foot.<ref name=":11">Green-Smerdon M. Dance Injuries of the Ankle and Foot Course. Plus , 2022.</ref> Moreover, injuries which are higher up in the chain will have an effect on the ankle and foot. The foot is essential to a dancer; it acts as their base of support, it is a lever to propel movement and an important shock absorber. As well as this, most of a dancer's artistic expression comes from their foot.<ref name=":11" /> | ||
The incidence of injuries in dancers varies from 40% to 84%. Most injures are caused by low cardiovascular conditioning, joint hypermobility, postural deviations, and alterations in the body’s center of balance.<ref name=":0">Cardoso AA, Reis NM, Marinho AP, Vieira MD, Boing L, Guimarães AC. [https://www.scielo.br/j/rbme/a/ZMwvSfMh6WSbBxZPhWGnf3k/?format=html&lang=en&stop=next Injuries in professional dancers: a systematic review.] Revista Brasileira de Medicina do Esporte. 2017 Nov;23:504-9.</ref><blockquote>“[F]or each 1000 hours of training, the injuries incidence diagnosed was from 0.62 to 5.6 injuries per dancers. Bearing in mind that the technical demand for a professional dancers is even higher, it is considered that this number increases drastically into the professional contest.”<ref name=":0" /></blockquote> | |||
== Acute vs Overuse Injuries == | |||
* Acute<ref name=":11" /> | |||
** Often attributed to poor technique and incorrect execution of jumps and landing | |||
** Dancer usually reports a specific incident | |||
** Many other contributing factors such as tiredness, fatigue or loss of balance | |||
* Overuse<ref name=":11" /> | |||
** Excessive use | |||
** Repeated microtrauma | |||
== Risk Factors == | == Risk Factors == | ||
The following are risk factors for injuries in dancers:<ref name=":11" /> | |||
* Previous injuries | * Previous injuries | ||
* Poor rehabilitation | * Poor rehabilitation | ||
* Anatomical posture | * Anatomical posture | ||
* Poor training | * Poor training resulting in poor muscular strength<ref name=":1">Skwiot M, Śliwiński Z, Żurawski A, Śliwiński G. [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0253437 Effectiveness of physiotherapy interventions for injury in ballet dancers: A systematic review.] PLoS one. 2021 Jun 24;16(6):e0253437.</ref> | ||
* Poor lumbopelvic control<ref name=":2">Biernacki JL, Stracciolini A, Fraser J, Micheli LJ, Sugimoto D. [https://journals.lww.com/cjsportsmed/Abstract/2021/03000/Risk_Factors_for_Lower_Extremity_Injuries_in.13.aspx?context=LatestArticles Risk factors for lower-extremity injuries in female ballet dancers: a systematic review]. Clinical journal of sport medicine. 2021 Mar 1;31(2):e64-79.</ref> | * Poor lumbopelvic control<ref name=":2">Biernacki JL, Stracciolini A, Fraser J, Micheli LJ, Sugimoto D. [https://journals.lww.com/cjsportsmed/Abstract/2021/03000/Risk_Factors_for_Lower_Extremity_Injuries_in.13.aspx?context=LatestArticles Risk factors for lower-extremity injuries in female ballet dancers: a systematic review]. Clinical journal of sport medicine. 2021 Mar 1;31(2):e64-79.</ref> | ||
* Technical mistakes<ref name=":1" /> | * Technical mistakes<ref name=":1" /> | ||
| Line 16: | Line 28: | ||
* Dance style | * Dance style | ||
* Shoe fit and style | * Shoe fit and style | ||
* Floor type<ref name=":0" /><ref name=":7">Campbell RS, Lehr ME, Livingston A, McCurdy M, Ware JK. [https://www.sciencedirect.com/science/article/abs/pii/S1466853X18305169 Intrinsic modifiable risk factors in ballet dancers: Applying evidence based practice principles to enhance clinical applications.] Physical Therapy in Sport. 2019 Jul 1;38:106-14.</ref> | |||
'''Additional contributing factors can include''':<ref name=":11" /> | |||
* Transitioning from part-time to professional dancer<ref>Fuller M, Moyle GM, Hunt AP, Minett GM. [https://www.ingentaconnect.com/content/jmrp/jdms/2019/00000023/00000003/art00004 Ballet and contemporary dance injuries when transitioning to full-time training or professional level dance: a systematic review]. Journal of Dance Medicine & Science. 2019 Sep 1;23(3):112-25.</ref> | |||
* Transitioning from | |||
* The foot can affect the knee, hip, core musculature and spine | * The foot can affect the knee, hip, core musculature and spine | ||
* | * Lack of turnout | ||
* Biomechanical requirements<ref name=":2" /> | * Biomechanical requirements of pointe and demi-pointe - i.e. full plantarflexion with 90 degrees of metatarsal phalangeal joint extension<ref name=":2" /> | ||
* The dancer's body and their management | |||
* The | |||
* Psychology and expectations of dancers | * Psychology and expectations of dancers | ||
* | * Decreased [[Triceps Surae|triceps surae]] (gastrocnemius and soleus) and [[Tibialis Posterior|tibialis posterior]] strength<ref name=":8" /> | ||
* Decreased plantarflexion active range of motion<ref name=":8">En Pointe: [https://www.orthocarolina.com/media/en-pointe-what-ballet-dancers-should-know-about-injury-prevention What Ballet Dancers Should Know About Injury Prevention]</ref> | |||
'''Muscle weakness often results in''':<ref name=":11" /> | |||
* Rolling in and out of the ankles (increased ankle inversion / eversion) | |||
* Decreased stability en pointe | |||
* Decreased plantarflexion range of motion | |||
== Anterior Ankle Injuries == | |||
* | * Anterior bone spurs | ||
** Often found in mature or retired dancers | |||
* [[Medial Tibial Stress Syndrome|Tibial stress syndrome]]<ref name=":3">Rietveld AB. [https://scholarlypublications.universiteitleiden.nl/access/item%3A2947375/view Performing arts medicine with a focus on Relevé in Dancers]. Leiden University; 2017 Nov 28.</ref> | |||
* Tibial [[Stress Fractures|stress fracture]] | |||
* | * Anterior ligament Injury | ||
* | * [[Extensor Hallucis Longus|Extensor hallucis longus]] tendon pathology | ||
* Tibial stress syndrome<ref name=":3" /> | ** This is common in dancers spending hours trying to improve their pointe work and can result in long-term instability | ||
* Tibial stress fracture | |||
* Anterior | |||
* Anterior capsule synovitis | * Anterior capsule synovitis | ||
* [[Anterior Ankle Impingement Syndrome|Anterior impingement]] | |||
==== Anterior impingement syndrome ==== | ==== Anterior Impingement Syndrome ==== | ||
Anterior impingement syndrome is the primary anterior ankle injury in dancers:<ref name=":11" /> | |||
* Aggravated by repetitive forced dorsiflexion | |||
* Symptoms are generally progressive in nature | |||
* Treatment:<ref name=":11" /> | |||
** Educate the dancer on correct stretching, focus on strengthening the intrinsic and extrinsic muscles | |||
** Address biomechanical faults and look higher up the chain for compensations or weakness | |||
** [[Mulligan Concept|Mulligan]] mobilisation with movement, passive accessory movement, chair ankle rocker (example below) | |||
** Often responsive to conservative treatment | |||
** Surgery is effective if condition has progressed far enough<ref name=":4">Khurana A, Singh I, Singh MS. [https://jassm.org/is-anterior-and-posterior-ankle-impingement-under-diagnosed-a-review/ Is anterior and posterior ankle impingement under-diagnosed? A review]. Journal of Arthroscopic Surgery and Sports Medicine. 2021 Jan 10;2(1):58-65.</ref> | |||
*'''Ballet specific considerations''':<ref name=":11" /> | |||
** Dance movements which contribute to anterior impingement syndrome are: plié, forcing turnout and rolling ankles | |||
** Compensation: Dancer lifts heel up earlier in a plié | |||
[[File:Chair ankle rocker.png|center|thumb|400x400px|'''Chair Ankle Rocker -''' With one foot up on a chair, rock forwards from neutral into dorsiflexion]] | |||
== Posterior Ankle Injuries == | |||
== | * [[Ankle Impingement|Posterior ankle impingement syndrome]] | ||
* [[Achilles Tendinopathy|Achilles tendinopathy]]<ref name=":5">Batenhorst EZ. [https://digitalcommons.wou.edu/cgi/viewcontent.cgi?article=1225&context=honors_theses A Dancer’s View: Analysis and Prevention of Common Dance Injuries]. 2020</ref> | |||
** The prevalence of this injury in dancers is due to movements such as: relevés, jumps, turns, and pointe work | |||
** Can be caused by tying ribbons incorrectly across the Achilles tendon or from dancing on hard floors | |||
** Changing choreographers is often a contributing factor, especially if the new choreographer advocates for an intense jumping routine or encourages faster direction changes<ref name=":11" /> | |||
==== Posterior Ankle Impingement Syndrome ==== | |||
* Often referred to as Dancer's heel, can be bony or soft tissue | |||
* Aggravated by forced plantarflexion and often coincides with flexor hallucis longus [[tendinopathy]] | |||
* Symptoms include: | |||
** Pain and tenderness over the posterolateral aspect of the ankle | |||
** Pain with: | |||
*** Active plantarflexion | |||
*** Axial loading | |||
*** Great toe dorsiflexion | |||
* Treatment | |||
** Education | |||
** Late-stage degeneration can be operated on<ref name=":4" /><ref>Grigoryev K. ''[https://www.proquest.com/openview/13aa37c86679bb28ab06a1a1d8ee37f0/1?pq-origsite=gscholar&cbl=18750&diss=y Comparison of Open and Endoscopic Surgical Procedures as a Treatment of Posterior Ankle Impingement Syndrome in Ballet Dancers: A Meta-Analysis]'' (Doctoral dissertation, California State University, Fresno).</ref> | |||
* '''Ballet specific considerations:''' | |||
**'''Biomechanics check''': plié, grand plié, relevé | |||
** '''Stretch''': hamstrings, adductors, tibialis anterior, gastrocnemius and soleus | |||
** '''Strengthen''': gluteals, hamstrings, adductors, abductors | |||
** '''Specific rehabilitation:''' Mobility crawls (example below), isometric single leg heel raise, eccentric single leg heel lowering | |||
[[File:Mobility Crawls(1).jpg|center|thumb|500x500px|Mobility Crawls]] | |||
* | |||
== | == Lateral Ankle Injuries == | ||
* | * [[Management of Ankle Sprains|Lateral ankle sprains]]<ref name=":6">Bodini BD, Lucenteforte G, Serafin P, Barone L, Vitale JA, Serafin A, Sansone V, Negrini F. [https://www.mdpi.com/2076-3417/10/1/155 Do grade II ankle sprains have chronic effects on the functional ability of ballet dancers performing single-leg flat-foot stance? An observational cross-sectional study.] Applied Sciences. 2020 Jan;10(1):155.</ref> | ||
* Cuboid subluxation | |||
** Rotational strain to bone following other issues | |||
* [[Sinus Tarsi Syndrome|Sinus tarsi syndrome]] | |||
* [[Peroneal Tendinopathy|Peroneal tendon overuse]] and retinaculum stress<ref name=":11" /> | |||
* | |||
* | |||
* | |||
* | |||
* | |||
==== Lateral Ankle Sprain ==== | |||
* | * Aggravated by weak [[Triceps Surae|triceps surae]] (gastrocnemius and soleus) and posterior tibialis strength | ||
* | * Symptoms include: pain, swelling and instability | ||
* | * Treatment:<ref name=":11" /> | ||
** Ice, strapping, electrotherapy modalities, muscle strengthening | |||
* '''Ballet specific considerations''':<ref name=":11" /> | |||
** Dancer regularly relies on feedback and stability from the lateral ligament<ref name=":6" /> | |||
**'''Biomechanics check''': First position pilé, relevé, passé, alignment in demi-pointe or pointe<ref name=":5" /> | |||
**'''Stretch''': hamstrings, quadriceps, adductors, iliopsoas, gastrocnemius and soleus | |||
**'''Strengthen''': gluteals, dorsiflexors, everters | |||
**'''Specific rehabilitation:''' aggressive strengthening and proprioception, side plank theraband clamshell, single leg balance with tap to front around to back (example below, resisted plantarflexion with eversion | |||
[[File:SLB tap.png|center|thumb|400x400px|Single leg balance with tap to front around to back]] | |||
== | == Toe Injuries == | ||
* | * [[Hallux Valgus|Hallux valgus]]<ref name=":9">Mira NO, Marulanda AF, Peña AC, Torres DC, Orrego JC. [https://www.ingentaconnect.com/content/jmrp/jdms/2019/00000023/00000004/art00003 Study of ballet dancers during cou-de-pied derrière with demi-plié to piqué arabesque]. Journal of Dance Medicine & Science. 2019 Dec 15;23(4):150-8.</ref> | ||
* | * [[Hallux Rigidus|Hallux rigidus]]<ref name=":9" /> | ||
* Bunions<ref name=":9" /> | |||
** Aim to strengthen intrinsic foot muscles | |||
** Correct alignment and use toe spacers if required | |||
* [[Sesamoiditis]]<ref name=":9" /> | |||
* [[Metatarsalgia]]<ref name=":9" /> | |||
* [[Metatarsal Fractures|5th metatarsal fracture]] / Dancer's fracture / [[Lisfranc Injuries|Lisfranc]] fracture | |||
* | |||
* | |||
* | |||
** Correct alignment and toe spacers | |||
* | |||
* Metatarsalgia | |||
* 5th metatarsal fracture/ | |||
* Hammer toe | * Hammer toe | ||
* Blisters | * Blisters | ||
* Ingrown toe nails | * Ingrown toe nails | ||
==== Hallux | ==== Hallux Rigidus ==== | ||
* Associated with the [[flexor hallucis longus]],<ref name=":10">Ogilvie-Harris DJ, Carr MM, Fleming PJ. [https://journals.sagepub.com/doi/abs/10.1177/107110079501600307 The foot in ballet dancers: the importance of second toe length]. Foot & ankle international. 1995 Mar;16(3):144-7.</ref><ref>Wentzell M. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6173219/ Conservative management of a chronic recurrent flexor hallucis longus stenosing tenosynovitis in a pre-professional ballet dancer: a case report.] The Journal of the Canadian Chiropractic Association. 2018 Aug;62(2):111.</ref> which is the primary dynamic stabiliser of the medial ankle en pointe and demi-pointe positions<ref name=":11" /> | |||
* Can be aggravated when the second toe is longer than the first,<ref name=":10" /> or by excessive interphalangeal joint flexion compensation, also referred to as knuckling under | |||
* Symptoms include: stiff and painful joint<ref>Anderson MR, Ho BS, Baumhauer JF. [https://journals.sagepub.com/doi/full/10.1177/2473011418764461 Current concepts review: hallux rigidus. Foot & Ankle Orthopaedics.] 2018 Jun 7;3(2):2473011418764461.</ref> | |||
* Treatment: | |||
** Late-stage treatment is a surgical debridement<ref>Carpenter B, Gentile M, Hagenbucher JR. [https://internationalfootankle.org/journal/index.php/JIFAF/article/view/1 Functional hallux rigidus in high level athletes: Arthroscopic repair by flexor hallucis longus debridement.] Journal of the International Foot & Ankle Foundation. 2022;1(1).</ref> | |||
* Ballet specific considerations:<ref name=":11" /> | |||
**'''Biomechanics check:''' first position and passé | |||
**'''Stretch:''' iliopsoas, quadriceps, adductors, calf muscles | |||
**'''Strengthen:''' gluteals, hamstrings, adductors, abductors | |||
**'''Specific rehabilitation:''' toe / ankle rocker with a toe spacer, great toe flexion and extension, isometric theraband toe abduction, flexion with theraband, toe abduction, toe separation | |||
* | ==== Sesamoiditis ==== | ||
* | Sesamoid bones are embedded within the [[Flexor Hallucis Brevis|flexor hallucis brevis]] (FHB) tendon and articulate with the plantar surface of the first metatarsal head. They help to stabilise the first metatarsal phalangeal joint and improve the power of the FHB tendon.<ref name=":11" /> | ||
* Strengthen | * In dance, they are aggravated by:<ref name=":11" /> | ||
* | ** Technical errors, such as rolling in, pronation and forcing turnout | ||
** Collapsed arches which puts more pressure on the sesamoids | |||
** Taking off and landing jumps especially without plié | |||
** Rolling into relevé / demi-pointe (more stressful than en pointe) | |||
** Walking with toe out gait | |||
* Symptoms include: pain under the first metatarsal head on the plantar forefoot, tenderness should move distally with dorsiflexion of great toe<ref name=":11" /> | |||
* Treatment:<ref name=":11" /> | |||
** Educate the dancer on the use of stiff soled shoes outside class, which offer more support | |||
** Encourage padding to off-load the area | |||
** Always assess and correct alignment | |||
** Unfortunately this condition takes months to resolve | |||
* Ballet specific considerations:<ref name=":11" /> | |||
**'''Stretch:''' hamstrings, gluteal muscles, adductors, and roll out calf muscles | |||
**'''Strengthen:''' gluteal muscles, hamstrings, adductors, iliopsoas, intrinsic foot muscles | |||
**'''Specific rehabilitation:''' Theraband clamshells, foam roll ball squeeze with leg lowering (example below), prone hamstring curl to hip extension | |||
[[File:Foam ball low.png|center|thumb|450x450px|Foam roll ball squeeze with leg lowering]] | |||
==== | ==== 5th Metatarsal Fracture ==== | ||
* | * Often referred to as a Dancer's fracture | ||
* Aggravated by twisting injuries | |||
* Remember to differentiate between a Dancer's fracture and a Jones fracture, which occurs further down towards the base of the 5th metatarsal (i.e. at the proximal metadiaphyseal junction<ref>Datir A, Bell D. [https://radiopaedia.org/articles/jones-fracture-1 Jones fracture]. Reference article, Radiopaedia.org [cited 18 May 2022]. Available from: https://radiopaedia.org/articles/jones-fracture-1</ref>) and is caused by repetitive stress<ref name=":11" /> | |||
* | ** Please note, a Jones fracture requires surgery | ||
* | * Treatment of a Dancer's fracture is conservative / non-operative | ||
* | * Ballet specific considerations:<ref name=":11" /> | ||
* | **'''Stretch:''' hamstrings, gluteal muscles, adductors, and roll out calf muscles | ||
* | **'''Strengthen:''' gluteal muscles, hamstrings, adductors, iliopsoas | ||
* Strengthen | **'''Specific rehabilitation:''' side plank hip adduction, foam roll, quadruped donkey kicks, quadruped Continuous Articular Rotation wheel (example below) | ||
* | [[File:CAR Wheel(1).png|center|thumb|500x500px|Quadruped Continuous Articular Rotation Wheel]] | ||
==== | == Plantar Fasciitis == | ||
* | * [[Plantar Fasciitis|Plantar fasciitis]] is often associated with repetitive jumping, which is why it has a high prevalence in dancers<ref name=":5" /> | ||
* Symptoms include:<ref name=":11" /> | |||
* | ** Heel pain with first steps in the morning | ||
** Heel pain after long periods of non-weight bearing | |||
** Tenderness to the anterior medial heel | |||
** Limited dorsiflexion and a tight [[Achilles Tendon|Achilles tendon]] | |||
** A limp may be present or there may be a preference for toe walking | |||
** Pain is usually worse when barefoot on hard surfaces and with stair climbing | |||
* Treatment:<ref name=":11" /> | |||
** Conservative measures are the first choice | |||
** Physiotherapy | |||
** Rest from offending activity | |||
**[[Cryotherapy|Ice]] after activity | |||
** Deep [[Friction Massage|friction]] massage of the arch and insertion | |||
** Shoe inserts or [[Introduction to Orthotics]] and night splints | |||
**[[Extracorporeal Shockwave Therapy |Extracorporeal shock-wave therapy]]<ref>Rhim HC, Kwon J, Park J, Borg-Stein J, Tenforde AS. [https://www.mdpi.com/2075-1729/11/12/1287 A Systematic Review of Systematic Reviews on the Epidemiology, Evaluation, and Treatment of Plantar Fasciitis]. Life. 2021 Dec;11(12):1287.</ref> , botulinum toxin A, [[Lateral Epicondyle Tendinopathy Toolkit: Appendix G - Medical and Surgical Interventions|autologous platelet-rich plasma, dextrose prolotherapy, or steroid injections]] | |||
** Advanced and invasive techniques should be combined with conservative therapy | |||
** Surgery should be the last option if this process has become chronic and other less invasive therapies have failed<span class="reference" id="cite_ref-:0_2-3"></span> | |||
* Educate the dancer on proper stretching and rehabilitation of the: plantar fascia; [[Achilles Tendon|Achilles' tendon]]; [[gastrocnemius]] and [[soleus]] | |||
* | * Ballet specific considerations:<ref name=":11" /> | ||
* | **'''Biomechanics check:''' plié, developpe and gait | ||
* | **'''Stretch:''' iliopsoas, quadriceps, adductors, calf muscles | ||
* Strengthen | **'''Strengthen:''' gluteal muscles, abductors, deep rotators | ||
* | **'''Specific rehabilitation:''' chair straight leg bridges, straight leg heel raises on stairs, ankle / toe rockers, strapping | ||
'''For more specific physiotherapy treatment options please see the [[Plantar Fasciitis]] page.''' | |||
== Foot and Ankle Care == | == Foot and Ankle Care == | ||
* | * Pointe work should always be progressed slowly and only once the individual has been assessed | ||
* | * Foot alignment should always be monitored | ||
* | * Balance exercises, intrinsic foot exercises and calf stretching and strengthening should be included in training | ||
* Dancers should be encouraged to walk with a normal of angle of gait, which allows off-loading of the hip rotators (i.e., not walking in a turnout position)<ref name=":11" /> | |||
* | |||
== References == | == References == | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category: | [[Category:Plus Content]] | ||
[[Category:Foot]] | [[Category:Foot]] | ||
[[Category:Foot - Conditions]] | [[Category:Foot - Conditions]] | ||
Latest revision as of 18:25, 9 January 2024
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson, Olajumoke Ogunleye and Nupur Smit Shah
Introduction[edit | edit source]
Approximately 85% of dancers will have some form of musculoskeletal injury during their career and around 50% of these occur in the ankle or foot.[1] Moreover, injuries which are higher up in the chain will have an effect on the ankle and foot. The foot is essential to a dancer; it acts as their base of support, it is a lever to propel movement and an important shock absorber. As well as this, most of a dancer's artistic expression comes from their foot.[1]
The incidence of injuries in dancers varies from 40% to 84%. Most injures are caused by low cardiovascular conditioning, joint hypermobility, postural deviations, and alterations in the body’s center of balance.[2]
“[F]or each 1000 hours of training, the injuries incidence diagnosed was from 0.62 to 5.6 injuries per dancers. Bearing in mind that the technical demand for a professional dancers is even higher, it is considered that this number increases drastically into the professional contest.”[2]
Acute vs Overuse Injuries[edit | edit source]
- Acute[1]
- Often attributed to poor technique and incorrect execution of jumps and landing
- Dancer usually reports a specific incident
- Many other contributing factors such as tiredness, fatigue or loss of balance
- Overuse[1]
- Excessive use
- Repeated microtrauma
Risk Factors[edit | edit source]
The following are risk factors for injuries in dancers:[1]
- Previous injuries
- Poor rehabilitation
- Anatomical posture
- Poor training resulting in poor muscular strength[3]
- Poor lumbopelvic control[4]
- Technical mistakes[3]
- Execution speed[3]
- Choreographer
- Dance style
- Shoe fit and style
- Floor type[2][5]
Additional contributing factors can include:[1]
- Transitioning from part-time to professional dancer[6]
- The foot can affect the knee, hip, core musculature and spine
- Lack of turnout
- Biomechanical requirements of pointe and demi-pointe - i.e. full plantarflexion with 90 degrees of metatarsal phalangeal joint extension[4]
- The dancer's body and their management
- Psychology and expectations of dancers
- Decreased triceps surae (gastrocnemius and soleus) and tibialis posterior strength[7]
- Decreased plantarflexion active range of motion[7]
Muscle weakness often results in:[1]
- Rolling in and out of the ankles (increased ankle inversion / eversion)
- Decreased stability en pointe
- Decreased plantarflexion range of motion
Anterior Ankle Injuries[edit | edit source]
- Anterior bone spurs
- Often found in mature or retired dancers
- Tibial stress syndrome[8]
- Tibial stress fracture
- Anterior ligament Injury
- Extensor hallucis longus tendon pathology
- This is common in dancers spending hours trying to improve their pointe work and can result in long-term instability
- Anterior capsule synovitis
- Anterior impingement
Anterior Impingement Syndrome[edit | edit source]
Anterior impingement syndrome is the primary anterior ankle injury in dancers:[1]
- Aggravated by repetitive forced dorsiflexion
- Symptoms are generally progressive in nature
- Treatment:[1]
- Educate the dancer on correct stretching, focus on strengthening the intrinsic and extrinsic muscles
- Address biomechanical faults and look higher up the chain for compensations or weakness
- Mulligan mobilisation with movement, passive accessory movement, chair ankle rocker (example below)
- Often responsive to conservative treatment
- Surgery is effective if condition has progressed far enough[9]
- Ballet specific considerations:[1]
- Dance movements which contribute to anterior impingement syndrome are: plié, forcing turnout and rolling ankles
- Compensation: Dancer lifts heel up earlier in a plié
Posterior Ankle Injuries[edit | edit source]
- Posterior ankle impingement syndrome
- Achilles tendinopathy[10]
- The prevalence of this injury in dancers is due to movements such as: relevés, jumps, turns, and pointe work
- Can be caused by tying ribbons incorrectly across the Achilles tendon or from dancing on hard floors
- Changing choreographers is often a contributing factor, especially if the new choreographer advocates for an intense jumping routine or encourages faster direction changes[1]
Posterior Ankle Impingement Syndrome[edit | edit source]
- Often referred to as Dancer's heel, can be bony or soft tissue
- Aggravated by forced plantarflexion and often coincides with flexor hallucis longus tendinopathy
- Symptoms include:
- Pain and tenderness over the posterolateral aspect of the ankle
- Pain with:
- Active plantarflexion
- Axial loading
- Great toe dorsiflexion
- Treatment
- Ballet specific considerations:
- Biomechanics check: plié, grand plié, relevé
- Stretch: hamstrings, adductors, tibialis anterior, gastrocnemius and soleus
- Strengthen: gluteals, hamstrings, adductors, abductors
- Specific rehabilitation: Mobility crawls (example below), isometric single leg heel raise, eccentric single leg heel lowering
Lateral Ankle Injuries[edit | edit source]
- Lateral ankle sprains[12]
- Cuboid subluxation
- Rotational strain to bone following other issues
- Sinus tarsi syndrome
- Peroneal tendon overuse and retinaculum stress[1]
Lateral Ankle Sprain[edit | edit source]
- Aggravated by weak triceps surae (gastrocnemius and soleus) and posterior tibialis strength
- Symptoms include: pain, swelling and instability
- Treatment:[1]
- Ice, strapping, electrotherapy modalities, muscle strengthening
- Ballet specific considerations:[1]
- Dancer regularly relies on feedback and stability from the lateral ligament[12]
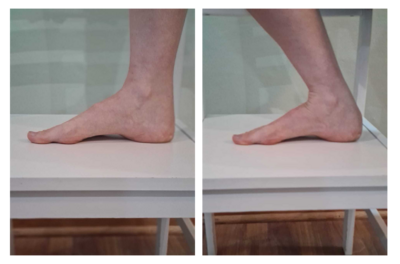
- Biomechanics check: First position pilé, relevé, passé, alignment in demi-pointe or pointe[10]
- Stretch: hamstrings, quadriceps, adductors, iliopsoas, gastrocnemius and soleus
- Strengthen: gluteals, dorsiflexors, everters
- Specific rehabilitation: aggressive strengthening and proprioception, side plank theraband clamshell, single leg balance with tap to front around to back (example below, resisted plantarflexion with eversion
Toe Injuries[edit | edit source]
- Hallux valgus[13]
- Hallux rigidus[13]
- Bunions[13]
- Aim to strengthen intrinsic foot muscles
- Correct alignment and use toe spacers if required
- Sesamoiditis[13]
- Metatarsalgia[13]
- 5th metatarsal fracture / Dancer's fracture / Lisfranc fracture
- Hammer toe
- Blisters
- Ingrown toe nails
Hallux Rigidus[edit | edit source]
- Associated with the flexor hallucis longus,[14][15] which is the primary dynamic stabiliser of the medial ankle en pointe and demi-pointe positions[1]
- Can be aggravated when the second toe is longer than the first,[14] or by excessive interphalangeal joint flexion compensation, also referred to as knuckling under
- Symptoms include: stiff and painful joint[16]
- Treatment:
- Late-stage treatment is a surgical debridement[17]
- Ballet specific considerations:[1]
- Biomechanics check: first position and passé
- Stretch: iliopsoas, quadriceps, adductors, calf muscles
- Strengthen: gluteals, hamstrings, adductors, abductors
- Specific rehabilitation: toe / ankle rocker with a toe spacer, great toe flexion and extension, isometric theraband toe abduction, flexion with theraband, toe abduction, toe separation
Sesamoiditis[edit | edit source]
Sesamoid bones are embedded within the flexor hallucis brevis (FHB) tendon and articulate with the plantar surface of the first metatarsal head. They help to stabilise the first metatarsal phalangeal joint and improve the power of the FHB tendon.[1]
- In dance, they are aggravated by:[1]
- Technical errors, such as rolling in, pronation and forcing turnout
- Collapsed arches which puts more pressure on the sesamoids
- Taking off and landing jumps especially without plié
- Rolling into relevé / demi-pointe (more stressful than en pointe)
- Walking with toe out gait
- Symptoms include: pain under the first metatarsal head on the plantar forefoot, tenderness should move distally with dorsiflexion of great toe[1]
- Treatment:[1]
- Educate the dancer on the use of stiff soled shoes outside class, which offer more support
- Encourage padding to off-load the area
- Always assess and correct alignment
- Unfortunately this condition takes months to resolve
- Ballet specific considerations:[1]
- Stretch: hamstrings, gluteal muscles, adductors, and roll out calf muscles
- Strengthen: gluteal muscles, hamstrings, adductors, iliopsoas, intrinsic foot muscles
- Specific rehabilitation: Theraband clamshells, foam roll ball squeeze with leg lowering (example below), prone hamstring curl to hip extension
5th Metatarsal Fracture[edit | edit source]
- Often referred to as a Dancer's fracture
- Aggravated by twisting injuries
- Remember to differentiate between a Dancer's fracture and a Jones fracture, which occurs further down towards the base of the 5th metatarsal (i.e. at the proximal metadiaphyseal junction[18]) and is caused by repetitive stress[1]
- Please note, a Jones fracture requires surgery
- Treatment of a Dancer's fracture is conservative / non-operative
- Ballet specific considerations:[1]
- Stretch: hamstrings, gluteal muscles, adductors, and roll out calf muscles
- Strengthen: gluteal muscles, hamstrings, adductors, iliopsoas
- Specific rehabilitation: side plank hip adduction, foam roll, quadruped donkey kicks, quadruped Continuous Articular Rotation wheel (example below)
Plantar Fasciitis[edit | edit source]
- Plantar fasciitis is often associated with repetitive jumping, which is why it has a high prevalence in dancers[10]
- Symptoms include:[1]
- Heel pain with first steps in the morning
- Heel pain after long periods of non-weight bearing
- Tenderness to the anterior medial heel
- Limited dorsiflexion and a tight Achilles tendon
- A limp may be present or there may be a preference for toe walking
- Pain is usually worse when barefoot on hard surfaces and with stair climbing
- Treatment:[1]
- Conservative measures are the first choice
- Physiotherapy
- Rest from offending activity
- Ice after activity
- Deep friction massage of the arch and insertion
- Shoe inserts or Introduction to Orthotics and night splints
- Extracorporeal shock-wave therapy[19] , botulinum toxin A, autologous platelet-rich plasma, dextrose prolotherapy, or steroid injections
- Advanced and invasive techniques should be combined with conservative therapy
- Surgery should be the last option if this process has become chronic and other less invasive therapies have failed
- Educate the dancer on proper stretching and rehabilitation of the: plantar fascia; Achilles' tendon; gastrocnemius and soleus
- Ballet specific considerations:[1]
- Biomechanics check: plié, developpe and gait
- Stretch: iliopsoas, quadriceps, adductors, calf muscles
- Strengthen: gluteal muscles, abductors, deep rotators
- Specific rehabilitation: chair straight leg bridges, straight leg heel raises on stairs, ankle / toe rockers, strapping
For more specific physiotherapy treatment options please see the Plantar Fasciitis page.
Foot and Ankle Care[edit | edit source]
- Pointe work should always be progressed slowly and only once the individual has been assessed
- Foot alignment should always be monitored
- Balance exercises, intrinsic foot exercises and calf stretching and strengthening should be included in training
- Dancers should be encouraged to walk with a normal of angle of gait, which allows off-loading of the hip rotators (i.e., not walking in a turnout position)[1]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 Green-Smerdon M. Dance Injuries of the Ankle and Foot Course. Plus , 2022.
- ↑ 2.0 2.1 2.2 Cardoso AA, Reis NM, Marinho AP, Vieira MD, Boing L, Guimarães AC. Injuries in professional dancers: a systematic review. Revista Brasileira de Medicina do Esporte. 2017 Nov;23:504-9.
- ↑ 3.0 3.1 3.2 Skwiot M, Śliwiński Z, Żurawski A, Śliwiński G. Effectiveness of physiotherapy interventions for injury in ballet dancers: A systematic review. PLoS one. 2021 Jun 24;16(6):e0253437.
- ↑ 4.0 4.1 Biernacki JL, Stracciolini A, Fraser J, Micheli LJ, Sugimoto D. Risk factors for lower-extremity injuries in female ballet dancers: a systematic review. Clinical journal of sport medicine. 2021 Mar 1;31(2):e64-79.
- ↑ Campbell RS, Lehr ME, Livingston A, McCurdy M, Ware JK. Intrinsic modifiable risk factors in ballet dancers: Applying evidence based practice principles to enhance clinical applications. Physical Therapy in Sport. 2019 Jul 1;38:106-14.
- ↑ Fuller M, Moyle GM, Hunt AP, Minett GM. Ballet and contemporary dance injuries when transitioning to full-time training or professional level dance: a systematic review. Journal of Dance Medicine & Science. 2019 Sep 1;23(3):112-25.
- ↑ 7.0 7.1 En Pointe: What Ballet Dancers Should Know About Injury Prevention
- ↑ Rietveld AB. Performing arts medicine with a focus on Relevé in Dancers. Leiden University; 2017 Nov 28.
- ↑ 9.0 9.1 Khurana A, Singh I, Singh MS. Is anterior and posterior ankle impingement under-diagnosed? A review. Journal of Arthroscopic Surgery and Sports Medicine. 2021 Jan 10;2(1):58-65.
- ↑ 10.0 10.1 10.2 Batenhorst EZ. A Dancer’s View: Analysis and Prevention of Common Dance Injuries. 2020
- ↑ Grigoryev K. Comparison of Open and Endoscopic Surgical Procedures as a Treatment of Posterior Ankle Impingement Syndrome in Ballet Dancers: A Meta-Analysis (Doctoral dissertation, California State University, Fresno).
- ↑ 12.0 12.1 Bodini BD, Lucenteforte G, Serafin P, Barone L, Vitale JA, Serafin A, Sansone V, Negrini F. Do grade II ankle sprains have chronic effects on the functional ability of ballet dancers performing single-leg flat-foot stance? An observational cross-sectional study. Applied Sciences. 2020 Jan;10(1):155.
- ↑ 13.0 13.1 13.2 13.3 13.4 Mira NO, Marulanda AF, Peña AC, Torres DC, Orrego JC. Study of ballet dancers during cou-de-pied derrière with demi-plié to piqué arabesque. Journal of Dance Medicine & Science. 2019 Dec 15;23(4):150-8.
- ↑ 14.0 14.1 Ogilvie-Harris DJ, Carr MM, Fleming PJ. The foot in ballet dancers: the importance of second toe length. Foot & ankle international. 1995 Mar;16(3):144-7.
- ↑ Wentzell M. Conservative management of a chronic recurrent flexor hallucis longus stenosing tenosynovitis in a pre-professional ballet dancer: a case report. The Journal of the Canadian Chiropractic Association. 2018 Aug;62(2):111.
- ↑ Anderson MR, Ho BS, Baumhauer JF. Current concepts review: hallux rigidus. Foot & Ankle Orthopaedics. 2018 Jun 7;3(2):2473011418764461.
- ↑ Carpenter B, Gentile M, Hagenbucher JR. Functional hallux rigidus in high level athletes: Arthroscopic repair by flexor hallucis longus debridement. Journal of the International Foot & Ankle Foundation. 2022;1(1).
- ↑ Datir A, Bell D. Jones fracture. Reference article, Radiopaedia.org [cited 18 May 2022]. Available from: https://radiopaedia.org/articles/jones-fracture-1
- ↑ Rhim HC, Kwon J, Park J, Borg-Stein J, Tenforde AS. A Systematic Review of Systematic Reviews on the Epidemiology, Evaluation, and Treatment of Plantar Fasciitis. Life. 2021 Dec;11(12):1287.