Manual Lymphatic Drainage: Difference between revisions
No edit summary |
m (link corrected) |
||
| (47 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox">
'''Original Editor''' - [[User:Chew Chee Boon|Chew Chee Boon]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}
</div> | ||
'''Original Editor '''- | == Description == | ||
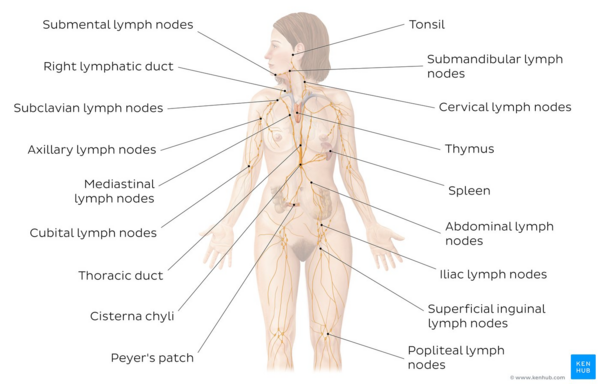
[[File:Lymphatic system - Kenhub.png|alt=Overview of the lymphatic system|right|frameless|600x600px|Overview of the lymphatic system]] | |||
Manual Lymph drainage (MLD), is a technique developed by the Vodders (Dr. Emil Vodder and his wife, Estrid) in 1936 in Paris for treatment of swollen lymph nodes<ref>Dr Vodder School International. Manual Lymph Drainage History (MLD). Available from: https://vodderschool.com/manual_lymph_drainage_history (Accessed 3 September 2020)</ref>. | |||
Lymphatic diseases, especially [[Lymphoedema|lymphedema]], represent a serious problem in the health community<ref name=":0">Tzani I, Tsichlaki M, Zerva E, Papathanasiou G, Dimakakos E. [https://www.researchgate.net/publication/326301004_Physiotherapeutic_rehabilitation_of_lymphedema_State-of-the-art Physiotherapeutic rehabilitation of lymphedema]: State-of-the-art. Lymphology. 2018 Jul 2;51(1):1-2.</ref>. | |||
</ | |||
MLD is a light, skin-stretching massage that helps promote the movement of lymphatic fluid out of the swollen limb. It should not be confused with a traditional massage. MLD is specifically focused on the lymph vessels to help the flow of lymphatic fluid. Therapy is applied to your unaffected areas first, making it possible for the fluid to move out of the affected area, or “decongest” the region. MLD helps open the remaining functioning lymph collectors and move protein and fluid into them, as well as to help speed up lymph fluid flow through the lymphatics. | |||
Deep breathing techniques called [[Diaphragmatic Breathing Exercises|diaphragmatic breathing]] are usually done at the beginning and end of a therapy session to help open the deep lymphatic pathways. It’s not only relaxing, but it helps increase movement of fluid toward the [[Anatomy of the Human Heart|heart]]<ref>Lymph care [https://www.lymphcareusa.com/patient/therapy-solutions/complete-decongestive-therapy/manual-lymphatic-drainage-mld.html MLD] Available from:https://www.lymphcareusa.com/patient/therapy-solutions/complete-decongestive-therapy/manual-lymphatic-drainage-mld.html (last accessed 17.8.2020)</ref>. | |||
Image: Overview of the lymphatic system<ref > Overview of the lymphatic system image - © Kenhub https://www.kenhub.com/en/study/lymphatic-system</ref> | |||
MLD: | |||
* | * The intention behind MLD is to augment the rhythmic contractions and stimulate the lymph nodes to improve their activity in order to reroute stagnant [[Lymphatic System|lymphatic]] fluid<ref name=":0" />. | ||
* | * MLD is comprised of four main strokes: stationary circles, scoop technique, pump technique, and rotary technique<ref name=":0" />. | ||
* It is effective as a preventative and postoperative rehabilitation treatment<ref name=":0" />. | |||
* | * MLD is a a key component [[Complete Decongestive Therapy (CDT)|Complete Decongestive Therapy]] (CDT)<ref name="best practice" />. It shows optimal results when it is combined with the other CDT elements<ref name=":0" />. | ||
* MLD also increases [[blood]] flow in deep and superficial veins<ref name="venous ins">Crisóstomo RS, Candeias MS, Armada-da-Silva PA. Venous flow during manual lymphatic drainage applied to different regions of the lower extremity in people with and without chronic venous insufficiency: a cross-sectional study.Physiotherapy. 2016 Feb 1. pii: S0031-9406(16)00023-7.</ref>. | |||
* MLD may be useful in conditions such as post-traumatic and post-surgical edema<ref name=":0" /> and [https://www.physio-pedia.com/The_Role_of_the_Physiotherapist_in_Palliative_Care_for_People_With_Lymphoedema palliative care]<ref name=":0" />. | |||
== | == Techniques == | ||
There are various techniques for MLD including the Vodder, Földi, Leduc or Casley-Smith methods. | |||
MLD is recommended as a component of [[Complete Decongestive Therapy (CDT)|CDT,]] but is often used in combination with other treatments<ref name=":0" />. MLD in isolation is effective but a combination of the parts of CDT is optimal<ref name=":0" />. CDT has been shown to be effective in reducing lymphedema volume and improving quality of life patient mobility<ref name=":0" />. | |||
It often takes many hours of training in MLD, combined with years of hands-on experience, for a lymphedema therapist to become truly skilled. | |||
The most appropriate techniques, optimal frequency and indications for MLD, as well as the benefits of treatment, all remain to be clarified, but the different methods have several aspects in common, including the following<ref name="best practice">[https://www.woundsinternational.com/resources/details/best-practice-for-the-management-of-lymphoedema-an-international-consensus Lymphoedema Framework. Best Practice for the Management of Lymphoedema. International consensus.] London: MEP Ltd, 2006.</ref> : | |||
''' | *Usually performed with the patient in the lying position | ||
*Starts and ends with deep [[Diaphragmatic Breathing Exercises|diaphragmatic breathing]] | |||
*The unaffected lymph nodes and region of the body are treated first | |||
*Moves proximal to distal to drain the affected areas | |||
*Slow and rhythmical movements | |||
*Uses gentle pressure - this is essential | |||
The video below gives a very brief explanation of Manual Lymphatic Drainage | |||
{{#ev:youtube|dT6rAL4-D14 | 300}}<ref>National Lymphedema Network. Manual Lymph Drainage (MLD). Available from: http://www.youtube.com/watch?v=dT6rAL4-D14[last accessed 01/04/2022]</ref> | |||
'''Different Approaches'''<ref name="Williams">Williams A. [https://www.researchgate.net/profile/Anne-Williams-4/publication/44683866_Manual_lymphatic_drainage_Exploring_the_history_and_evidence_base/links/547c94eb0cf2cfe203c1db71/Manual-lymphatic-drainage-Exploring-the-history-and-evidence-base.pdf Manual lymphatic drainage: exploring the history and evidence base]. British Journal of Community Nursing. 2010 Apr;15(Sup3):S18-24.</ref> | |||
* Vodder - Different kinds of hand motions are used on the skin depending on the part of the body being treated. It also includes edema movements at fibrotic areas. The different motions include "pump", "scoop", "stationery circle", "rotary" and "thumb circle". | |||
* Foldi - Based on the Vodder technique, this method lays emphasis on a "thrust" and "relaxation" phase. 'Encircling strokes' are included in this approach. | |||
* Casley-Smith - This method involves use of gentle and slow effleurage movements with the side of the hand. The effleurage movements are performed over the "watershed" areas between lymphotomes. | |||
* Leduc - It involves use of "call up" (or enticing) and "reabsorption" movements which reflects how lymph is absorbed first in the initial lymphatics and then into larger lymphatics. | |||
== Indications == | |||
[[File:Lymphoedema red leg.png|right|frameless]]MLD is indicated in primary or secondary [[Lymphatic Obstruction (Lymphedema)|lymphedema ]]<nowiki/>in the following situations: | |||
*When there is swelling at a limb's root<ref name="best practice" /> | |||
*When trunk and midline edema is present<ref name="best practice" /> | |||
*When comfort and pain relief is required but other therapies are no longer appropriate - palliative<ref name="best practice" /> | |||
*As an adjunct to pain management<ref name="best practice" /> | |||
*As a preventative treatment<ref name=":0" /> | |||
*Chronic venous insufficiency <ref name="venous ins" /> | |||
MLD may also be helpful in the below situations: | |||
*It may be used as a complement treatment for patients with psychological stress. <ref>Jung-Myo S, Sung-Joong K. Manual Lymph Drainage Attenuates Frontal EEG Asymmetry in Subjects with Psychological Stress: A Preliminary Study. J Phys Ther Sci. 2014 Apr; 26(4): 529–531.</ref><ref>Shim JM, Yeun YR, Kim HY, Kim SJ. [https://www.jstage.jst.go.jp/article/jpts/29/3/29_jpts-2016-900/_pdf Effects of manual lymph drainage for abdomen on the brain activity of subjects with psychological stress]. Journal of physical therapy science. 2017;29(3):491-4.</ref> | |||
*It (craniocervical MLD) may be effective for reducing intracranial pressure in people with severe cerebral diseases.<ref>Roth C, Stitz H, Roth C, Ferbert A, Deinsberger W, Pahl R et. al. [https://www.researchgate.net/profile/Holger-Engel/publication/303687614_Craniocervical_manual_lymphatic_drainage_and_its_impact_on_intracranial_pressure_-_a_pilot_study/links/5c66682d45851582c3e98103/Craniocervical-manual-lymphatic-drainage-and-its-impact-on-intracranial-pressure-a-pilot-study.pdf Craniocervical manual lymphatic drainage and its impact on intracranial pressure - a pilot study]. Eur J Neurol. 2016 Sep;23(9):1441-6.</ref> | |||
== Contraindications == | |||
= | '''General contraindications'''<ref name="best practice" />''':''' | ||
* Acute cellulitis/erysipelas | |||
* Severe cardiac insufficiency | |||
* Hepatic cirrhosis with abdominal fluid (ascites) | |||
* Unstable hypertension | |||
* Renal failure | |||
* Untreated tuberculosis or malaria | |||
* Superior vena cava obstruction | |||
= | '''Local contraindications'''<ref name="best practice" />''':''' | ||
*Untreated thyroid dysfunction | |||
*Metastases | |||
*Primary tumours | |||
== Principles of MLD == | |||
[ | *The [[Integumentary System|skin]] is stretched in specific directions using hand movements to promote variations in interstitial pressure without the use of oils<ref name=":0" /><ref name="Williams" />. | ||
*Slow repetitive movements are used which incorporate a resting phase to allow the skin to return to its normal position<ref name=":0" /><ref name="Williams" />. | |||
== | *The pressure is varied according to the underlying tissue with the aim to promote lymphatic drainage<ref name="Williams" />. The pressure however is softer than in traditional massage<ref name="Williams" />. | ||
*Areas of fibrosclerosis are treated using deeper and firmer movements in combination with compression therapy<ref name="Williams" />. | |||
= | *The lymphatic drainage starts centrally and proximally<ref name=":0" /><ref name="Williams" /> with treatments usually starting around the neck<ref name="Williams" />. | ||
< | |||
< | |||
*Functional and healthy lymph nodes are treated first<ref name="Williams" />. | |||
< | *There is emphasis on treatment of anterior and posterior trunk in the early phases before the swollen limb is treated<ref name="Williams" />. | ||
< | *Breathing techniques are combined with pressure by the therapist's hands to promote drainage of deep abdominal lymph nodes and vessels<ref name="Williams" />. | ||
</ | |||
*Limb mobilization and relaxation techniques are often combined with MLD.<ref name="Williams" /> | |||
== Physiotherapist-administered MLD == | |||
Physiotherapy for patients with lymphedema can only be successful if the physiotherapist is specifically educated, trained and experienced in each method<ref name=":0" />. | |||
It is often given as part of [[Complete Decongestive Therapy (CDT)|Complete Decongestive Therapy]] (CDT) which has two phases - phase I and II<ref name=":0" />. MLD is performed in phase I and II, but phase II has more MLD<ref name=":0" />. The two phases consist of the following: | |||
'''Phase I''' | |||
* MLD<ref name=":0" /> | |||
* lymphological compression bandages<ref name=":0" /> | |||
* remedial exercises<ref name=":0" /> | |||
* physiotherapy<ref name=":0" /><ref name="best practice" /> where patients are struggling with mobility or joint mobility/function<ref name="best practice" /> | |||
* Education regarding self-management and skin care<ref name=":0" /> | |||
'''Phase II''' | |||
* MLD<ref name=":0" /> | |||
* wearing of fitted compression stockings<ref name=":0" /> | |||
== Resources == | |||
* Browse videos on this page regarding techniques on [[Lymphoedema|Lymphedema]] management. | |||
* [https://vodderschool.com/manual_lymph_drainage_history Manual Lymphatic Drainage (MLD) History] | |||
== References == | == References == | ||
<references /> | |||
[[Category:Manual_Therapy]] | |||
[[Category:Palliative_Care]] | |||
[[Category:Procedures]] | |||
Latest revision as of 14:30, 9 January 2023
Description[edit | edit source]
Manual Lymph drainage (MLD), is a technique developed by the Vodders (Dr. Emil Vodder and his wife, Estrid) in 1936 in Paris for treatment of swollen lymph nodes[1].
Lymphatic diseases, especially lymphedema, represent a serious problem in the health community[2].
MLD is a light, skin-stretching massage that helps promote the movement of lymphatic fluid out of the swollen limb. It should not be confused with a traditional massage. MLD is specifically focused on the lymph vessels to help the flow of lymphatic fluid. Therapy is applied to your unaffected areas first, making it possible for the fluid to move out of the affected area, or “decongest” the region. MLD helps open the remaining functioning lymph collectors and move protein and fluid into them, as well as to help speed up lymph fluid flow through the lymphatics.
Deep breathing techniques called diaphragmatic breathing are usually done at the beginning and end of a therapy session to help open the deep lymphatic pathways. It’s not only relaxing, but it helps increase movement of fluid toward the heart[3].
Image: Overview of the lymphatic system[4]
MLD:
- The intention behind MLD is to augment the rhythmic contractions and stimulate the lymph nodes to improve their activity in order to reroute stagnant lymphatic fluid[2].
- MLD is comprised of four main strokes: stationary circles, scoop technique, pump technique, and rotary technique[2].
- It is effective as a preventative and postoperative rehabilitation treatment[2].
- MLD is a a key component Complete Decongestive Therapy (CDT)[5]. It shows optimal results when it is combined with the other CDT elements[2].
- MLD also increases blood flow in deep and superficial veins[6].
- MLD may be useful in conditions such as post-traumatic and post-surgical edema[2] and palliative care[2].
Techniques[edit | edit source]
There are various techniques for MLD including the Vodder, Földi, Leduc or Casley-Smith methods.
MLD is recommended as a component of CDT, but is often used in combination with other treatments[2]. MLD in isolation is effective but a combination of the parts of CDT is optimal[2]. CDT has been shown to be effective in reducing lymphedema volume and improving quality of life patient mobility[2].
It often takes many hours of training in MLD, combined with years of hands-on experience, for a lymphedema therapist to become truly skilled.
The most appropriate techniques, optimal frequency and indications for MLD, as well as the benefits of treatment, all remain to be clarified, but the different methods have several aspects in common, including the following[5] :
- Usually performed with the patient in the lying position
- Starts and ends with deep diaphragmatic breathing
- The unaffected lymph nodes and region of the body are treated first
- Moves proximal to distal to drain the affected areas
- Slow and rhythmical movements
- Uses gentle pressure - this is essential
The video below gives a very brief explanation of Manual Lymphatic Drainage
Different Approaches[8]
- Vodder - Different kinds of hand motions are used on the skin depending on the part of the body being treated. It also includes edema movements at fibrotic areas. The different motions include "pump", "scoop", "stationery circle", "rotary" and "thumb circle".
- Foldi - Based on the Vodder technique, this method lays emphasis on a "thrust" and "relaxation" phase. 'Encircling strokes' are included in this approach.
- Casley-Smith - This method involves use of gentle and slow effleurage movements with the side of the hand. The effleurage movements are performed over the "watershed" areas between lymphotomes.
- Leduc - It involves use of "call up" (or enticing) and "reabsorption" movements which reflects how lymph is absorbed first in the initial lymphatics and then into larger lymphatics.
Indications[edit | edit source]
MLD is indicated in primary or secondary lymphedema in the following situations:
- When there is swelling at a limb's root[5]
- When trunk and midline edema is present[5]
- When comfort and pain relief is required but other therapies are no longer appropriate - palliative[5]
- As an adjunct to pain management[5]
- As a preventative treatment[2]
- Chronic venous insufficiency [6]
MLD may also be helpful in the below situations:
- It may be used as a complement treatment for patients with psychological stress. [9][10]
- It (craniocervical MLD) may be effective for reducing intracranial pressure in people with severe cerebral diseases.[11]
Contraindications[edit | edit source]
General contraindications[5]:
- Acute cellulitis/erysipelas
- Severe cardiac insufficiency
- Hepatic cirrhosis with abdominal fluid (ascites)
- Unstable hypertension
- Renal failure
- Untreated tuberculosis or malaria
- Superior vena cava obstruction
Local contraindications[5]:
- Untreated thyroid dysfunction
- Metastases
- Primary tumours
Principles of MLD[edit | edit source]
- The skin is stretched in specific directions using hand movements to promote variations in interstitial pressure without the use of oils[2][8].
- Slow repetitive movements are used which incorporate a resting phase to allow the skin to return to its normal position[2][8].
- The pressure is varied according to the underlying tissue with the aim to promote lymphatic drainage[8]. The pressure however is softer than in traditional massage[8].
- Areas of fibrosclerosis are treated using deeper and firmer movements in combination with compression therapy[8].
- The lymphatic drainage starts centrally and proximally[2][8] with treatments usually starting around the neck[8].
- Functional and healthy lymph nodes are treated first[8].
- There is emphasis on treatment of anterior and posterior trunk in the early phases before the swollen limb is treated[8].
- Breathing techniques are combined with pressure by the therapist's hands to promote drainage of deep abdominal lymph nodes and vessels[8].
- Limb mobilization and relaxation techniques are often combined with MLD.[8]
Physiotherapist-administered MLD[edit | edit source]
Physiotherapy for patients with lymphedema can only be successful if the physiotherapist is specifically educated, trained and experienced in each method[2].
It is often given as part of Complete Decongestive Therapy (CDT) which has two phases - phase I and II[2]. MLD is performed in phase I and II, but phase II has more MLD[2]. The two phases consist of the following:
Phase I
- MLD[2]
- lymphological compression bandages[2]
- remedial exercises[2]
- physiotherapy[2][5] where patients are struggling with mobility or joint mobility/function[5]
- Education regarding self-management and skin care[2]
Phase II
Resources[edit | edit source]
- Browse videos on this page regarding techniques on Lymphedema management.
- Manual Lymphatic Drainage (MLD) History
References[edit | edit source]
- ↑ Dr Vodder School International. Manual Lymph Drainage History (MLD). Available from: https://vodderschool.com/manual_lymph_drainage_history (Accessed 3 September 2020)
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 2.20 2.21 2.22 2.23 Tzani I, Tsichlaki M, Zerva E, Papathanasiou G, Dimakakos E. Physiotherapeutic rehabilitation of lymphedema: State-of-the-art. Lymphology. 2018 Jul 2;51(1):1-2.
- ↑ Lymph care MLD Available from:https://www.lymphcareusa.com/patient/therapy-solutions/complete-decongestive-therapy/manual-lymphatic-drainage-mld.html (last accessed 17.8.2020)
- ↑ Overview of the lymphatic system image - © Kenhub https://www.kenhub.com/en/study/lymphatic-system
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Lymphoedema Framework. Best Practice for the Management of Lymphoedema. International consensus. London: MEP Ltd, 2006.
- ↑ 6.0 6.1 Crisóstomo RS, Candeias MS, Armada-da-Silva PA. Venous flow during manual lymphatic drainage applied to different regions of the lower extremity in people with and without chronic venous insufficiency: a cross-sectional study.Physiotherapy. 2016 Feb 1. pii: S0031-9406(16)00023-7.
- ↑ National Lymphedema Network. Manual Lymph Drainage (MLD). Available from: http://www.youtube.com/watch?v=dT6rAL4-D14[last accessed 01/04/2022]
- ↑ 8.00 8.01 8.02 8.03 8.04 8.05 8.06 8.07 8.08 8.09 8.10 8.11 Williams A. Manual lymphatic drainage: exploring the history and evidence base. British Journal of Community Nursing. 2010 Apr;15(Sup3):S18-24.
- ↑ Jung-Myo S, Sung-Joong K. Manual Lymph Drainage Attenuates Frontal EEG Asymmetry in Subjects with Psychological Stress: A Preliminary Study. J Phys Ther Sci. 2014 Apr; 26(4): 529–531.
- ↑ Shim JM, Yeun YR, Kim HY, Kim SJ. Effects of manual lymph drainage for abdomen on the brain activity of subjects with psychological stress. Journal of physical therapy science. 2017;29(3):491-4.
- ↑ Roth C, Stitz H, Roth C, Ferbert A, Deinsberger W, Pahl R et. al. Craniocervical manual lymphatic drainage and its impact on intracranial pressure - a pilot study. Eur J Neurol. 2016 Sep;23(9):1441-6.