Congestive Heart Failure - Pharmacotherapy: Difference between revisions
Kim Jackson (talk | contribs) m (Adding headings) |
(page link update) |
||
| (21 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User: | <div class="editorbox"> '''Original Editor '''- [[User:Lauren Pulliam Southern|Lauren Pulliam Southern]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Introduction == | == Introduction == | ||
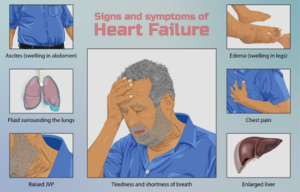
[[File:Heart failure.png|thumb|Heart Failure]] | |||
The goal of therapy for chronic congestive heart failure ([[Congestive Heart Failure|CHF]]) is to improve symptom management and [[Quality of Life|quality of life]], decrease hospitalisations, and decrease overall mortality associated with this disease. | |||
The goal of pharmacologic therapy is to give all indicated agents rather than single agents because the aggregate effect of these therapies is better than monotherapy from any of the agents<ref name=":0">Malik A, Brito D, Vaqar S, Chhabra L, Doerr C. [https://www.ncbi.nlm.nih.gov/books/NBK430873/ Congestive Heart Failure (Nursing)]. StatPearls [Internet]. 2021 Sep 24.Available: https://www.ncbi.nlm.nih.gov/books/NBK430873/<nowiki/>(accessed 8.4.2022)</ref>. | |||
== Pharmacological Management of Heart Failure == | |||
[[File:CR.jpg|right|frameless]] | |||
Drugs used in heart failure include those used to initially manage mild to moderate failure and those used more commonly in severe to very severe conditions. | |||
First Agents Used: | |||
# [[ACE Inhibitors: Congestive Heart Failure|ACE Inhibitors]]: work by increasing vasodilation and decreasing workload of the heart in patients with CHF. | |||
#[[Diuretics]]: promote the removal from the body of excess water, salts, poisons, and accumulated metabolic products, such as urea. See also [[Aldosterone Receptor Antagonist Diuretics in the treatment of congestive heart failure|Aldosterone Receptor Antagonists]] | |||
#[[Glycosides and Congestive Heart Failure]]: a class of drugs that includes digoxin, digitoxin and ouabain. Such agents increase the force of contraction of the heart (ie a positive inotropic action) which underlies their use in some cases of heart failure<ref>Pharmacology education Glycosides Available:http://www.pharmacologyeducation.org/positive-inotropic-drugs-cardiac-glycosides-digoxin (accessed 3.6.2021)</ref>. | |||
#[[Beta-Blockers]] (mild-to-moderate disease): decrease the excessive activity of the [[Sympathetic Nervous System|sympathetic nervous system]] which is characteristic of CHF.(mild-to-moderate disease) | |||
Selection of agents and their combinations depend on initial clinical state and on patient responsiveness to initial therapy | |||
Additional Agents: | |||
# More aggressive diuretic therapy eg Loop diuretics such as Furosemide (Lasix), one of the most commonly used drugs in the treatment [[Oedema Assessment|edema]] caused by congestive heart failure (CHF). | |||
#[[Vasodilators]] | |||
# Parenteral inotropic agents (dobutamine). There are very few options for patients in the end stages of CHF. Home inotropic infusions offer a nonsurgical option to improve both patients' symptoms and quality of life. The use of these medications requires advanced planning as well as symptom management and device management. They can be safely used throughout the continuum of care as pediatric/adult “bridges to transplant” through [[Physiotherapy in Palliative Care|hospice care]].<ref>Lyons MG, Carey L. [https://journals.lww.com/homehealthcarenurseonline/Fulltext/2013/04000/Parenteral_Inotropic_Therapy_in_the_Home__An.4.aspx Parenteral inotropic therapy in the home: an update for home care and hospice.] Home Healthcare Now. 2013 Apr 1;31(4):190-204.Available: https://journals.lww.com/homehealthcarenurseonline/Fulltext/2013/04000/Parenteral_Inotropic_Therapy_in_the_Home__An.4.aspx<nowiki/>(accessed 3.6.2021)</ref> | |||
Selection of agents and their combinations depend on initial clinical state and on patient responsiveness to initial therapy<ref>Pharmacology 2020 | |||
Chapter 10: Pharmacological Management of Congestive Heart Failure Available:https://www.pharmacology2000.com/Cardio/CHF/chfobj1.htm (accessed 3.6.2021)</ref>. | |||
==== | An implantable [[Cardioversion|cardioverter]]-defibrillator (ICD) is indicated for primary prevention of sudden cardiac death in patients with HF who have an LVEF of less than or equal to 35%<ref name=":0" />. | ||
==== Conclusion ==== | |||
As part of an interdisciplinary team, it is also essential that physical therapists be knowledgeable regarding the pharmacological treatment of CHF. The drugs used to manage CHF work by increasing cardiac contractility or decreasing cardiac workload. | |||
# These pharmacological effects may potentially allow for drug therapy and exercise therapy to have the mutually reinforcing benefits of increasing exercise tolerance and strengthening cardiac function. See [[Cardiac Rehabilitation|cardiac rehabilitation]] | |||
# Despite these potential benefits, the drugs used to treat CHF may also cause serious side effects including dizziness, nausea, [[Heart Arrhythmias|arrhythmias]], fatigue, and weakness. | |||
Knowledge of these side effects will allow the therapist to consider the response to exercise prescription and other modalities in the context of the patient’s pharmacotherapy. Early recognition of these symptoms may prevent development of serious complications or even death. | |||
== References == | |||
<references /> | <references /> | ||
[[Category:Cardiopulmonary]] | [[Category:Cardiopulmonary]] | ||
[[Category:Pharmacology for Cardiovascular Disease]] | [[Category:Pharmacology for Cardiovascular Disease]] | ||
[[Category:Older People/Geriatrics]] | |||
[[Category:Pharmacology]] | |||
[[Category:Winston-Salem State University Pharmacology Project]] | |||
Latest revision as of 06:55, 8 February 2023
Introduction[edit | edit source]
The goal of therapy for chronic congestive heart failure (CHF) is to improve symptom management and quality of life, decrease hospitalisations, and decrease overall mortality associated with this disease.
The goal of pharmacologic therapy is to give all indicated agents rather than single agents because the aggregate effect of these therapies is better than monotherapy from any of the agents[1].
Pharmacological Management of Heart Failure[edit | edit source]
Drugs used in heart failure include those used to initially manage mild to moderate failure and those used more commonly in severe to very severe conditions.
First Agents Used:
- ACE Inhibitors: work by increasing vasodilation and decreasing workload of the heart in patients with CHF.
- Diuretics: promote the removal from the body of excess water, salts, poisons, and accumulated metabolic products, such as urea. See also Aldosterone Receptor Antagonists
- Glycosides and Congestive Heart Failure: a class of drugs that includes digoxin, digitoxin and ouabain. Such agents increase the force of contraction of the heart (ie a positive inotropic action) which underlies their use in some cases of heart failure[2].
- Beta-Blockers (mild-to-moderate disease): decrease the excessive activity of the sympathetic nervous system which is characteristic of CHF.(mild-to-moderate disease)
Selection of agents and their combinations depend on initial clinical state and on patient responsiveness to initial therapy
Additional Agents:
- More aggressive diuretic therapy eg Loop diuretics such as Furosemide (Lasix), one of the most commonly used drugs in the treatment edema caused by congestive heart failure (CHF).
- Vasodilators
- Parenteral inotropic agents (dobutamine). There are very few options for patients in the end stages of CHF. Home inotropic infusions offer a nonsurgical option to improve both patients' symptoms and quality of life. The use of these medications requires advanced planning as well as symptom management and device management. They can be safely used throughout the continuum of care as pediatric/adult “bridges to transplant” through hospice care.[3]
Selection of agents and their combinations depend on initial clinical state and on patient responsiveness to initial therapy[4].
An implantable cardioverter-defibrillator (ICD) is indicated for primary prevention of sudden cardiac death in patients with HF who have an LVEF of less than or equal to 35%[1].
Conclusion[edit | edit source]
As part of an interdisciplinary team, it is also essential that physical therapists be knowledgeable regarding the pharmacological treatment of CHF. The drugs used to manage CHF work by increasing cardiac contractility or decreasing cardiac workload.
- These pharmacological effects may potentially allow for drug therapy and exercise therapy to have the mutually reinforcing benefits of increasing exercise tolerance and strengthening cardiac function. See cardiac rehabilitation
- Despite these potential benefits, the drugs used to treat CHF may also cause serious side effects including dizziness, nausea, arrhythmias, fatigue, and weakness.
Knowledge of these side effects will allow the therapist to consider the response to exercise prescription and other modalities in the context of the patient’s pharmacotherapy. Early recognition of these symptoms may prevent development of serious complications or even death.
References[edit | edit source]
- ↑ 1.0 1.1 Malik A, Brito D, Vaqar S, Chhabra L, Doerr C. Congestive Heart Failure (Nursing). StatPearls [Internet]. 2021 Sep 24.Available: https://www.ncbi.nlm.nih.gov/books/NBK430873/(accessed 8.4.2022)
- ↑ Pharmacology education Glycosides Available:http://www.pharmacologyeducation.org/positive-inotropic-drugs-cardiac-glycosides-digoxin (accessed 3.6.2021)
- ↑ Lyons MG, Carey L. Parenteral inotropic therapy in the home: an update for home care and hospice. Home Healthcare Now. 2013 Apr 1;31(4):190-204.Available: https://journals.lww.com/homehealthcarenurseonline/Fulltext/2013/04000/Parenteral_Inotropic_Therapy_in_the_Home__An.4.aspx(accessed 3.6.2021)
- ↑ Pharmacology 2020 Chapter 10: Pharmacological Management of Congestive Heart Failure Available:https://www.pharmacology2000.com/Cardio/CHF/chfobj1.htm (accessed 3.6.2021)