Diaphragm Rehabilitation: Difference between revisions
Carin Hunter (talk | contribs) No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
== Introduction == | == Introduction == | ||
Rehabilitation is a vital part of recovery, and for physiotherapists, it is integral to the treatment plan. | Rehabilitation is a vital part of recovery, and for physiotherapists, it is integral to the treatment plan. However, when patients sustain an injury which causes damage to the diaphragm, or have been on a ventilator, this muscle is often overlooked in the rehabilitation plan. The [[How We Breathe#Basics of Breathing|diaphragm]], which is the main respiratory muscle, works constantly throughout the day and performs many different breaths and breath holds. Retraining the diaphragm is, therefore, crucial for optimal function. | ||
== | == Causes of Diaphragm Dysfunction == | ||
Some causes of diaphragm dysfunction are discussed below: | |||
=== Surgical Diagnoses === | |||
*'''Congenital Diaphragmatic Hernia:''' One or more of a person's abdominal organs (i.e. stomach, spleen, liver, intestines) move upwards into the chest through a defect in the diaphragm. Congenital hernias are considered a medical emergency and require prompt surgery.<ref>Petrosyan M, Shah AA, Chahine AA, Guzzetta PC, Sandler AD, Kane TD. [https://www.sciencedirect.com/science/article/abs/pii/S0022346818304457 Congenital paraesophageal hernia: Contemporary results and outcomes of laparoscopic approach to repair in symptomatic infants and children.] Journal of pediatric surgery. 2019 Jul 1;54(7):1346-50.</ref> | |||
* | *'''Acquired Diaphragmatic Hernia (ADH):''' Usually caused by a penetrating injury (e.g. gun shot wound, stabbing) or a blunt injury (e.g. fall, motor vehicle accident). Penetrating injuries are a far more common cause of diaphragmatic rupture and subsequent hernias than blunt injuries.<ref>Newbury A, Dorfman JD, Lo HS. [https://www.sciencedirect.com/science/article/abs/pii/S0887217118300313 Imaging and management of thoracic trauma.] InSeminars in Ultrasound, CT and MRI 2018 Aug 1 (Vol. 39, No. 4, pp. 347-354). WB Saunders.</ref> | ||
* | |||
== | === Diaphragm Atrophy Secondary to Mechanical Ventilation === | ||
* After an individual has been on mechanical ventilation for an extended period of time, they may experience [[Diaphragmatic Breathing and Ventilator-Induced Diaphragmatic Dysfunction|disuse atrophy]]. This is caused by decreased protein synthesis,<ref>Ku Z, Yang JI, Menon VA, Thomason DB. [https://journals.physiology.org/doi/abs/10.1152/ajpcell.1995.268.6.C1369 Decreased polysomal HSP-70 may slow polypeptide elongation during skeletal muscle atrophy.] American Journal of Physiology-Cell Physiology. 1995 Jun 1;268(6):C1369-74.</ref> increased proteolysis<ref>Bodine SC, Latres E, Baumhueter S, Lai VK, Nunez L, Clarke BA, Poueymirou WT, Panaro FJ, Na E, Dharmarajan K, Pan ZQ. [https://www.science.org/doi/abs/10.1126/science.1065874 Identification of ubiquitin ligases required for skeletal muscle atrophy.] Science. 2001 Nov 23;294(5547):1704-8.</ref> or combination of both factors after mechanical ventilation. | |||
* Oxidative stress: "defined as a disturbance in the balance between the production of reactive oxygen species (free radicals) and antioxidant defenses".<ref>Betteridge DJ. [https://www.sciencedirect.com/science/article/abs/pii/S0026049500800773 What is oxidative stress?]. Metabolism. 2000 Feb 1;49(2):3-8.</ref> Oxidative stress starts to occur within six hours of continuous [[Ventilation and Weaning|mechanical ventilation]] and it is linked to diaphragmatic dysfunction and weakness.<ref>Zergeroglu MA, McKenzie MJ, Shanely RA, Van Gammeren D, DeRuisseau KC, Powers SK. [https://journals.physiology.org/doi/full/10.1152/japplphysiol.00824.2002 Mechanical ventilation-induced oxidative stress in the diaphragm.] Journal of applied physiology. 2003 Sep;95(3):1116-24.</ref> This phenomenon also occurs in skeletal muscles, but it takes longer to set in.<ref>Kondo HI, Miura MI, Nakagaki IK, Sasaki SA, Itokawa YO. [https://journals.physiology.org/doi/abs/10.1152/ajpendo.1992.262.5.e583 Trace element movement and oxidative stress in skeletal muscle atrophied by immobilization.] American Journal of Physiology-Endocrinology And Metabolism. 1992 May 1;262(5):E583-90.</ref> | |||
* A study conducted by Grosu and Lee<ref name=":1" /> in 2017 concluded there was no relationship between changes in diaphragm thickness and extubation outcome.<ref name=":1">Grosu HB, Ost DE, Im Lee Y, Song J, Li L, Eden E, Rose K. [http://rc.rcjournal.com/content/62/7/904.short Diaphragm muscle thinning in subjects receiving mechanical ventilation and its effect on extubation.] Respiratory care. 2017 Jul 1;62(7):904-11.</ref> However, Goligher et al.<ref name=":2">Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, Vorona S, Sklar MC, Rittayamai N, Lanys A, Murray A. [https://www.atsjournals.org/doi/full/10.1164/rccm.201703-0536OC Mechanical ventilation–induced diaphragm atrophy strongly impacts clinical outcomes.] American journal of respiratory and critical care medicine. 2018 Jan 15;197(2):204-13.</ref> reached the conclusion that diaphragmatic atrophy that developed while a patient was on mechanical ventilation had a strong influence over the clinical outcome: "Targeting an inspiratory effort level similar to that of healthy subjects at rest might accelerate an individual's liberation from ventilation."<ref name=":2" /> | |||
* There are a number of studies to highlight the benefits of [[Physiotherapists Role in ICU|early rehabilitation in ICU]]. Early rehabilitation can lessen the amount of dysfunction caused by mechanical ventilation and can assist a patient's extubation. <ref>Dong Z, Liu Y, Gai Y, Meng P, Lin H, Zhao Y, Xing J. [https://bmcpulmmed.biomedcentral.com/articles/10.1186/s12890-021-01461-2 Early rehabilitation relieves diaphragm dysfunction induced by prolonged mechanical ventilation: a randomised control study.] BMC pulmonary medicine. 2021 Dec;21(1):1-8.</ref> | |||
* The Manual Evaluation Diaphragm<ref>Bordoni B, Morabito B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6605963/ The Diaphragm Muscle Manual Evaluation Scale.] Cureus. 2019 Apr;11(4).</ref> (MED) Scale is the only evaluation scale in the world to generate a value for the mobility of the diaphragm. | |||
** The MED Scale has been designed to make use of a therapist's palpations skills during evaluation. This means it is the first non-instrumental evaluation tool designed for assessing the diaphragm function. | |||
** Please read the following article for more information on [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6605963/#:~:text=Manual%20evaluation%20of%20the%20diaphragm%20is%20an%20important%20tool%20for,areas%2C%20both%20passively%20and%20actively. The Diaphragm Muscle Manual Evaluation Scale].<ref>Bordoni B, Morabito B. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6605963/ The Diaphragm Muscle Manual Evaluation Scale]. ''Cureus''. 2019;11(4):e4569.</ref> | |||
== Techniques to Strengthen the Diaphragm == | |||
# Sandbag breathing | # Sandbag breathing | ||
# Deep | # Deep chest breathing | ||
# Bellow’s | # Bellow’s breath | ||
# Intercostal | # Intercostal stretching breath | ||
# Focused | # Focused diaphragmatic breath | ||
# Diaphragm stretches | # Diaphragm stretches | ||
# | # Transversus abdominis activation | ||
# Straw breathing | # Straw breathing | ||
# Cat- | # Cat-cow pose<ref name=":3">Pandya R. Rehabilitating the Diaphragm Course. Physioplus, 2022</ref> | ||
=== 1. Sandbag | === 1. Sandbag Breathing === | ||
[[File:Sandbag breathing.jpg|right|frameless|270x270px]] | [[File:Sandbag breathing.jpg|right|frameless|270x270px|alt=|Figure 1. Sandbag breathing.]] | ||
The patient lies in a supine position. The spine is not bent to either side. | The patient lies in a supine position (Figure 1). The spine is not bent to either side. | ||
Establish a flow of relaxed breathing | Establish a flow of relaxed breathing with the following three steps:<ref name=":3" /> | ||
# Feel the breath flowing out and in, repeatedly. | # Feel the breath flowing out and in, repeatedly. | ||
| Line 41: | Line 44: | ||
{{#ev:youtube|xJabf_p-B9E}} | {{#ev:youtube|xJabf_p-B9E}} | ||
=== 2. Deep Chest Breathing === | === 2. Deep Chest Breathing === | ||
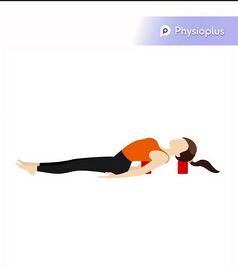
[[File:Chest expansion.jpg|right|frameless|270x270px]] | [[File:Chest expansion.jpg|right|frameless|270x270px|alt=|Figure 2. Deep chest breathing.]] | ||
The patient should sit on the floor and place two yoga blocks on the floor behind them. One should be lying flat and the other should be at medium height. | The patient should sit on the floor and place two yoga blocks on the floor behind them (Figure 2). One block should be lying flat and the other should be at medium height. The patient then needs to lay their shoulder blades on the flat block and their head on the medium height block, as shown in Figure 2. Relax arms out to each side with palms faced upwards with legs stretched out in front. Inhale deeply and allow chest to completely rise.<ref name=":3" /> | ||
On the exhale, allow | On the exhale, allow the stomach to fall first, then the diaphragm, then the lungs and finally the chest. | ||
Repeat this exercise nine times with a regular breath | Repeat this exercise nine times with a regular breath between each repetition. | ||
Deep chest breathing will help to tone both the diaphragm and the intercostal muscles. | Deep chest breathing will help to tone both the diaphragm and the intercostal muscles.<ref name=":3" /> | ||
=== 3. Bellow’s Breath === | === 3. Bellow’s Breath === | ||
Bellow’s breath is a detoxifying breathing exercise. To carry out this exercise | Bellow’s breath is a detoxifying breathing exercise. To carry out this exercise, the client needs to be in a seated position. Once comfortable, the client inhales naturally through their nose. On the exhale, they need to snap their stomach muscles in, forcing the exhalation. Repeat this breathing pattern for 30 seconds, gradually increasing the pace.<ref name=":3" /> | ||
{{#ev:youtube|EfcXiEBiDBE}} | {{#ev:youtube|EfcXiEBiDBE}} | ||
=== 4. Intercostal Stretching Breath === | === 4. Intercostal Stretching Breath === | ||
To perform an intercostal stretching breath, begin in a standing position and stretch both of | To perform an intercostal stretching breath, begin in a standing position and stretch both of arms over the head. Inhale deeply and on the exhale, stretch both arms to the right, stretching the intercostal muscles on the left side of your body. | ||
Inhale and come back to the center; | Inhale and come back to the center; | ||
On the next exhale, stretch | On the next exhale, stretch arms to the left, feeling the a stretch in the right intercostal muscles. | ||
Repeat two more times on each side. | Repeat two more times on each side.<ref name=":3" /> | ||
=== 5. Focused Diaphragmatic Breath === | === 5. Focused Diaphragmatic Breath === | ||
When performing a | When performing a focused diaphragmatic breath, the patient first should understand exactly where their diaphragm is. Take their fingers and place them on the bottom of their sternum. Instruct them to take a few breaths and feel their diaphragm move under their fingers. | ||
To perform this breathing exercise, tense | To perform this breathing exercise, the patient must tense their stomach muscles and keep their fingers on the diaphragm. Inhale and exhale several times, focusing on the diaphragm’s movement. | ||
This exercise can help increase awareness of and tone the diaphragm. | This exercise can help increase awareness of and tone the diaphragm.<ref name=":3" /> | ||
=== 6. Diaphragm Stretches === | === 6. Diaphragm Stretches === | ||
To perform a | To perform a diaphragm stretch,<ref name=":0">Rathore M, Trivedi S, Abraham J, Sinha MB. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5433114/ Anatomical correlation of core muscle activation in different yogic postures.] International Journal of Yoga. 2017 May;10(2):59.</ref> the patient should begin in supine, in 90/90 hip-knee flexion. Place the heels of the patient's hands on their thighs, close to the hip creases. They should breathe calmly through their nose a few times. After a deep inhalation and full exhalation, the client should push their hands into their thighs. At this point, they should think about inhaling without actually breathing any air in. They then should suck their belly in and expand their ribs, which creates a vacuum. The client should then make small movements to bring their spine and pelvis into flexion, extension. Introducing lateral shifts will also increase the stretch in different parts of the diaphragm. Breathe normally during one to two cycles and repeat five times.<ref name=":4" /> | ||
=== 7. Transversus Abdominis Activation: === | === 7. Transversus Abdominis Activation: === | ||
| Line 79: | Line 82: | ||
As a progression, repeat the exercise above and at the end of exhalation lift both feet an inch off the floor. Hold during inhalation before lightly placing your feet back down. | As a progression, repeat the exercise above and at the end of exhalation lift both feet an inch off the floor. Hold during inhalation before lightly placing your feet back down. | ||
=== 8. Straw breathing<ref>Bech-Hanssen G, ed. [https://www.yogajournal.com/teach/anatomy-yoga-practice/why-your-diaphragm-could-be-core-strength-game-changer/ Why Your Diaphragm Could Be the Core Strength Game-Changer You’ve Overlooked.] yoga journal; Sep 28, 2018 ORIGINAL:Nov 7, 2017.</ref> === | === 8. Straw breathing<ref name=":4">Bech-Hanssen G, ed. [https://www.yogajournal.com/teach/anatomy-yoga-practice/why-your-diaphragm-could-be-core-strength-game-changer/ Why Your Diaphragm Could Be the Core Strength Game-Changer You’ve Overlooked.] yoga journal; Sep 28, 2018 ORIGINAL:Nov 7, 2017.</ref> === | ||
For this exercise, hold a straw between your lips, inhale through your nose and exhale through the straw. | For this exercise, hold a straw between your lips, inhale through your nose and exhale through the straw. | ||
Revision as of 10:40, 13 February 2022
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson and Ewa Jaraczewska
Introduction[edit | edit source]
Rehabilitation is a vital part of recovery, and for physiotherapists, it is integral to the treatment plan. However, when patients sustain an injury which causes damage to the diaphragm, or have been on a ventilator, this muscle is often overlooked in the rehabilitation plan. The diaphragm, which is the main respiratory muscle, works constantly throughout the day and performs many different breaths and breath holds. Retraining the diaphragm is, therefore, crucial for optimal function.
Causes of Diaphragm Dysfunction[edit | edit source]
Some causes of diaphragm dysfunction are discussed below:
Surgical Diagnoses[edit | edit source]
- Congenital Diaphragmatic Hernia: One or more of a person's abdominal organs (i.e. stomach, spleen, liver, intestines) move upwards into the chest through a defect in the diaphragm. Congenital hernias are considered a medical emergency and require prompt surgery.[1]
- Acquired Diaphragmatic Hernia (ADH): Usually caused by a penetrating injury (e.g. gun shot wound, stabbing) or a blunt injury (e.g. fall, motor vehicle accident). Penetrating injuries are a far more common cause of diaphragmatic rupture and subsequent hernias than blunt injuries.[2]
Diaphragm Atrophy Secondary to Mechanical Ventilation[edit | edit source]
- After an individual has been on mechanical ventilation for an extended period of time, they may experience disuse atrophy. This is caused by decreased protein synthesis,[3] increased proteolysis[4] or combination of both factors after mechanical ventilation.
- Oxidative stress: "defined as a disturbance in the balance between the production of reactive oxygen species (free radicals) and antioxidant defenses".[5] Oxidative stress starts to occur within six hours of continuous mechanical ventilation and it is linked to diaphragmatic dysfunction and weakness.[6] This phenomenon also occurs in skeletal muscles, but it takes longer to set in.[7]
- A study conducted by Grosu and Lee[8] in 2017 concluded there was no relationship between changes in diaphragm thickness and extubation outcome.[8] However, Goligher et al.[9] reached the conclusion that diaphragmatic atrophy that developed while a patient was on mechanical ventilation had a strong influence over the clinical outcome: "Targeting an inspiratory effort level similar to that of healthy subjects at rest might accelerate an individual's liberation from ventilation."[9]
- There are a number of studies to highlight the benefits of early rehabilitation in ICU. Early rehabilitation can lessen the amount of dysfunction caused by mechanical ventilation and can assist a patient's extubation. [10]
- The Manual Evaluation Diaphragm[11] (MED) Scale is the only evaluation scale in the world to generate a value for the mobility of the diaphragm.
- The MED Scale has been designed to make use of a therapist's palpations skills during evaluation. This means it is the first non-instrumental evaluation tool designed for assessing the diaphragm function.
- Please read the following article for more information on The Diaphragm Muscle Manual Evaluation Scale.[12]
Techniques to Strengthen the Diaphragm[edit | edit source]
- Sandbag breathing
- Deep chest breathing
- Bellow’s breath
- Intercostal stretching breath
- Focused diaphragmatic breath
- Diaphragm stretches
- Transversus abdominis activation
- Straw breathing
- Cat-cow pose[13]
1. Sandbag Breathing[edit | edit source]
The patient lies in a supine position (Figure 1). The spine is not bent to either side.
Establish a flow of relaxed breathing with the following three steps:[13]
- Feel the breath flowing out and in, repeatedly.
- Soften the abdomen and feel it rise as you inhale and fall as you exhale.
- Let the breath flow without pause between the breaths.
2. Deep Chest Breathing[edit | edit source]
The patient should sit on the floor and place two yoga blocks on the floor behind them (Figure 2). One block should be lying flat and the other should be at medium height. The patient then needs to lay their shoulder blades on the flat block and their head on the medium height block, as shown in Figure 2. Relax arms out to each side with palms faced upwards with legs stretched out in front. Inhale deeply and allow chest to completely rise.[13]
On the exhale, allow the stomach to fall first, then the diaphragm, then the lungs and finally the chest.
Repeat this exercise nine times with a regular breath between each repetition.
Deep chest breathing will help to tone both the diaphragm and the intercostal muscles.[13]
3. Bellow’s Breath[edit | edit source]
Bellow’s breath is a detoxifying breathing exercise. To carry out this exercise, the client needs to be in a seated position. Once comfortable, the client inhales naturally through their nose. On the exhale, they need to snap their stomach muscles in, forcing the exhalation. Repeat this breathing pattern for 30 seconds, gradually increasing the pace.[13]
4. Intercostal Stretching Breath[edit | edit source]
To perform an intercostal stretching breath, begin in a standing position and stretch both of arms over the head. Inhale deeply and on the exhale, stretch both arms to the right, stretching the intercostal muscles on the left side of your body.
Inhale and come back to the center;
On the next exhale, stretch arms to the left, feeling the a stretch in the right intercostal muscles.
Repeat two more times on each side.[13]
5. Focused Diaphragmatic Breath[edit | edit source]
When performing a focused diaphragmatic breath, the patient first should understand exactly where their diaphragm is. Take their fingers and place them on the bottom of their sternum. Instruct them to take a few breaths and feel their diaphragm move under their fingers.
To perform this breathing exercise, the patient must tense their stomach muscles and keep their fingers on the diaphragm. Inhale and exhale several times, focusing on the diaphragm’s movement.
This exercise can help increase awareness of and tone the diaphragm.[13]
6. Diaphragm Stretches [edit | edit source]
To perform a diaphragm stretch,[14] the patient should begin in supine, in 90/90 hip-knee flexion. Place the heels of the patient's hands on their thighs, close to the hip creases. They should breathe calmly through their nose a few times. After a deep inhalation and full exhalation, the client should push their hands into their thighs. At this point, they should think about inhaling without actually breathing any air in. They then should suck their belly in and expand their ribs, which creates a vacuum. The client should then make small movements to bring their spine and pelvis into flexion, extension. Introducing lateral shifts will also increase the stretch in different parts of the diaphragm. Breathe normally during one to two cycles and repeat five times.[15]
7. Transversus Abdominis Activation:[edit | edit source]
When performing Transversus Abdominis activation[14] the patient should lie on their back with their knees bent (crook lying). Place their feet hip-width apart and a block lengthwise between their thighs. Make sure their pelvis and low back are in neutral, place their fingertips on their lower abdomen, just between their front hip bones (ASIS).
On exhalation, instruct the patient to drop their belly button, engage the pelvic floor, and squeeze the block. They should be feeling for the transversus abdominis tensing under their fingertips. It is key that the patient maintains the neutral curve of the spine as their belly drops. On inhalation, relax and soften the belly. Complete a few times to find the deep activation of your core.
As a progression, repeat the exercise above and at the end of exhalation lift both feet an inch off the floor. Hold during inhalation before lightly placing your feet back down.
8. Straw breathing[15][edit | edit source]
For this exercise, hold a straw between your lips, inhale through your nose and exhale through the straw.
Breathing out through a long straw will automatically make your exhalation longer than the inhalation.
9. Cat-Cow Pose[edit | edit source]
Start this exercise in 4 point kneeling. Breathe in through your nose and out through your mouth.
When the patient breathes in, instruct them to drop their stomach down towards the floor and hollow their back.
When they breathe out, instruct them to round their back and tuck their chin toward their chest. Keep rounding as you blow all the air out of the lungs. Pause at the end of your exhale for five seconds, holding the rounded position. Then, breathe in through your nose again.
8. Diaphragm Stretches in Standing[edit | edit source]
The fibres being targeted by this stretch are mostly located between the 12th rib and the central tendon along the inside of the rib cage, which is called the Zone of Apposition.
Stand in a comfortable position and begin by stretching the left side of the diaphragm. Lift your left arm over your head, and place your right hand on your lower ribs on the left side.
On exhalation, laterally flex the spine to the right. There are two factors causing the diaphragm to lengthen as this movement is performed, firstly, the exhalation, and secondly the increase in distance between the 12th rib and the top of the diaphragm.
Inhale as you return to the upright position.
Repeat the movement for five breath cycles.
Exhale as you move to the right and inhale as you return to the upright position.
Step 1 - 3, showing the Diaphragm Stretch in Standing[13]
- Step 1: To increase the stretch, gently push down on the left lower ribs (7-12) with your right hand. Repeat the movement on the opposite side for five cycles of breath. As you move to the left, exhale and as you return to the upright position, inhale.
- Step 2: Finally, reach up with both arms and clasp your hands. Laterally flex your spine to the right and left. During lateral flexion, exhale and when you return to the centre, inhale. Move to the right and left four times.
- Step 3: To finish the exercise, reach up with both arms and clasp your hands. Laterally flex your spine to the right and left. During lateral flexion, exhale and when you return to center, inhale. Move to the right and left four times.
Additional Breathing Techniques[edit | edit source]
Paradoxical Breathing[edit | edit source]
Pranayama Breathing Techniques[edit | edit source]
Ujjayi Breathing[edit | edit source]
Bellows Breathing[edit | edit source]
Diaphragm Release[edit | edit source]
Myofascial Release for the Diaphragm[edit | edit source]
References[edit | edit source]
- ↑ Petrosyan M, Shah AA, Chahine AA, Guzzetta PC, Sandler AD, Kane TD. Congenital paraesophageal hernia: Contemporary results and outcomes of laparoscopic approach to repair in symptomatic infants and children. Journal of pediatric surgery. 2019 Jul 1;54(7):1346-50.
- ↑ Newbury A, Dorfman JD, Lo HS. Imaging and management of thoracic trauma. InSeminars in Ultrasound, CT and MRI 2018 Aug 1 (Vol. 39, No. 4, pp. 347-354). WB Saunders.
- ↑ Ku Z, Yang JI, Menon VA, Thomason DB. Decreased polysomal HSP-70 may slow polypeptide elongation during skeletal muscle atrophy. American Journal of Physiology-Cell Physiology. 1995 Jun 1;268(6):C1369-74.
- ↑ Bodine SC, Latres E, Baumhueter S, Lai VK, Nunez L, Clarke BA, Poueymirou WT, Panaro FJ, Na E, Dharmarajan K, Pan ZQ. Identification of ubiquitin ligases required for skeletal muscle atrophy. Science. 2001 Nov 23;294(5547):1704-8.
- ↑ Betteridge DJ. What is oxidative stress?. Metabolism. 2000 Feb 1;49(2):3-8.
- ↑ Zergeroglu MA, McKenzie MJ, Shanely RA, Van Gammeren D, DeRuisseau KC, Powers SK. Mechanical ventilation-induced oxidative stress in the diaphragm. Journal of applied physiology. 2003 Sep;95(3):1116-24.
- ↑ Kondo HI, Miura MI, Nakagaki IK, Sasaki SA, Itokawa YO. Trace element movement and oxidative stress in skeletal muscle atrophied by immobilization. American Journal of Physiology-Endocrinology And Metabolism. 1992 May 1;262(5):E583-90.
- ↑ 8.0 8.1 Grosu HB, Ost DE, Im Lee Y, Song J, Li L, Eden E, Rose K. Diaphragm muscle thinning in subjects receiving mechanical ventilation and its effect on extubation. Respiratory care. 2017 Jul 1;62(7):904-11.
- ↑ 9.0 9.1 Goligher EC, Dres M, Fan E, Rubenfeld GD, Scales DC, Herridge MS, Vorona S, Sklar MC, Rittayamai N, Lanys A, Murray A. Mechanical ventilation–induced diaphragm atrophy strongly impacts clinical outcomes. American journal of respiratory and critical care medicine. 2018 Jan 15;197(2):204-13.
- ↑ Dong Z, Liu Y, Gai Y, Meng P, Lin H, Zhao Y, Xing J. Early rehabilitation relieves diaphragm dysfunction induced by prolonged mechanical ventilation: a randomised control study. BMC pulmonary medicine. 2021 Dec;21(1):1-8.
- ↑ Bordoni B, Morabito B. The Diaphragm Muscle Manual Evaluation Scale. Cureus. 2019 Apr;11(4).
- ↑ Bordoni B, Morabito B. The Diaphragm Muscle Manual Evaluation Scale. Cureus. 2019;11(4):e4569.
- ↑ 13.0 13.1 13.2 13.3 13.4 13.5 13.6 13.7 Pandya R. Rehabilitating the Diaphragm Course. Physioplus, 2022
- ↑ 14.0 14.1 Rathore M, Trivedi S, Abraham J, Sinha MB. Anatomical correlation of core muscle activation in different yogic postures. International Journal of Yoga. 2017 May;10(2):59.
- ↑ 15.0 15.1 Bech-Hanssen G, ed. Why Your Diaphragm Could Be the Core Strength Game-Changer You’ve Overlooked. yoga journal; Sep 28, 2018 ORIGINAL:Nov 7, 2017.