Burn Injury Management Considerations for Rehabilitation Professionals: Difference between revisions
Carin Hunter (talk | contribs) No edit summary |
Carin Hunter (talk | contribs) No edit summary |
||
| Line 85: | Line 85: | ||
** If no adequate first aid was administered, suspect deeper burn injury | ** If no adequate first aid was administered, suspect deeper burn injury | ||
* Falls | * Falls | ||
** Is there any indication that the patient fell? | ** Is there any indication that the patient fell? | ||
** What height did they fall from? | ** What height did they fall from? | ||
** Suspect a possible head injury, sprain or fracture | ** Suspect a possible head injury, sprain or fracture | ||
* Electrical injury | * Electrical injury | ||
** What voltage was involved? | ** What voltage was involved? | ||
Revision as of 11:42, 16 June 2022
Top Contributors - Jess Bell, Carin Hunter, Kim Jackson, Stacy Schiurring and Robin Tacchetti
Burn Assessment[edit | edit source]
When treating a patient with a burn, the first step is an accurate assessment. The time spent on an assessment will not only optimise their immediate treatment and minimise any long term injury they might be vulnerable to, but it will also help the patient to achieve their highest functional level. A complete assessment also will increase the chance of patient compliance as it offers the multidisciplinary team the opportunity to remind themselves of the patients long term goals and align their therapy to these objectives. A burn injury in unique to every situation and patient, and a clear assessment will help the team to be united in their efforts. The multidiciplinary team should be aware of the importance of an early and adequate assessment of the burn patients for optimal functional and cosmetic outcomes to minimise the impact of the trauma long term. For continuity it is helpful for the Initial Assessment to be available to all further disciplines conducting their assessments, and all these assessments be forwarded onto the rehabilitation setting and ideally, into the community setting. This continuity of information will lessen the frustration of the patient having to re-explain the story and it insures the information transferred is as accurate as possible.
Flow chart illustrating the assessment and management of the burn
Short Term Goals:
- Prevent respiratory complications
- Control Oedema
- Maintain Joint ROM
- Maintain Strength
- Prevent Excessive Scarring
Risk Factors:
- Injury Factors:
- Inhalation injury
- Burn area - systemic inflammatory reaction syndrome involving the lungs
- Depth of burn
- Scarring
- Patient Factors
- Reduced ambulation and mobility
- Increased bed rest
- Increased pain
- Pre-existing co-morbidities
- Treatment Factors
- Skin reconstruction surgery
- Invasive monitoring and procedures
- Management in critical care
Subjective Assessment[edit | edit source]
The following pieces of information should be included in the Subjective Assessment:
- Inhalation injury
- Total Body Surface Area (TBSA)
- Burn Type and Depth
- Burn Site and Impact
- Present History
- Any surgical or medical management
- Past History (Including Medical/ Drug)
- Social History
1. Inhalation Injury[edit | edit source]
During the subjective assessment, if the patient was in an enclosed space or is presenting with a reduced level of consciousness[1], it is imperative to make a note to conduct, or speak to the team member who can conduct, an Inhalation Injury Examination which will allow treatment to commence as soon as possible. When conducting a Subjective Assessment, the clinician should note any physical signs of inhalation injury such as charring around the mouth and nostrils.[2]
(2 - ANZBA 2007; British Burn Association 2005; 1 - Eisenmann-Klein 2010)
2. Total Body Surface Area[edit | edit source]
There are many methods on conducting a Total Body Surface Area (TBSA) assessment. The most accurate method is the Rules of Nines and Lund and Brower method. Another commonly used method is the Palmer Surface Method, whereby the patients palm size, (representing 1% TBSA) is used to estimate the total burns coverage. Please note, when assessing the burnt area, oedema should not be included.
When conducting the TBSA assessment, there are two main considerations:
- The Parkland Formula for fluid resuscitation
- When a patient has more than 20–25% TBSA a systemic inflammatory reaction is seen which is known to affect all body organs. This poses a risk for the respiratory system.
Please see Introduction to Burns for more information regarding TBSA Assessment
3. Burn Type and Depth[edit | edit source]
It is important to regularly re-examine the extent of tissue destruction as it can change up to 48 hours post burn. It is uncommon for a burn to present uniformly with a singe depth throughout[2]. Quick administration of first aid can influence the type and depth to a large extent.[1] ( British Burn Association 2005)
Click here for more information on Jacksons’ Burn Wound Model.
4. Burn Site and Impact[edit | edit source]
The burn site can have a large impact of the potential functional outcome and the trauma associated with the injury. There are four High Impact areas associated with burns and this requires an awareness of the clinician assessing as these areas require specialised treatment.
High Impact Areas:
- Hands
- Face
- Perineum
- Joints
5. Current History[edit | edit source]
When conducting the current history questioning, please be aware of the emotional trauma that could be associated with a burn injury. If there is a family member or witness around, they can also be asked to fill in areas of the history that either the patient cannot recall, or that they are battling emotionally to elaborate on.
Important aspects to cover:
- History of the incident
- Specific attention paid to the mechanism of injury
- First aid
- An accurate account of what treatment was given?
- On site medication administered needs to be explained clearly with amounts and times given as this could react with the medication administered on admission to hospital
- If no adequate first aid was administered, suspect deeper burn injury
- Falls
- Is there any indication that the patient fell?
- What height did they fall from?
- Suspect a possible head injury, sprain or fracture
- Electrical injury
- What voltage was involved?
- Which parts of the body was in contact with earth?
- Suspect nerve or deep muscle injury with high voltage current
- Explosions
- Suspect a fall, high velocity injury or possible tympanic membrane injury, as the latter would cause a loss of hearing and difficulty communicating
- Passage to hospital and time to admission
ANZBA 2007; British Burn Association 2005; Eisenmann-Klein 2010
6. Medical and Surgical History[edit | edit source]
- Pain medication
- Debridement
- Escharectomy
- Flaps/grafts
- Any particular MDT instructions to be followed
ANZBA 2007; British Burn Association 2005; Hettiaratchy et al 2004
7. Past History[edit | edit source]
- Include any medical history
- Previous surgical interventions
- Medication
- Amount
- Duration on medication
- Condition controlled or uncontrolled
8. Social History[edit | edit source]
ANZBA 2007; British Burn Association 2005; Eisenmann-Klein 2010
- Basic activities of daily living. These vary from person to person, some examples:
- Dressing
- Bathing
- Eating
- Shopping
- Driving
- Home maintenance
- Past physical function
- General mobility
- Stair mobility
- Lifting
- Past physical fitness
- Strength
- Flexibility
- Endurance
- Balance
- Social support and home situation
- Occupation
- Particularly important for hand burns
Psychosocial Factors/ Yellow Flags[edit | edit source]
- Self-image
- Coping style
- Mental health
- Emotional behaviour
ANZBA 2007; British Burn Association 2005; Hettiaratchy et al 2004
Objective Assessment[edit | edit source]
Pain Intensity Assessment[edit | edit source]
Observational behavioural pain assessment scales should be used to Measure pain in children aged 0 to 4 years e.g.
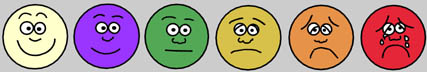
- Visual Analogue Scale (VAS) and the Wong-Baker FACES pain rating scale
- Visual analogue scale can have the faces used alongside but also has numbers assigned below the faces which the patient uses to indicate their pain scores.
- VAS can be used from age 12 upwards and is suitable for adults.
- Wong-Baker FACES consists of 6 pain assessment cards that vary from a smile to sad to crying facial expressions representing pain behavior rating and is supervised by the Chinese Association for the Study of Pain (CASP). The patient chooses the best card to represent the pain intensity.
- Faces pain rating scale can be used in children aged 5 years and older.
- The FLACC scale[3]
- 5 categories:
- Face
- Legs
- Activity
- Cry
- Consolability
- each of which accounts for scores of 0 to 2. With 10 as the full mark, 0 to 3, 4 to 7 and 8 to 10 scores represent no/light pain, moderate pain and acute pain, respectively
- 5 categories:
- COMFORT scale
- 6 categories including
- Alertness
- Calmness/agitation
- Crying
- Physical movement
- Muscle tone
- Facial tension
- With a full mark of 30, each category is scored on a 1 to 5 scale. In practice, suggestive information is offered according to the sum of the scores among the 6 categories. The higher scores one obtains, the more violent the pain (Table S1). Necessary pain interventional therapies shall be taken if the scores add up to more than 17
- 6 categories including
- Pain Observation Scale for Young Children (POCIS)
- used for pain behavioral assessment with points ranging from 0 to 7, in which 0, 1 to 2, 3 to 4 and 5 to 7 are recorded as no pain, slight pain, moderate pain and severe pain, respectively, with 7 categories each contributing 0 or 1 point towards the overall score
For more information regarding Pain Assessment Tools please see:
- British Pain Society Outcome Measures
- Physiopedia page on Outcome Measures
- Zieliński J, Morawska-Kochman M, Zatoński T. Pain assessment and management in children in the postoperative period: A review of the most commonly used postoperative pain assessment tools, new diagnostic methods and the latest guidelines for postoperative pain therapy in children. Adv Clin Exp Med. 2020 Mar 1;29(3):365-74.[4]
Burn Outcome Measures[edit | edit source]
When treating patients in a multidicsciplinary team, it is useful to use outcome measures that can be retested as the condition progresses. Some examples:
- Burn Specific Health Scale -Brief (BSHS-B): Examine the physical and psychosocial functioning of burn patients and their quality of life. McMahon 2008;Brusselaers et al 2010; Wasiak et al 2011
- Burns Scar Index (Vancouver Scar Scale)
- Burns Specific Pain Anxiety Scale
Taal LA, Faber AW, Van Loey NE, Reynders CL, Hofland HW. The abbreviated burn specific pain anxiety scale: a multicenter study. Burns. 1999 Sep 1;25(6):493-7. - file:///C:/Users/mamad/Downloads/taal1999BSPAS.pdf
https://www.sciencedirect.com/science/article/abs/pii/S0305417996001179
Taal LA, Faber AW. The burn specific pain anxiety scale: introduction of a reliable and valid measure. Burns. 1997 Mar 1;23(2):147-50.
Inhalation Assessment[edit | edit source]
Physical signs are not the most reliable and accurate tools for assessment but they can contribute to the whole assessment of the patient. Physical signs should be included with clinical tests, regular re-assessment and correct initial management.
Initial management:
- Quick transportation to the emergency room
- Conscious
- Patent airway
- Chest radiograph
- Arterial blood gases
Physical Signs[5] (ANZBA 2007; British Burn Association 2005)
- Soot stained sputum
- Stridor (Noisy breathing due to an obstructed airway)
- Wheezing
- Facial burns
- Singed nasal hairs
- Anxiety
- Cough
- Stupor
- Dyspnea
- Hoarse vocal quality
- Singed facial / nasal hair
- Oedema
- Erythema (Superficial reddening of the skin, usually in patches, as a result of injury or irritation causing dilatation of the blood capillaries)
- Inspiratory and end expiratory crackles on auscultation
- Chest x-ray changes
- Signs of Hypoxia
- Headache
- Shortness of breath
- Fast heartbeat
- Coughing
- Wheezing
- Confusion
- Bluish color in skin, fingernails, and lips
Bronchoscopy Assessment:[5]
- Bronchoscopy assists with rapid diagnosis of inhalation injury and grading it be unavailable to the clinician and is considered the gold standard[6]
- Inhalation Injury signs on bronchoscopy:
- Erythema
- Edema (which may be seen as a blunting of the carina)
- Mucosal blisters
- Erosions
- Hemorrhages
- Bronchial secretions
- Soot deposits
- Indirect laryngoscopy permits visual assessment to the level of the vocal cords and can be a useful, albeit limited, tool should
Three determinants of injury severity[5]
- Duration of smoke exposure
- Temperature of the inhaled smoke
- Composition of the smoke
For the latest recommendations please see:
- A Critical Update of the Assessment and Acute Management of Patients with Severe Burns[7]
- Inhalation Injury in the Burned Patient[5]
Oedema Assessment[edit | edit source]
WORDS CARIN!!!!!!
| Stage of Oedema | Appearance of Oedema |
| Stage 1 | Soft, may pit on pressure |
| Stage 2 | Firm, rubbery, non-pitting |
| Stage 3 | Hard, fibrosed |
Clinical stages and appearance of oedema
When assessing oedema, the subjective component includes when the swelling began and any changes in the oedema with position. The objective assessment needs to be carefully carried out so there is a reduced risk on infection and no increase in pain.
The most commonly used tools to measure edema are:
- Volume measurements (with a water volumeter)
- Girth measurements (with a tape measure).
- Pitting edema assessment (based on the depth and duration of the indentation).
For more information on how to conduct these measurements, please see Oedema Assessment
Physical Assessment[edit | edit source]
When conducting a physical assessment, it is often helpful to break up the assessment into two section. Firstly the upper limbs, lower limbs and trunk, secondly, general functional mobility. When conducting a physical assessment, it is important to consider complicating factors such as prolonged bed rest, high levels of pain and pre-existing co morbidities.
(ANZBA 2007; Hettiaratchy et al 2004; Settle 1986; Siemionow and Eisenmann Klein 2010)
- Limbs and Trunk
- Assessment of:
- Joint range of motion
- Muscle Strength
- Muscle Length
- Limiting factors:
- Pain
- Muscle length
- Trans-articular burns
- Scar contracture
- Individual specificity of the burn
- Assessment of:
- General Functional Mobility
- The mobility assessment should only be carried out once the patient is medically stable and the focus is:
- Prevention of complications associated with prolonged bed rest
- Restoration of function & independence.
- Factors to be assessed:
- Functional transfers
- Gait
- Endurance
- Balance
- Factors to consider:
- Posture
- Activities of daily living
- Demands of vocational roles
- Cardiovascular response to mobilisation
- Neurological status
- Pain
- Concomitant injuries/weight-bearing status
- The mobility assessment should only be carried out once the patient is medically stable and the focus is:
Management of Burn Pain[edit | edit source]
There are many factors to consider when when treating burn pain. Initially, The clinician should understand what pain is currently being treated and the cause of the pain.
Initially the acute pain experienced is due to the burning tissues. The burn should be cooled with tepid water, not ice ater as this can cause further damage to the area. This helps to end the burning and decrease the pain experienced. Cooling the burn and the evapotarion of oedema fluid can lead to hypothermia. Due to this, the patient should be given sufficient aid to warm themselves
Once hospitalised, there are a number of factors which should be considered by the clinicians. These being
- Pain associated with procedures. Usually of a high intensity but short duration
- Surgery
- Wound cleaning
- Dressing changes
- Physiotherapy
- Resting pain. Usually of low intensity but longer duration
- Pruritus
- Chronic pain. This can be due to changes experienced in nerve fibres.
Pain associated with procedures[edit | edit source]
Each procedure will trigger a fresh painful stimulus and further stress response. Therefore, analgesia should be preventive, as some of these events are predictable. Pain, and thus poor analgesia, may interfere with sleep, which is felt to be a significant part of the healing process. During the early part of the in-patient stay, prolonged procedures may be best performed under general anaesthesia. This is especially true if access to the patient will be difficult or in the case of children where fear of repeated potentially painful procedures will be a significant barrier to trusting the staff.
Surgery[edit | edit source]
Intraoperative and postoperative analgesia will usually be based on opioids. The concept of balanced analgesia will encourage the additional use of regional block and NSAIDs, depending on the extent of injury and site of graft harvest. However, as with other critically ill patients and if large volumes of fluid or blood are required, coagulopathy may occur. This may preclude the use of neuraxial techniques. Likewise, a risk of haematoma formation underneath a critical skin graft may preclude the use of nonspecific COX inhibitors. Large raw areas produced during surgery, in particular donor sites, are amenable to analgesia by a number of methods. At surgery, local anaesthetic gel may be applied under the dressings. Bupivacaine is effective (0.5% plain mixed with an equal quantity of aqueous gel), although there is a theoretical risk of local anaesthetic toxicity following unpredictable absorption over a large area (studies have not demonstrated this to date). An appropriate regional block may be used. However, regional techniques are less often used than might be expected because of practical difficulties such as infection at or close to the insertion site, generalized sepsis and coagulation abnormalities. For the lower limbs and abdomen, a continuous epidural infusion may be possible. Opioids may be added to the regimen, giving a reduced risk of local anaesthetic toxicity and therefore side-effects. Brachial or lumbar plexus block is also an effective technique. Appropriate selection of local anaesthetic agents allows the block to persist into the postoperative period; this may be prolonged further by the addition of a2-antagonistssuch as clonidine. Single-shotregimens are less effective; however, interestis growing in the placement of catheters alongside the nerve plexus to allow repeated bolus doses or infusions. The placement of epidural or limb catheters has a potential for bacterial colonization, and they may fall out if attached to mobile areas of skin or close to the burn where fixation is difficult. Once again, the mainstay of early postoperative pain management is based on opioids. These can be administered transdermally, orally, intramuscularly and intravenously with a combination of background infusion and boluses. All have their merits, but intramuscular administration may be difficult due to the site of surgery, the extent of dressings, injection site discomfort and unpredictable absorption. There is a vogue for patient-controlled analgesia (PCA), which has been found to be effective in burnsin severalstudies. However, thisis not ideal, asit requires a cooperative patient able to use the device (not possible with burned hands) and plasma opioid concentrations may fall during sleep. A background infusion will reduce the likelihood of this; however, opioids have a tendency to accumulate, leading to undesirable side-effects. Nursing vigilance must be maintained and protocols must be in place to prevent or deal with these events. Similar constraints apply to the use of opioids by continuous infusion, which is an effective approach immediately after operation if carefully monitored. The inflammatory component of pain and opioid use can be reduced by regular NSAID analgesia, unless the risk of haematoma formation outweighs the benefits.
Dressings changes[edit | edit source]
The management of pain during dressings changes is the most extensively investigated aspect of burn pain management, yet no single technique has been shown to be better than any other. A large burn dressing may take 1--2 h and may include active wound debridement or postoperative removal of items such as staples. General anaesthesia is often appropriate; deep intravenous sedation may be given and supervised by an anaesthetist. For smaller dressings, analgesia is commenced before the procedure takes place by a bolus of opioid or local anaesthetic; time is Pain in the patient with burns Continuing Education in Anaesthesia, Critical Care & Pain | Volume 4 Number 2 2004 59 Downloaded from https://academic.oup.com/bjaed/article/4/2/57/271658 by guest on 14 June 2022 allowed for onset of the analgesia. Depending on the level of stimulus, further doses can be used during the procedure supplemented by a benzodiazepine. Entonox is useful for short procedures to supplement opioids, reduce breakthrough pain and avoid prolonged sedation. Ideally, easily titratable sedative and analgesic agents with few side-effects and short half-lives are required. Few drugs have all these properties. Sedation with many agents has been reported, including lidocaine infusions, benzodiazepines and volatile inhalation agents. Ketamine is analgesic and sedative. Although loss of airway is unlikely at normal doses, its use islimited in adults by side-effects including hallucinations. The latter can be mitigated by adding a small dose of a benzodiazepine. Boluses orinfusions ofshorter-acting opioidssuch as alfentanil and fentanyl are suitable for short procedures. They can nevertheless accumulate and may result in respiratory depression, particularly if given to a patient already receiving opioids. Combination with a low-dose infusion of propofol (administered by an anaesthetist) gives adequate conditions for dressings changes. The effects of propofol terminate within minutes if a target-controlled infusion at a dose range of 1--2 mg mlÿ1 is used. Further flexibility can be introduced by adding remifentanil. Because the half-life of remifentanil is short, supplementation with opioids, NSAIDs, or both, is necessary to control pain in the post-procedural period. The requirement for procedures can be reduced by using suitable dressings, such as a synthetic temporary skin substitute, especially in children. Biobrane1 (a porcine collagen-based material) and similar synthetics are used on superficial wounds that are expected to heal; they are left in place until healthy skin has formed, thus reducing distress and infection risk and also allowing early mobilization.
Physiotherapy[edit | edit source]
Physiotherapy is an important part of rehabilitation. Moving damaged areas causes pain and further exacerbation of the stress response. On the other hand, the patient is engaged in the process and therefore motivated. This type of pain is predictable and again amenable to multimodal management using oral analgesics. The scope of strong painkillers and anaesthesia is limited because of the requirement for cooperation; however, the physiotherapists will often take the opportunity of a visit to theatre or the dressings station to perform passive range of movement exercises in the early stages.
Resting Pain[edit | edit source]
After initial treatment and between procedures, the patient most commonly suffers low-grade but persistent discomfort, the nature of which has been repeatedly shown to be under-appreciated even by experienced staff. This is difficult to treat adequately while minimizing the patient’s exposure to side-effects, but adequate treatment is essential to patient well-being. A multimodal approach using low-dose oral opioids in combination with NSAIDs provides best results. Careful titration by measuring the extent of pain relief regularly and adjusting doses accordingly is essential; it can be integrated into the work of the Acute Pain Team or managed by the burns nurses according to well-designed protocols. Pre-emptive, regular dosing with supplemental prescriptions for breakthrough pain is most effective in practice.
Itching[edit | edit source]
Pruritus is another disabling condition that is poorly understood. It may disrupt normal physiology, and scratching may cause damage to forming skin. The mechanism is thought to involve histamine and prostaglandin release. Treatment is again difficult and usually involves combinations of antihistamines and NSAIDs. Empirical observation that heat may trigger the reaction has led to treatment by cold compresses and control of the environmental temperature.
Chronic Pain[edit | edit source]
Damaged and regenerating nerve tissues can give rise to complex neuropathic pain syndromes whereby the sensation of the painful stimulus far outlives its expected duration. This can destroy the sleep pattern, result in depressive symptoms and impair rehabilitation. There may be hyperalgesia (an increased response to a painful stimulus) and allodynia (a painful response to a normally innocuous stimulus). This may be a significant problem starting quite early in the post-injury course and persisting for many years afterthe initial injury (Table 1). Thistype of pain is very difficult to treat using conventional analgesics, unlessthere is ongoing inflammation or tissue damage. The severity of chronic symptoms is often related to the size of the burn and the number of skin grafts performed. Treatment includes antidepressants (amitriptyline), anticonvulsants (gabapentin and sodium valproate), regional nerve block and cognitive behavioural therapy.
Norman AT, Judkins KC. Pain in the patient with burns. Continuing education in anaesthesia, critical care & pain. 2004 Apr 1;4(2):57-61.
Judkins KC. Pain management in the burned patient. Pain Rev 1998; 5: 133--46
Kidd BL, Urban LA. Mechanisms of inflammatory pain. Br J Anaesth 2001; 87: 3--11
MalenfantA, ForgetR, Papillon J,AmselR, Frigon J, ChoiniereM. Prevalence and characteristics of chronic sensory problemsin burn patients. Pain 1996; 67: 493--500
Pal KS, Cortiella J, Herndon D. Adjunctive methods of pain control in burns. Burns 1997; 23: 404--12
Thurber CA, Martin-Herz SP, Patterson DR. Psychological principles of burn wound pain in children. 1: Theoretical framework. J Burn Care Rehab 2000; 21: 376--86
- Pharmacological Pain Management
- Opioids
- Simple analgesics
- NSAIDS
- Alternative Techniques
- Psychological techniques
- Hypnosis
- Virtual Reality
- Sleep Normalisation
- Music therapy
- Paediatric Burn Pain
- Other causes of pain
1. Pharmacological Pain Management: (Richardson and Mustard 2009)[edit | edit source]
Pharmacological pain management usually begins within the first 48 hours after a burn injury. There is no standard treatment of burns patients, each requires individual assessment. The most common
Opioids:[edit | edit source]
the cornerstone of pain management in burns, and are available in a variety of potencies, methods of administration and duration of action. Opioids used to effectively manage background pain, with well-timed and effective doses of opioids used separately to manage procedural pain
For a patient with a large burn needing immediate, vigorous cleaning, the only viable recourse may be general anaesthesia. This will be especially true if there is an inhalation injury or multiple trauma requiring stabilization, surgery or transfer to an appropriate specialist centre. Continuous intravenous infusions of opioids provide the mainstay of analgesia for this group. For the patient without threat to the airway, the gold standard remains intravenous morphine. This can be titrated in small (1--2 mg) boluses until the patient is comfortable. Due diligence must be exercised to avoid the side-effects of excessive sedation and respiratory depression; nevertheless, high doses are sometimes required. Absorption of opioids given intramuscularly may be unpredictable. Tissue damage releases multiple inflammatory mediators such as hydrogen ions, prostaglandins and bradykinin.
| Positive Effects | Side Effects | Examples of Opioids |
| Pain relief
Increased comfort Morphine related to reduced Post-traumatic stress disorder |
Respiratory distress
Itch Nausea and vomiting Opioid tolerance – requiring increasing doses Opioid induced hyperalgesia (OIH) – increased sensitivity, throughout the body following opioid exposure Provide poor defence against central sensitisation Physical dependence – common in long term use 25 |
Morphine
Oxycodone Fentanyl: potent, rapid onset, short acting opioid. Used for procedural pain management. Remifentaril: ultra-short acting opiate. Alfentaril: short acting, used for post-procedural analgesia. Table 5: side effects of opioidsMethadone: long acting |
Simple analgesics:[edit | edit source]
paracetamol can be used in conjunction with opioids, to give a synergistic effect comparable to a higher opioid dose. Paracetamol is an effective anti-pyretic and has few contra-indications.
Non-steroidal anti-inflammatory drugs (NSAIDs) inhibit the formation of prostaglandins and therefore provide analgesia. They may be useful alone in smaller burns or as an adjunct to opioids. However, the severely burnt patient may be hypovolaemic and therefore at risk of gastric erosions. NSAIDs should be used with caution in the Pain in the patient with burns 58 Continuing Education in Anaesthesia, Critical Care & Pain | Volume 4 Number 2 2004 Downloaded from https://academic.oup.com/bjaed/article/4/2/57/271658 by guest on 14 June 2022 shocked patient or the elderly. If NSAIDs are contraindicated, then tramadol may be useful as an intermediately potent analgesic. If there is concern over the patient’s condition, keep it simple (i.e. intravenous morphine with adequate fluid resuscitation).
Non-steroidal Anti-inflammatory Drugs (NSAIDS):[edit | edit source]
synergistic with opioids and can reduce opioid dose and thus reduce side-effects. Not used in wide spread burns due to already increased risk of renal failure and peptic ulceration. There is potential to increase bleeding in large burns also, due to the anti-platelet effect.
Other medications:[edit | edit source]
see Richardson and Mustard 2009
Possible side effects of analgesics:
- Drowsiness
- Adverse reaction
- Nausea and increased risk of aspiration
- Impaired memory and communication
- Postural hypotension, and fainting (ANZBA 2007) 3.2 Non-Pharmacological Management of Pain
The following is a synthesis of information form the following articles: Summer et al (2007), Richardson and Mustard (2009), ANZBA (2007) and de Jong et al (2007)
Overall, the levels of evidence to support the use of alternative therapies for pain relief are of poor quality. However, no negative side effects were reported in the literature reviews and these therapies are all used in conjunction with pharmacological management to optimize pain relief for the individual.
2. Alternative Techniques:[edit | edit source]
Psychological techniques:[edit | edit source]
beneficial for reducing anxiety and providing patients with coping methods for pain levels and durations. These include relaxation, distraction and cognitive behavioural therapy (CBT). CBT is beneficial in the management of complex pain problems and can reduce fear and anxiety associated with activities or environments.
Hypnosis:[edit | edit source]
a state of “increased suggestibility, attention and relaxation”. In the burn patient hypnosis is used in the management of procedural pain and anxiety. The use of hypnosis clinically is increasing but its usefulness is dependent on the individual’s hypnotic susceptibility, high baseline pain and the skill of the practitioner. The current best available evidence for management of procedural pain was found for active hypnosis, rapid induction analgesia and distraction relaxation.
Virtual Reality:[edit | edit source]
immersing the patient in a virtual world has shown some effect on procedural pain control and is better than hand-held gaming devices. However, the equipment is costly and bulky and not always suitable for paediatric intervention. A paediatric intervention, using hand-held game devices which provide augmented reality was trialled among 3-14 year olds. This has shown significantly lower pain scores than standard distraction and relaxation when undergoing dressing changes (Mott et al 2008).
Sleep Normalisation:[edit | edit source]
disrupted sleep occurs in up to 50% of burn patients and links have been established between poor sleep quality and pain severity, as well as pain and prolonged experiences of sleep disturbance. Normalisation of the 24hour day, with a bedtime routine, within the limits of the hospital environment is aimed for to promote sleep, with the use of analgesics and night sedation.
Music therapy:[edit | edit source]
this is thought to target pain via the gate control theory. This suggests that music serves as a distraction from noxious stimuli. Also, the anxiety related to the rehabilitation of burns can increase the activation of the sympathetic nervous system. Music uses all three cognitive strategies employed in pain and anxiety management (imagery –
envisioning events that are inconsistent with pain, self-statements and attention-diversion devices to direct attention away from the pain ad redirects it to another event) (Ferusson and Voll 2004; Presner et al 2001).
A systematic review of music therapy among pregnant women, medical-surgical patients and critical care patients showed statistically significant reductions in pain scores. Of the seventeen studies reviewed by Cole and LoBiondo-Wood (2012), 13 studies demonstrated the positive effects of music on pain. Other positive findings of the studies included reduced anxiety, muscle tension, blood pressure and heart rate. A burn specific study included showed reduced pain levels during and after the debridement, reduced anxiety and decreased muscle tension during and after dressing changes.
The Cochrane Review of music as an adjunct to pain relief concluded that “music and other non-pharmacological therapies could have a synergistic effect to produce clinically important benefits on pain intensity or analgesic requirements” and thus requires further study. This is based on the studies indicating that music resulted in reduced pain intensity and reduced opioid requirements. The reported changes in both of these outcomes were small however, and their clinical importance is unclear (Cepeda et al 2006).
3.Paediatric Burn Pain (Richardson and Mustard 2009)[edit | edit source]
∙ children 0-4 years represent approx. 20% all hospitalised burn patients ∙ In preschool aged children the half-life of opioids (morphine and alfentanyl) are 50% those in adults. Higher dosage required.
∙ Risk of accidental overdose due to difficulties with pain evaluation resulting in overestimation of child’s pain
∙ Childs environment has huge effect on pain perception. Parents’ presence and aid during dressing change can have beneficial for procedural pain and reducing anxiety.
The whole experience of trauma, hospital admission and treatment cycles is especially distressing for children. They require the same standard of analgesia and treatment as adults but are more difficult to assess in terms of pain. Behavioural assessments are important, especially in babies and toddlers where, for instance, quiet inactivity should be considered abnormal; administration of analgesia may restore play. Instead of a Visual Analogue Score, several scales are available, the best known of which is the Children’s Hospital of Eastern Ontario Pain Scale (CHEOPS) which uses ‘smiley faces’. It has been shown that PCA can be used successfully in children as young as 4 yrs old. Psychological strategies have also been shown to work in children. The role of the Hospital Play Specialist is crucial in this respect; every burn unit should have at least one. The role of appropriate dressings material in children (e.g. Biobrane1) has been emphasized previously. Propofol is not licensed for younger children, so other intravenous techniques must be used for dressings changes. For a first procedure, general anaesthesia is a kindness that minimizes later aversion to procedures. Ketamine is still widely used for children, in whom side-effects seem to be less of a problem. Addition of a small dose of benzodiazepine reduces the incidence of hallucinations.
3.3 Considerations Pre Physiotherapy Treatment[edit | edit source]
∙ Pain relief is key. Timing physiotherapy to correspond with analgesia is essential for the patient, particularly to avoid the pain-anxiety avoided.
∙ Knowledge of pain medications, short-acting pain relief may be required in addition to long-acting background pain relief prior to physiotherapy. Also, the side-effects possible due to the medications, and vigilance for signs of these.
∙ Daily assessment of therapy input and pain management to ensure on-going management of pain. (ANZBA 2007)
28
4. Other causes of pain[edit | edit source]
The burn wound and donor sites are not the only possible causes of pain in the burned patient, especially in major or multiple injuries. In the initial assessment, a secondary survey must performed to locate other injuries. Pain from fractures may be severe. Current guidelines recommend the stabilization of the fracture and the titration-to-effect of intravenous opioid. Likewise, the pain of abdominal injuries should be managed appropriately. Compartment syndrome in a limb may be a concern with a circumferential burn or in association with a fracture and can be caused or exacerbated by fluid resuscitation. If untreated this will result in limb ischaemia. Surgical decompression is required. Pain should be also considered as a harbinger of infection in the recovery phase. Hot, erythematous, swollen areas may indicate cellulitis or pusformation, which necessitates systemic antibiotics, surgical incision and drainage, or both. Major burns are associated with a multitude of complications including perforation of an abdominal viscus, colonic pseudo-obstruction, abdominal compartment syndrome and heterotopic bone deposition; in all of these scenarios, a change in the magnitude or type of pain may be the first indicator of trouble.
Oedema Management[edit | edit source]
1. Elevation[edit | edit source]
Elevation of the hand above heart level is the most simple and effective ways to prevent and decrease oedema (Kamolz 2009). A Bradford sling can be used to facilitate elevation. This type of sling facilitates both elevation and protection of wound area while still allowing movement. Its foam design also reduces the risk of the development of pressure points or friction (Glassey 2004).
Fig 21. Bradford sling in a position
of elevation (Microsurgeon 2013)
When a patient is admitted with severe burns of a large TBSA they are at risk of systemic inflammation. Therefore, not only must the affected limb be placed in elevation, the following precautions should also be taken
∙ Elevation of the head: This aids chest clearance, reduces swelling of head, neck and upper airways. It is important not place a pillow underneath the head in the case of anterior neck burns as there is a risk of neck flexion contractures
∙ Elevate all limbs effected
∙ Feet should be kept at 90
∙ Neutral position of hips
∙ Care must be taken to reduce the risk of pressure sores. (Procter 2010)
2. Compression[edit | edit source]
2.1 Coban Wrap[edit | edit source]
A Coban Wrap is a self-adhesive bandage. the advantage of this is that it will not stick to the underlying tissue and interrupt the healing process. This makes it suitable for decreasing hand oedema, particularly in the acute stages of a burn. There is evidence that the Coban Wrap assists in decreasing oedema, improving dexterity, range of motion and grip strength in hands.
Lowell 2003
Burns and Plastic Surgery Occupational Therapy
2.2 Oedema Glove/Digi Sleeve[edit | edit source]
These are hand specific oedema management products. There is currently no specific evidence available to support the efficacy of oedema gloves or digi sleeves in the reduction of oedema. However it is common practice in Irish hospital to provide these products to patients with excessive hand and finger oedema. Their use is based on the principle of compression to reduce oedema which is heavily supported by evidence (Latham and Radomski 2008).
Scar Management[edit | edit source]
Abnormal scarring is the most common complication of burn injuries, with the estimated prevalence of > 70% of those who suffer burn injuries (Anzarut et al, 2009). Not only do hypertrophic scars cause psychosocial difficulties through their cosmetic appearance, they may also be painful, pruritic, and they may limit range of motion where they occur on or near a joint (Morien et al 2009; Polotto 2011).
Hypertrophic scars require a continuum of dedicated and specialised treatment from the acute stage to many years post treatment (Procter, 2010, ANZBA 2007).
The following is an examination of the evidence and recommendations for use in the most common of these, including silicone gel, pressure garment therapy, and massage. The positioning and mobilisation advice above is all applicable, and should be continued in the management of hypertrophic scars where necessary.
5.221 Scar Outcome Measures[edit | edit source]
- Vancouver Burn Scar Scale (VBSS/VSS)
- Aim: Assessment of the scar in 4 catagories: Vascularity, height/thickness, pliability, and pigmentation, relief, and surface area. Also includes assessment of patient pain, itching, colour, stiffness, thickness and relief. The only scale to measure subjective aspects of pain and pruritus (severe itching) (Fearmonti et al 2010).(Fearmonti et al 2010)(Durani et al 2009)(Brusselaers et al 2010)
- Method: Burns Scar Index (Vancouver Scar Scale)
- Patient and Observer Scar Assessment Scale (POSAS)
- Aim: Assessment of the scar from the patient and the observers perspective
- Method: About POSAS
- Burn Specific Health Scale -Brief (BSHS-B)
- Aim: Assessment of general, physical, mental, and social health aspects of the burn survivor
- Method: Burn Specific Health Scale -Brief (BSHS-B)
5.222 Silicone[edit | edit source]
Silicone Overview
The use of silicone gel or sheeting to prevent and treat hypertrophic scarring is still relatively new. It began in 1981 with treatment of burn scars (O’Brien & Pandit 2008). The physiological effects of silicone in the treatment of scarring remain unclear. Below is a summary of the current hypotheses surrounding the physiological effects of silicone. This summary has been adapted from the most recently published literature on this topic.
1) Hydration Effect: Hydration can be caused by the occlusion of the underlying skin. It decreases capillary activity and collagen production, through inhibition of the proliferation of fibroblasts
2) Increase in temperature: A rise in temperature increases collagenase activity thus increased scar breakdown.
51
3) Polarized Electric Fields: The negative charge within silicone causes polarization of the scar tissue, resulting in involution of the scar.
4) Presence of silicone oil: The presence of silicone has been detected in the stratum corneum of skin exposed to silicone. However other researchers suggest occlusive products without silicone show similar results.
5) Oxygen tension: After silicone treatment the hydrated stratum corneum is more permeable to oxygen and thus oxygen tension in the epidermis and upper dermis rises. Increased oxygen tension will inhibit the ‘‘hypoxia signal’’ from this tissue. Hypoxia is a stimulus to angiogenesis and tissue growth in wound healing, as a consequence removing the hypoxia stops new tissue growth. This theory has been contraindicated by other researchers.
6) Mast cells: It is suggested that silicone results in an increase of mast cells in the cellular matrix of the scar with subsequent accelerated remodelling of the tissue. 7) Static electricity: Static electricity on silicone may influence the alignment of collagen deposition (negative static electric field generated by friction between silicone gel/sheets and the skin could cause collagen realignment and result in the involution of scars. (Bloemen et al 2009; Momeni et al 2009)
Evidence
Momeni et al 2009: RCT, double blind placebo controlled trial
Subjects: N=38, with hypertrophic scars post thermal burn. All were 2-4 months post burn, with areas including upper limb (n=14) lower limb (n=8) trunk (n=3) and face (n=9).
Intervention: Patients acted as their own control, with the scar area being randomly divided into two sections: one received silicone sheets, and the other a placebo. Both were applied for 4hrs/day initially, with this incrementally increased to 24 hrs/day over the course of the study, for a four month period.
Outcome measures: assessed at one and four months, by a blinded assessor using the Vancouver Scar Scale and by Clinical Appearance.
Results: No significant differences in baseline characteristics. At one month the silicone group had lower scar scores than the placebo group, however they were not statistically
52
significant. At four months, the silicone group had significantly lower scores on VSS for all dimensions except pain compared to placebo.
Limitations: Small heterogeneous cohort. No discussion of clinical significance of the reduction in scar scales. 4 subjects lost to follow up with no intention to treat analysis.
Brien and Pandit 2008: Cochrane Systematic Review Investigating the Efficacy of Silicone Gel Sheeting in Preventing and Treating Hypertrophic and Keloid Scars
Studies Included: 15 RCTs, n=615, only 3 studies specific to burn patients. 12 compared silicone to no treatment, and the remainder silicone was compared to placebo or laser treatment.
Outcome Measures: Primary outcome measures included scar length, width and thickness; secondary outcomes include scar appearance, colour, elasticity, relief of itching/pain
Results: No significant difference between silicone gel sheeting and control in reducing scar length and width. Significant results for reducing scar thickness, though these were thought not to be clinically relevant. No statistically significant difference between silicone gel and controls in secondary outcomes.
Limitations: Large age range, heterogeneous sample, poor quality of trials in general, with most at high risk of selection and detection bias. Only three studies used blinded outcome measures. 6 studies lost >10% of participants to follow up.
Conclusion on Silicone
It is unclear whether silicone gel help prevent scarring. Many of the studies advocating the use of silicone gel are of poor quality and are susceptible to bias. However, it is currently common practice in Ireland to administered silicone gel as an adjunct to treatment of scarring. Silicone gel as opposed to sheets is the preferred product to use as it is easier to apply can be used on more areas of the body and gives a higher patient compliance (Bloemen et al 2009).
53
5.223 Pressure Garment Therapy (PGT)[edit | edit source]
Though the effectiveness of PGT has never been proven, it is a common treatment modality for reducing oedema and managing hypertrophic scars (Procter, 2010).
Aims
o Reduce scarring by hastening maturation
o Pressure decreases blood flow
o Local hypoxia of hypervascular scars
o Reduction in collagen deposition
o Therefore
o Decreases scar thickness
o Decreases scar redness
o Decreases swelling
o Reduces itch
o Protects new skin/grafts
o Maintains contours (Procter 2010)
The exact physiological effects of how pressure positively influences the maturation of hypertrophic scars remain unclear. Below is a summary of the current hypotheses surrounding the physiological effects of pressure garments. This summary has been adapted from the most recently published literature on
1) Hydration effect: decreased scar hydration results in mast cell stabilization and a subsequent decrease in neurovascularisation and extracellular matrix production. However this hypothesis is in contrast with a mechanism of action of silicone, in which an increase of mast cells causes scar maturation.
2) Blood flow: a decrease in blood flow causes excessive hypoxia resulting in fibroblast degeneration and decreased levels of chondroitin-4-sulfate, with a subsequent increase in collagen degradation.
3) Prostaglandin E2 release: Induction of prostaglandin E2 release, which can block fibroblast proliferation as well as collagen production
(MacIntyre & Baird 2006)
54
Evidence
The evidence for PGT is limited.
∙ Early studies found significant benefit from their use in terms of scar maturation and necessity of surgery for correction
∙ These were not RCTs, and were conducted in a time where inefficient surgical debridement resulted in scar loads much worse than those seen today (Engrav et al 2010)
| Article citation and design | Anzarut et al (2009)
Systematic Review+ Meta-Analysis |
Engrav et al (2010)
Within wound RCT |
| Selection criteria | 6 trials with 316 patients located 3 between-subject design
3 studies within-subject design Adult and paediatric populations |
54 patients recruited over 12 years
Forearm burn requiring >3 weeks to heal/skin grafting. Mean age, 36 yrs, mean length of follow up, 9.5 months |
| Intervention | 3 studies wore pressure garments for 23h/day
3 studies did not describe length of pressure garment treatment |
Randomised normal compression (17- 25mmHg) and low
compression (<5 mmHg) to proximal/distal area of scar. 23 hrs/ day to wound maturity, or up to 1 yr |
| Outcome measures | Primary Outcome:
Global scar score Secondary outcome: Scar height, vascularity, pliability, colour |
Durometry (hardness)
colorimetry (colour) ultrasonography (thickness) Clinical appearance: judged by a panel of 11 experts in burn care |
| Results | Global Scar Score:
∙ No significant differences between PGT & control interventions Secondary Outcome: |
∙ Statistically significant decrease in scar hardness
and height ∙ 3/19 and 5/28 patients respectively achieved a decrease which could be |
55
| ∙ Scar height showed a small but statistically significant decrease in height for pressure garment
therapy. ∙ Questionable if this is clinically significant. ∙ Scar vascularity, pliability and colour failed to demonstrate a different between groups |
clinically detected
∙ In only 3/41 patients could the zone of normal and low compression be identified correctly by a panel of 11 experts However, the authors concluded by recommending that PGT should continue to be used. | |
| Limitations | Publication bias present with only 1 trial reported negative effect
In 5 of the 6 studies, concealment of allocation was unclear All studies had inadequate reporting of randomisation and did not comment on withdrawals and dropouts. |
Some data lost for different parameters over the space of 12 years. Noted that in this time, staff and equipment changed, which could have confounded results. Evidence of bias in interpretation of results. Low risk of bias from randomisation, not all assesors blinded. |
Table 9 Available Evidence for PGT
∙ The authors’ bias was evident in both of the above articles. Though their results were similar, Anzarut et al, 2009 concluded that there was no evidence to justify this ‘expensive source of patient discomfort’, while Engrav et al, 2010 concluded that its use was justified.
Patient Adherence to Pressure Garment Therapy
In 2009 Ripper et al carried out a quantitative study on adult burn patient’s adherence to pressure garment therapy.
Subjects: 21 participates interviewed concerning their experiences with pressure garments. Time since burn ranged from 5months to 4years and 2 months.
Methodology: Randomised selection of patients 21 patients segregated into 3 groups: Patients who had completed PGT, Patients who were still in the course of therapy, and Patients who refused to wear the garments and had stopped PTG completely.
56
Results: Complaints most frequently mentioned were: “Physical and Functional limitations” caused by garments. “Additional effort” created by the need to care for the garment. Motivating factors for the patients: ‘expectation of success’ ‘emotional support’ ‘practical support’ and experiencing ‘good outcome’.
Limitation: Unclear method of randomised selection, variation in time elapsed since burns, body parts affected by burns not established
Careful considerations of cost, compliance, patient discomfort, possible complications and the perceived benefits before prescribing this treatment.
Recommendations for practice and safety considerations
Pressure: 15 mmHg has been noted as the minimum to elicit change, and pressures of above 40 mmHg have been found to cause complications. Both Anzarut et al (2009) and Engrav et al (2010) used pressures of between 15 and 25 mmHg.
Time: It is recommended that garments are worn for up to 23 hours a day, with removal for cleaning of the wound and garment, and moisturisation of the wound. (Procter 2010; Anzarut et al 2009 and Bloeman et al 2009).
Duration: garments can be worn as soon as wound closure has been obtained, and the scar is stable enough to tolerate pressure. Post grafting, 10-14 days wait is recommended, at the discretion of the surgeon (Bloeman et al 2009). Garments should be worn for up to one year, or until scar maturation (Anzarut et al 2009; Engrav et al 2010 and Bloeman et al 2009).
Possible complications/ confounding factors for use of PGT
∙ Lack of a scientific evidence to established optimum pressure
∙ Non-Compliance ( due to comfort, movement, appearance)
∙ Heat and perspiration
∙ Swelling of extremities caused by inhibited venous return
∙ Skin breakdown
∙ Web space discomfort
∙ Inconvenience
∙ Personal hygiene difficulties possibility of infection
∙ Allergies to material (MacIntyre & Baird 2006; Glassey 2004)
57
5.224 Massage
Five principles of scar massage:
1. Prevent adherence
2. Reduce redness
3. Reduce elevation of scar tissue
4. Relieve pruritus
5. Moisturise (Glassey 2004) Scar Massage Techniques
∙ Retrograde massage to aid venous return, increase lymphatic drainage, mobilise fluid ∙ Effleurage to increase circulation
∙ Static pressure to reduce pockets of swelling
∙ Finger and thumb kneading to mobilise the scar and surrounding tissue ∙ Skin rolling to restore mobility to tissue interfaces
∙ Wringing the scar to stretch and promote collagenous remodelling
∙ Frictions to loosen adhesions
(Holey and Cook 2003)
| Guidelines for Massage during 3 Stages of healing | |
| Inflammatory Phase | gentle massage to decrease oedema and increase blood supply (currently no high level evidence to support this) |
| Proliferative Phase | Massage that applies gentle stress to the healing scar is recommended to ensure collagen is aligned correctly. |
| Remodelling Phase | Massage should be progressed to include prolonged stretching to minimise adhesions. This is proposed to aid in scar tissue breakdown |
Table 10 Guidelines for scar massage during healing stages (Glassey 2004)
58
Table 11. Evidence for the use of massage in scar management
| Article | Field et al 2000
RCT |
Morien et al 2008
Pilot Study |
Shin and Bordeaux, 2012 Lit review |
| Subjects | 20 subjects in remodelling phase of wound healing. Randomly assigned into 2 groups
Massage Vs Control |
8 Children
Mean age 13.5 years (10-17years) All thermal burns including hand burns |
Not burn specific, though the majority of scars were of this origin
10 articles: n=144 adult and children |
| Intervention | Massage Therapy Group:
30minutes massage with cocoa butter twice weekly for 5 weeks Control Group: Standard Treatment |
20-25 minute massage session once daily for 5 days
(effleurage, petrissage, friction, lengthening rolling) Session followed by discussion of psychosocial issues |
Time to Rx: mean 4.3 months. + variation in protocols. 20 mins/day- 30 mins 2x weekly. 1 Rx-6 months Rx |
| Outcome
measures |
Itching: VAS
Pain: McGill Pain Questionnaire Anxiety: State Trait Anxiety Inventory Mood: Profile of Mood States |
Likert pictorial scale
Goniometry Range of Motion |
Patient and observer scar assessment scale, Vancouver scar scale, thickness, vascularity, colour, pain, pruritus, mood, anxiety, and depression. |
| Results | Massage Therapy Group Reported: decreased itching, pain, anxiety and increased mood
Ratings improved from the 1st-last day of the study |
Increased ROM in massaged tissue. Decreased ROM in unmassaged tissue
No significant difference in mood across time |
45.7% improved in at least one of the above parameters. 54.7% had no improvement.
Noted massage was more economical than silicone/PGT. |
59
| Limitations | Small Sample Size
No follow up |
Paediatric
population. Mood Instrument may have been influenced by other factors. Recruitment and area to be massaged not random Small sample size No follow up |
No discussion of quality or statistical tests. |
Conclusion on Scar Massage
Evidence suggests that burn patients receive psychological benefits from massage in terms of altered mood (decreased depression, anger), decreased pain, and anxiety (Field et al 1998). Evidence also indicates that massage increases ROM in non-burned patients, but little evidence exist examining the effect of massage on ROM in burn patients (Morien et al 2008).
Recommendations for practice and safety considerations.
Insufficient consistency in literature with regards to protocols on frequency or duration of treatment. Suggestions for practice include (Shin and Bordeaux, 2012, Morien et al, 2008)
∙ Clean hands essential
∙ Use non irritating lubricant, free of any known sensitisers.
∙ Modify practice according to patient stage of healing, sensitivity and pain levels. Contraindications: Shin and Bordeaux 2012
∙ Compromised integrity of epidermis
∙ Acute infection
∙ Bleeding
∙ Wound dehiscence,
∙ Graft failure
∙ Intolerable discomfort
∙ Hypersensitivity to emollient
Reconstruction Post Burn Injury[edit | edit source]
The impact of reconstructive surgery post burn injury has a major impact on a patient. As an allied health professional, we must work as part of an MDT in order to ensure successful surgery while at the same time ensuring long term health and function. Timely burn wound excision and skin grafting form the cornerstone for acute burn surgical management (Klein 2010).Surgery for burned patients is not normally indicated until 48 hours after injury, when the depth of the burn has been established. The only exception is when necrotic tissue is evident then early excision may be required. A plastic surgeon must reconstruct the injured body part in a way that is extensible, sensate and cosmetically acceptable (Glassey 2004). In addition to this, they must rebuild or replace muscles, tendons, joints and nerves to ensure they are appropriately intact.
4.1 Aims
1. Achieve would closure
2. Prevent infection
3. Re-establish the function and properties of an intact skin
4. Reduce the effect of burn scars causing joint contractures
5. Reduce the extent of a cosmetically unacceptable scar
(Glassey 2004; BBA Standard 6 2005)
4.2 Choosing the Correct Method of Reconstruction
The simplest management involves conservative wound care and dressings, while the most complex is free-flap reconstruction. When deciding on the most appropriate intervention, a surgeon must consider the extent of the missing tissue and the structures effected (Glassey 2004). Generally, a superficial partial thickness burn will heal with conservative treatment (secondary intention) in 10 days to 3 weeks, unless infection occurs. Primary intention occurs if a wound is of such size that it can be closed directly without producing undue tension at the wound site. Delayed primary closure occurs once a suspected infection has been cleared. Deep partial and full thickness burns both require surgical intervention. Surgery normally takes place within the first 5 days post injury to prevent infection which could extend the depth of the tissue loss (Glassey 2004).
29
Figure11. The reconstructive ladder, procedures ranging from simplest to most complex. (Ataturk University School of Medicine 2009)
4.3 Skin Grafts
“A skin graft is the transportation of skin from one area of the body to another.” (Glassey 2004)
A graft is an area of skin that is separated from its own blood supply and requires a highly vascular recipient bed in order for it to be successful. Prior to grafting, the process of wound debridement must take place. Wound debridement involves removing necrotic tissue, foreign debris, and reducing the bacterial load on the wound surface (Cardinal et al 2009).This is believed to encourage better healing. The following are the methods available for grafting onto a debrided wound to obtain closure:
∙ Autograft (‘split skin graft’) (own skin)
∙ Allograft (donor skin)
∙ Heterograft or xenografts (animal skin)
∙ Cultured skin
∙ Artificial skin (Glassey 2004)
30
4.31 Meshed vs. Sheet Grafts
Sheet grafts are those which are not altered once they have been taken from the donor site.
Meshed grafts are those which are passed through a machine that places fenestrations (small holes) in the graft. Meshed grafts have advantages over sheet grafts of 1) allowing the leakage of serum and blood which prevents haematomas and seromas and 2) they can be expanded to cover a larger surface area.
(Klein 2010)
4.311 Criteria to be met Pre- Grafting
∙ Diagnosis of DEEP tissue loss
∙ Patient is systemically fit for surgery
∙ Patient has no coagulation abnormalities ∙ Sufficient donor sites available
Figure12. Diagrams illustrating the process of mesh graft procedure (www.beltina .org)
∙ Would clear of streptococcus (Glassey 2004) 4.312 The Donor Site
The thigh is the most common donor site for split thickness skin grafts (STSG). A split thickness graft involves a portion of the thickness of the dermis while a full thickness skin graft (FTSG) involves the entire thickness of the dermis (Klein 2010). The most common site for full thickness skin grafts is the groin. Cosmetic areas such as the face should be avoided for graft donation.
The donor site should just be left with a superficial or a superficial partial thickness wound which will heal in 10-14 days and may be reused if necessary. Often, the donor site can be more painful than the recipient due to exposure of nerve endings (Glassey 2004).
31
4.313 Skin Substitutes
“Skin Substitutes are defined as a heterogeneous group of wound cover materials that aid in wound closure and replace the functions of the skin either temporarily or permanently”
(Halim et al 2010)
Conventionally, STSG and FTSG have been found to be the best option for burn wound coverage (Halim et al 2010). However, in cases of extensive burn injury, the supply of autografts is limited by additional wound or scarring at donor sites. For this reason, skin substitutes will be required. Skin substitutes require higher cost, expertise and experience than autografts. However, they also offer numerous advantages in the form of rapid wound coverage requiring a less vascularised wound bed, an increase in the dermal component of a healed wound, reduced inhibitory factors of wound healing, reduced inflammatory response and reduced scarring (Halim et al 2010).
Currently, there are various skin substitutes on the market but scientists and engineers are working towards producing the optimal skin substitute. As a general rule, skin substitutes are classified as either temporary or permanent and synthetic or biological. A very clear and concise overview of the different skin substitutes available for burn injuries is provided in Halim et al (2010).
4.314 The Recipient Site
The graft should take within 5 days and will provide a permanent covering of the injury. A graft should always be placed over bleeding, healthy tissue to ensure it is vascularised for survival (Glassey 2004).
Post-operatively the graft site is dressed to ensure pressure is created over the graft to limit haematoma formation. The body part is immobilised in an anti- deformity position at first in order to prevent shearing forces that could disrupt the graft (Edgar and Brereton 2004). Some very mobile body parts, such as the hand, may require splinting to ensure joint immobility.
4.315 Process of Graft ‘Take’
∙ Serum Inhibition (24-48hrs): fibrin layer formation and diffusion of fluid from the wound bed
32
∙ Inoscultation (day 3): capillary budding from the wound bed up into the base of the graft
∙ Capillary in-growth and remodelling (Glassey 2004) 4.316 Reasons for Graft Failure
∙ Inadequate blood supply to wound bed
∙ Graft movement
∙ Collection of fluid beneath graft (e.g. haematoma)
∙ Infection (e.g. streptococcus)
∙ The grafts properties (e.g. vascularity of donor site) (Glassey 2004)
4.4 Skin Flaps
The difference between a skin graft and a skin flap is that “a skin flap contains its own vasculature and therefore can be used to take over a wound bed that is avascular”. A skin graft does not have this ability (Glassey 2004). When speaking about grafts and flaps in the research, skin flaps is often incorporated into the term ‘skin grafts’.
Fig 13: skin flaps
(MicroSurgeon, 2012)
Tissues which a skin graft will not take over include and which a skin flap will include:
∙ Bone without periosteum
∙ Tendon without paratenon
∙ Cartilage without perichondrium (Glassey 2004)
33
4.41 Categorisation of Skin Flaps
Based on three factors:
1. Vascularity
2. Anatomical composition
3. Method of relocation (Glassey 2004)
- ↑ 1.0 1.1 Siemionow MZ, Eisenmann-Klein M, editors. Plastic and reconstructive surgery. Springer Science & Business Media; 2010 Jan 13.
- ↑ 2.0 2.1 Martin H. Immediate management of burn injury. 2007
- ↑ Feng Z, Tang Q, Lin J, He Q, Peng C. Application of animated cartoons in reducing the pain of dressing changes in children with burn injuries. International journal of burns and trauma. 2018;8(5):106.
- ↑ Zieliński J, Morawska-Kochman M, Zatoński T. Pain assessment and management in children in the postoperative period: A review of the most commonly used postoperative pain assessment tools, new diagnostic methods and the latest guidelines for postoperative pain therapy in children. Adv Clin Exp Med. 2020 Mar 1;29(3):365-74.
- ↑ 5.0 5.1 5.2 5.3 Foncerrada G, Culnan DM, Capek KD, González-Trejo S, Cambiaso-Daniel J, Woodson LC, Herndon DN, Finnerty CC, Lee JO. Inhalation injury in the burned patient. Annals of plastic surgery. 2018 Mar;80(3 Suppl 2):S98.
- ↑ Long B, Graybill JC, Rosenberg H. Just the facts: evaluation and management of thermal burns. Canadian Journal of Emergency Medicine. 2021 Nov 2:1-3.
- ↑ Lang TC, Zhao R, Kim A, Wijewardena A, Vandervord J, Xue M, Jackson CJ. A critical update of the assessment and acute management of patients with severe burns. Advances in wound care. 2019 Dec 1;8(12):607-33.