Amyotrophic Lateral Sclerosis (ALS): A Case Study: Difference between revisions
Kara Blair (talk | contribs) No edit summary |
No edit summary |
||
| (6 intermediate revisions by 2 users not shown) | |||
| Line 2: | Line 2: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | ||
== Abstract == | == Abstract == | ||
Amyotrophic Lateral Sclerosis (ALS) is a rare neurological disease that involves the degeneration of neurons responsible for controlling voluntary muscle movement ( | Amyotrophic Lateral Sclerosis (ALS) is a rare neurological disease that involves the degeneration of neurons responsible for controlling voluntary muscle movement<ref name=":0">Amyotrophic Lateral Sclerosis (ALS) Fact Sheet [Internet]. Bethesda, MD 20892: National Institute of Neurological Disorders and Stroke; [cited 2021May11]. Available from: https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/amyotrophic-lateral-sclerosis-als-fact-sheet </ref>. Ultimately, most people with ALS die within 3-5 years after symptom onset due to respiratory failure<ref name=":0" />. This fictional case study involves a 24-year-old male diagnosed with early-stage juvenile ALS 6 months prior. This case study documents the subjective and objective findings from the patient’s initial physiotherapy assessment, and additional findings 6-weeks after beginning physiotherapy treatment. Moreover, potential physiotherapy interventions are outlined, with the goal being to maintain the patient’s strength, balance, and overall functional independence despite having a progressive degenerative disease. Furthermore, this case study highlights the importance of a multidisciplinary team approach to managing progressive degenerative diseases such as ALS. Together, the interdisciplinary team can address the wide range of signs and symptoms, the various biopsychosocial implications, and finally, work towards achieving patient specific goals. | ||
== Introduction == | == Introduction == | ||
{{#ev:youtube|aDpN-6EAd3k}}<ref>The ALS Association. What is ALS?. Available from: https://www.youtube.com/watch?v=aDpN-6EAd3k [last accessed 5/10/2021]</ref> | {{#ev:youtube|aDpN-6EAd3k}}<ref>The ALS Association. What is ALS?. Available from: https://www.youtube.com/watch?v=aDpN-6EAd3k [last accessed 5/10/2021]</ref> | ||
[https://physio-pedia.com/Amyotrophic_Lateral_Sclerosis?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Amyotrophic lateral sclerosis (ALS)] is a progressive neuromuscular disease that involves the neurons responsible for controlling voluntary muscle movement | [https://physio-pedia.com/Amyotrophic_Lateral_Sclerosis?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Amyotrophic lateral sclerosis (ALS)] is a progressive neuromuscular disease that involves the neurons responsible for controlling voluntary muscle movement<ref name=":0" />. ALS most commonly appears between the ages of 55 to 75 but can impact individuals within any age group<ref name=":0" />. In ALS, both the upper motor neurons and lower motor neurons degenerate, and therefore, stop sending signals to the muscles<ref name=":0" />. This interruption in signalling results in weakening of the muscles, twitching—known as fasciculations—and muscle wasting. The early symptoms usually involve muscle weakness and eventually progress to the inability to speak, eat, move, or breathe<ref name=":0" />. [https://physio-pedia.com/index.php?title=Respiratory_Failure&veaction=edit§ion=1?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Respiratory failure] is the dominant cause of death in individuals with ALS and usually occurs within 3 to 5 years from the onset of symptoms<ref name=":0" />. Approximately 70% of patients with ALS present with limb-onset ALS—weakness in the arms and legs—and the remaining patients present with bulbar-onset ALS, which manifests with [https://physio-pedia.com/Dysarthria?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal dysarthria]—motor speech disorder—and [https://physio-pedia.com/Dysphagia?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal dysphagia]—difficulty swallowing<ref name=":1">Jamrozik Z, Gawel M, Szacka K, Bakon L. A case report of amyotrophic lateral sclerosis in a patient with Klippel–Feil Syndrome—a familial occurrence: A potential ole of TGF-β signaling pathway. Medicine[Internet]. 2015 Jan [cited 2021 May 10];94(4). doi: 10.1097/MD.0000000000000441</ref>. | ||
The clinical presentation of ALS is not homogenous. There is considerable variability in the phenotypical expression of ALS, as shown throughout the literature. Jamorzik et al. | The clinical presentation of ALS is not homogenous. There is considerable variability in the phenotypical expression of ALS, as shown throughout the literature. Jamorzik et al.<ref name=":1" /> discuss a 68-year-old man who first presented with dysarthria in July 2012, and began experiencing generalized fasciculations several months later. A year later, the patient’s speech became more slurred, but he did not present with muscular atrophy or weakness. Clinical evaluations supported by electrophysiological and biochemical testing led to the diagnosis of bulbar-onset ALS<ref name=":1" />. Conversely, Venizelos, Park & Fisher<ref name=":2">Venizelos A, Park Y, Fisher MA. A patient with amyotrophic lateral sclerosis and atypical clinical and electrodiagnostic features: a case report. Journal of medical case reports. 2011 Dec [cited 2021 May 13];5(1):1-5. doi: 10.1186/1752-1947-5-538</ref> presented a case of a 57-year-old Caucasian male who began experiencing unexplained bilateral lower extremity weakness and fasciculations. Within five months, his lower extremity weakness progressed until he was unable to stand independently. He also presented with muscular atrophy in the upper extremities, specifically in the intrinsic hand muscles. Despite being diagnosed with multiple other diseases, including [https://physio-pedia.com/Chronic_Inflammatory_Demyelinating_Polyneuropathy_(CIDP)?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal chronic inflammatory demyelinated polyneuropathy (CIDP)], the patient was later diagnosed with ALS and died one year after symptom onset<ref name=":1" />. In an additional study, Majmudar, Wu, and Paganoni<ref name=":3">Majmudar S, Wu J, Paganoni S. Rehabilitation in amyotrophic lateral sclerosis: why it matters. Muscle & Nerve [Internet]. 2014 Jul [cited 2021 May 9];50(1):4-13. doi: 10.1002/mus.24202.</ref> discussed a case involving a 45-year-old female patient who presented with an early stage of ALS. This patient first began experiencing right leg and arm weakness, fatigue and suffered from several falls while playing with her kids. Additionally, she expressed having difficulty with activities involving fine motor control, such as cutting food and doing up buttons on clothing<ref name=":3" />. | ||
There is currently no cure for ALS, however, [https://www.mayoclinic.org/drugs-supplements/riluzole-oral-route/side-effects/drg-20065853?p=1 riluzole] is a medication that is moderately effective at prolonging life for individuals with ALS by two to three months | There is currently no cure for ALS, however, [https://www.mayoclinic.org/drugs-supplements/riluzole-oral-route/side-effects/drg-20065853?p=1 riluzole] is a medication that is moderately effective at prolonging life for individuals with ALS by two to three months<ref name=":2" />. Moreover, physiotherapy in conjunction with other forms of healthcare has shown to be beneficial for symptom management, optimizing functional independence, and increasing quality of life in those with ALS. Management for ALS should be tailored to the individual to meet their individual needs and goals<ref name=":3" />. Majmudar et al.<ref name=":3" /> suggested that exercise, energy conservation techniques, stretching, and range of motion (ROM), as well as assistive devices for gait, may be appropriate for early-stage ALS. However, the individual should be monitored for signs of overexertion, excessive fatigue, and an increase in pain<ref name=":3" />. Tsitkanou et al.<ref>Tsitkanou S, Della Gatta P, Foletta V, Russell A. The role of exercise as a non-pharmacological therapeutic approach for amyotrophic lateral sclerosis: beneficial or detrimental?. Frontiers in neurology [Internet]. 2019 Jul 17 [cited 2021 May 13];10:783. doi: 10.3389/fneur.2019.00783</ref> demonstrated that both endurance and resistance training have a beneficial impact on quality of life; however, they do not extend life expectancy. | ||
The purpose of this report is to create a realistic picture of a young individual diagnosed with early-stage ALS. A fictional case study will be used to illustrate the progressive nature of the disease, outline the process of a physiotherapy assessment and identify the likely findings for patients with ALS. Physiotherapy interventions for ALS, supported by the work of other healthcare professionals, focus on maximizing patients’ mobility, respiratory function, independence, and quality of life | The purpose of this report is to create a realistic picture of a young individual diagnosed with early-stage ALS. A fictional case study will be used to illustrate the progressive nature of the disease, outline the process of a physiotherapy assessment and identify the likely findings for patients with ALS. Physiotherapy interventions for ALS, supported by the work of other healthcare professionals, focus on maximizing patients’ mobility, respiratory function, independence, and quality of life<ref name=":3" />. Therefore, this report will also outline various physiotherapy interventions that assist in improving quality of life in patients with ALS. This case study was developed by integrating evidence-based research and clinical findings to educate other healthcare professionals on ALS and inform clinical decision-making. | ||
When taking on this project, we were aware that ALS is a very challenging condition, and much research is needed to fully understand the cause of the disease and develop a cure. However, an additional challenge we faced was developing a physiotherapy treatment plan that targeted the multitude of impairments experienced by those with ALS. This progressive disease can lead to impairments in balance, gait, dexterity, strength, and so on. Therefore, the requirement for a treatment plan to tackle the immense number of symptoms, as well as work to achieve patient specific goals, adds to the complexity of the disorder. | When taking on this project, we were aware that ALS is a very challenging condition, and much research is needed to fully understand the cause of the disease and develop a cure. However, an additional challenge we faced was developing a physiotherapy treatment plan that targeted the multitude of impairments experienced by those with ALS. This progressive disease can lead to impairments in balance, gait, dexterity, strength, and so on. Therefore, the requirement for a treatment plan to tackle the immense number of symptoms, as well as work to achieve patient specific goals, adds to the complexity of the disorder. | ||
| Line 19: | Line 19: | ||
== Client Characteristics == | == Client Characteristics == | ||
[[File:Soccer-ball.jpg|alt=A soccer player kicking a soccer ball in the field|thumb|[https://www.google.com/url?sa=i&url=https%3A%2F%2Factiveforlife.com%2Fthe-evolution-of-the-soccer-ball%2F&psig=AOvVaw05ZQ1tVOtsyzVl1wGnV3GF&ust=1621036196093000&source=images&cd=vfe&ved=2ahUKEwiK_K3G7MfwAhUERs0KHc3-AMQQr4kDegUIARDVAQ Figure 1]]] | [[File:Soccer-ball.jpg|alt=A soccer player kicking a soccer ball in the field|thumb|[https://www.google.com/url?sa=i&url=https%3A%2F%2Factiveforlife.com%2Fthe-evolution-of-the-soccer-ball%2F&psig=AOvVaw05ZQ1tVOtsyzVl1wGnV3GF&ust=1621036196093000&source=images&cd=vfe&ved=2ahUKEwiK_K3G7MfwAhUERs0KHc3-AMQQr4kDegUIARDVAQ Figure 1]]] | ||
A 24-year-old, R-hand dominant, Caucasian male, named Jared Miller. Jared lives with his parents—Jane and James Miller—and his sister Jaya in Perth, Ontario. Jared was previously an athlete on his high school soccer team. After completing his undergraduate degree in Kinesiology at [https://www.queensu.ca/ Queen's University], Jared hoped to obtain a doctorate in Dentistry. However, Jared unable able to pursue this career aspiration after being diagnosed with ALS 6-months ago. He first noticed changes in muscle strength after falling several times on the soccer field, and he has expressed a general feeling of weakness. Since the onset of these initial symptoms, Jared has been experiencing ongoing muscle weakness, cramping, and associated pain. Moreover, Jared was referred to physiotherapy by a neurologist. Despite having been diagnosed with ALS, Jared has no comorbid conditions. ( | A 24-year-old, R-hand dominant, Caucasian male, named Jared Miller. Jared lives with his parents—Jane and James Miller—and his sister Jaya in Perth, Ontario. Jared was previously an athlete on his high school soccer team. After completing his undergraduate degree in Kinesiology at [https://www.queensu.ca/ Queen's University], Jared hoped to obtain a doctorate in Dentistry. However, Jared unable able to pursue this career aspiration after being diagnosed with ALS 6-months ago. He first noticed changes in muscle strength after falling several times on the soccer field, and he has expressed a general feeling of weakness. Since the onset of these initial symptoms, Jared has been experiencing ongoing muscle weakness, cramping, and associated pain. Moreover, Jared was referred to physiotherapy by a neurologist. Despite having been diagnosed with ALS, Jared has no comorbid conditions<ref name=":4">Norman K, Stobäus N, Gonzalez MC, Schulzke JD, Pirlich M. Hand grip strength: outcome predictor and marker of nutritional status. Clin Nutr [Internet]. 2011 Apr 1 [cited 2021 May 9];30(2):135-42. doi: 10.1016/j.clnu.2010.09.010</ref>. | ||
== Examination Findings == | == Examination Findings == | ||
| Line 29: | Line 29: | ||
==== '''Patient Profile''' ==== | ==== '''Patient Profile''' ==== | ||
24-year-old male with ALS. DOB: 1996/02 | 24-year-old male with ALS. DOB: 1996/06/02 | ||
During the initial assessment the patient was friendly yet appeared to be saddened and of low spirit. Jared has done an abundance of research on ALS and was very focused on the poor prognosis associated with the disease. The patient reports feeling defeated due to a lack of available treatments for ALS and feeling as if he was a burden to his mother. Additionally, the patient communicated feelings as if his dreams were taken away from him. He explained that he stopped playing soccer as a result of increased cramping and weakness in his legs, as well as having difficulty breathing while running on the field. Jared stated that he misses both the physical and social aspect of playing soccer. His parents have noticed changes in Jared’s voice, but reported that Jared’s friends and other family members haven’t noticed much change. Jared explained that his body image has been impacted since his diagnosis, as he has seen noticeable changes in his muscle mass. With that said, Jared expressed being motivated to start physiotherapy. Jared hopes to improve his lower extremity strength and balance, in order to go on leisurely hikes with his parents. | During the initial assessment the patient was friendly yet appeared to be saddened and of low spirit. Jared has done an abundance of research on ALS and was very focused on the poor prognosis associated with the disease. The patient reports feeling defeated due to a lack of available treatments for ALS and feeling as if he was a burden to his mother. Additionally, the patient communicated feelings as if his dreams were taken away from him. He explained that he stopped playing soccer as a result of increased cramping and weakness in his legs, as well as having difficulty breathing while running on the field. Jared stated that he misses both the physical and social aspect of playing soccer. His parents have noticed changes in Jared’s voice, but reported that Jared’s friends and other family members haven’t noticed much change. Jared explained that his body image has been impacted since his diagnosis, as he has seen noticeable changes in his muscle mass. With that said, Jared expressed being motivated to start physiotherapy. Jared hopes to improve his lower extremity strength and balance, in order to go on leisurely hikes with his parents. | ||
=== History of Present Illness === | === History of Present Illness === | ||
One year ago, the patient noticed general weakness and cramping in his legs while playing soccer, which led to numerous falls on the field over several games. He spoke with his family doctor after two weeks of frequent falling and cramping. His family doctor referred him to a neurologist in Ottawa. Jared was diagnosed with ALS six months ago by his neurologist on November 10, | One year ago, the patient noticed general weakness and cramping in his legs while playing soccer, which led to numerous falls on the field over several games. He spoke with his family doctor after two weeks of frequent falling and cramping. His family doctor referred him to a neurologist in Ottawa. Jared was diagnosed with ALS six months ago by his neurologist on November 10, 2020. Treatment to date has been Riluzole medication prescribed by his doctor. | ||
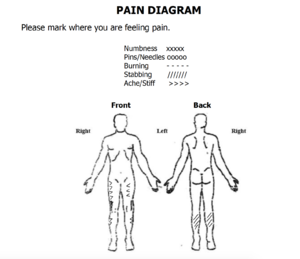
[[File:Screen Shot 2021-05-13 at 8.24.27 PM.png|alt=A pain diagram showing human body from the front and back. Achy pain represented by arrows on the front of both thighs and outside front of both calves. Stabbing/sharp pain, represented by oblique lines, located on back of calves. | [[File:Screen Shot 2021-05-13 at 8.24.27 PM.png|alt=A pain diagram showing human body from the front and back. Achy pain represented by arrows on the front of both thighs and outside front of both calves. Stabbing/sharp pain, represented by oblique lines, located on back of calves.|thumb|[https://www.lvhn.org/sites/default/files/uploads/PDFs/Advanced_Spine_Center_at_Neurosurgical_Associates/PMR_Pain_Diagram.pdf Figure 2]]] | ||
'''Pain:''' Site: calves, quads Radiation: not radiating Nature: deep cramping Periodicity: intermittent Duration: noticed it last 30 days Intensity: 4/10 Quality: sharp , cramping Aggravating factors: walking upstairs, running, walking distances >100 m Alleviating factors: massage, rest | '''Pain:''' Site: calves, quads Radiation: not radiating Nature: deep cramping Periodicity: intermittent Duration: noticed it last 30 days Intensity: 4/10 Quality: sharp , cramping Aggravating factors: walking upstairs, running, walking distances >100 m Alleviating factors: massage, rest | ||
=== Past medical history === | === Past medical history === | ||
| Line 42: | Line 43: | ||
=== Medications === | === Medications === | ||
Riluzole, 100mg orally/day ( | Riluzole, 100mg orally/day<ref>Miller RG, Mitchell JD, Moore DH. Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND). Cochrane Database of Syst Rev [Internet]. 2002 [cited 2021 May 9];(3). doi: 10.1002/14651858.CD001447</ref>, [https://www.webmd.com/drugs/2/drug-362/acetaminophen-oral/details Acetaminophen] as needed. | ||
=== Health Habits === | === Health Habits === | ||
| Line 58: | Line 59: | ||
=== Subjective outcome measures administered === | === Subjective outcome measures administered === | ||
* [https://www.pennstatehealth.org/sites/default/files/Neurology/ALSSQOL-%20Manual.pdf ALS-specific Quality of Life-Revised (ALSSQOL-R)]: a measure of QOL of individuals with ALS including aspects such as religiosity and intimacy. Jared’s ALSSQOL-R score= 7.2/10 ( | * [https://www.pennstatehealth.org/sites/default/files/Neurology/ALSSQOL-%20Manual.pdf ALS-specific Quality of Life-Revised (ALSSQOL-R)]: a measure of QOL of individuals with ALS including aspects such as religiosity and intimacy. Jared’s ALSSQOL-R score= 7.2/10<ref>Felgoise SH, Simmons Z, Brothers A, Stephens HE, Walsh SM. The ALS Specific Quality of Life-Revised (ALSSQOL-R) User’s Guide [Internet]. 2011 [cited 2021 May 11]. Available from: https://www.pennstatehealth.org/sites/default/files/Neurology/ALSSQOL-%20Manual.pdf</ref>. | ||
* [https://physio-pedia.com/Numeric_Pain_Rating_Scale?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Numeric Pain Rating Scale (NPRS):] a self-report measure regarding the patient’s pain experience, where the patient selects a whole number between 0-10 that best reflects their intensity of his/her pain over the last 24 hours. Jared indicates a pain score of 4 | * [https://physio-pedia.com/Numeric_Pain_Rating_Scale?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Numeric Pain Rating Scale (NPRS):] a self-report measure regarding the patient’s pain experience, where the patient selects a whole number between 0-10 that best reflects their intensity of his/her pain over the last 24 hours. Jared indicates a pain score of 4<ref>Numeric Pain Rating Scale [Internet]. Shirley Ryan AbilityLab. [cited 2021 May 11]. Available from: https://www.sralab.org/rehabilitation-measures/numeric-pain-rating-scale</ref>. | ||
=== '''Objective''' === | === '''Objective''' === | ||
| Line 78: | Line 79: | ||
* Sensation tested using a [https://physio-pedia.com/Dermatomes?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal dermatomal] pattern for the hot/cold and sharp/dull testing. No significant findings were found. | * Sensation tested using a [https://physio-pedia.com/Dermatomes?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal dermatomal] pattern for the hot/cold and sharp/dull testing. No significant findings were found. | ||
* To rule out combined cortical sensation impairments, testing including graphesthesia and stereognosis was completed. No significant findings were found. | * To rule out combined cortical sensation impairments, testing including graphesthesia and stereognosis was completed. No significant findings were found. | ||
* Tone was assessed using the [https://physio-pedia.com/Modified_Ashworth_Scale?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Modified Ashworth Spasticity Scale] | * Tone was assessed using the [https://physio-pedia.com/Modified_Ashworth_Scale?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Modified Ashworth Spasticity Scale] <ref>Ashworth Scale / Modified Ashworth Scale [Internet]. Chicago, IL: Shirley Ryan AbilityLab. [updated 2016 May 26, cited 2021May11]. Available from: https://www.sralab.org/rehabilitation-measures/ashworth-scale-modified-ashworth-scale</ref>. Findings include: | ||
** Increased tone in global muscles. | ** Increased tone in global muscles. | ||
** UE = 1+; LE = 1 | ** UE = 1+; LE = 1 | ||
| Line 84: | Line 85: | ||
==== Motor Control ==== | ==== Motor Control ==== | ||
* '''Global strength''' was measured using [https://physio-pedia.com/Category:Manual_Muscle_Testing?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal manual muscle testing (MMT)]. Findings include: | * '''Global strength''' was measured using [https://physio-pedia.com/Category:Manual_Muscle_Testing?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal manual muscle testing (MMT)]<ref>Cudkowicz M, Qureshi M, Shefner J. Measures and markers in amyotrophic lateral sclerosis. NeuroRx [Internet]. 2004 Apr 1 [Cited 2021 May 9];1(2):273-83. doi: 10.1602/neurorx.1.2.273</ref>. Findings include: | ||
** Bilateral ankle dorsiflexion = 3-/5 | ** Bilateral ankle dorsiflexion = 3-/5 | ||
** Wrist extension = 3+/5 | ** Wrist extension = 3+/5 | ||
| Line 91: | Line 92: | ||
** Knee extension = 3+/5 | ** Knee extension = 3+/5 | ||
* [https://physio-pedia.com/Grip_Strength?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Grip Strength] was measured using held dynamometer (HHD). Findings include: | * [https://physio-pedia.com/Grip_Strength?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal Grip Strength] was measured using held dynamometer (HHD)<ref name=":4" />. Findings include: | ||
** Lower than average grip strength | ** Lower than average grip strength | ||
** L = 30kg; R =35kg | ** L = 30kg; R =35kg | ||
| Line 98: | Line 99: | ||
** All AROM are WNL except: | ** All AROM are WNL except: | ||
*** Bilateral wrist extension = 50° | *** Bilateral wrist extension = 50° | ||
*** Bilateral finger extension (DIP, PIP, MCP) = MCP 30-45°; PIP, 0°; DIP, 20° | *** Bilateral finger extension (DIP, PIP, MCP) = MCP 30-45°; PIP, 0°; DIP, 20° | ||
*** Bilateral elbow extension = 10° | *** Bilateral elbow extension = 10° | ||
*** Bilateral dorsiflexion = 0° | *** Bilateral dorsiflexion = 0° | ||
| Line 106: | Line 107: | ||
** PROM all WNL | ** PROM all WNL | ||
* '''Manual dexterity''' was assessed using the [https://strokengine.ca/en/assessments/purdue-pegboard-test-ppt/ Purdue Pegboard Test (PPBT)]. ( | * '''Manual dexterity''' was assessed using the [https://strokengine.ca/en/assessments/purdue-pegboard-test-ppt/ Purdue Pegboard Test (PPBT)]<ref>Marvin K. Purdue Pegboard Test (PPT) [Internet]. Strokengine. [updated 2012 September 9, cited 2021May11]. Available from: https://strokengine.ca/en/assessments/purdue-pegboard-test-ppt/</ref><ref>Purdue Pegboard Test [Internet]. Lafayette, IN: Lafayette Instrument [updated 2021 March 3, cited 2021 May 9]. Available from: https://lafayetteevaluation.com/products/purdue-pegboard</ref>. | ||
** Jared’s overall dexterity was slowed bilaterally with his non-dominant (L) hand scoring slightly slower than his R hand. | ** Jared’s overall dexterity was slowed bilaterally with his non-dominant (L) hand scoring slightly slower than his R hand. | ||
*** Right hand: 9 | *** Right hand: 9 | ||
| Line 127: | Line 128: | ||
==== Balance ==== | ==== Balance ==== | ||
Balance was measured using the [https://www.sralab.org/rehabilitation-measures/mini-balance-evaluation-systems-test miniBESTest] for a baseline | Balance was measured using the [https://www.sralab.org/rehabilitation-measures/mini-balance-evaluation-systems-test miniBESTest] for a baseline<ref>Mini balance evaluation systems test [Internet]. Chicago, IL: Shirley Ryan AbilityLab; [updated 2013 June 4, cited 2021 May 11]. Available from: https://www.sralab.org/rehabilitation-measures/mini-balance-evaluation-systems-test</ref>. | ||
* Jared got a total score of 17/28. | * Jared got a total score of 17/28. | ||
| Line 152: | Line 153: | ||
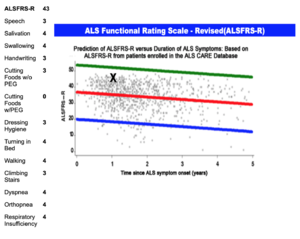
==== ALS Functional rating scale - Revised (ALSFRS-R) ==== | ==== ALS Functional rating scale - Revised (ALSFRS-R) ==== | ||
[https://www.outcomes-umassmed.org/als/alsscale.aspx ALSFRS-R] is a test used to measure the functional status of individuals with ALS. The ALSFRS-R is scored using 12 activities of daily living measured using a 5-point scale. The highest score for each item is 4 which represents normal function. The lowest score for each item is 0 which represents loss of the function being assessed. The total score for the scale is 48, with a higher score indicating a higher functioning individual. | [https://www.outcomes-umassmed.org/als/alsscale.aspx ALSFRS-R] is a test used to measure the functional status of individuals with ALS. The ALSFRS-R is scored using 12 activities of daily living measured using a 5-point scale. The highest score for each item is 4 which represents normal function. The lowest score for each item is 0 which represents loss of the function being assessed. The total score for the scale is 48, with a higher score indicating a higher functioning individual<ref>Outcome measures [Internet]. Utrecht, the Netherlands: ENCALS; [cited 202 1May 11]. Available from: https://www.encals.eu/outcome-measures/</ref><ref>The ALS C.A.R.E. Program. Interpretation guides to standardized questionnaires employed in the ALS CARE database [Internet]. Worcester, MA: University of Massachusetts Medical School; [cited 2021 May 11]. Available from: https://www.outcomes-umassmed.org/als/sf12.aspx</ref>. | ||
[[File:Jared's ALSFRS-R Score.png|thumb|Figure 4. Jared's ALSFRS-R score during his first physiotherapy appointment (01/04/2021). The left column depicts Jared's score in each category. The right graph depicts the data compared to Jared (seen as the X).|alt=|center]] | [[File:Jared's ALSFRS-R Score.png|thumb|Figure 4. Jared's ALSFRS-R score during his first physiotherapy appointment (01/04/2021). The left column depicts Jared's score in each category. The right graph depicts the data compared to Jared (seen as the X).|alt=|center]] | ||
==== Ventilatory Muscle Strength ==== | ==== Ventilatory Muscle Strength ==== | ||
* Maximal Inspiratory Pressure (MIP) = -102 cmH20 and Maximal Expiratory Pressure (MEP) = 143 cmH2O | * Maximal Inspiratory Pressure (MIP) = -102 cmH20 and Maximal Expiratory Pressure (MEP) = 143 cmH2O. | ||
==== BMI ==== | ==== BMI ==== | ||
* 6 foot 1 in, 158 pounds:[https://physio-pedia.com/index.php?title=File%3A690px-Body_mass_index_chart.svg.png&veaction=edit§ion=1?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal BMI] of 21 (healthy/normal weight) | * 6 foot 1 in, 158 pounds:[https://physio-pedia.com/index.php?title=File%3A690px-Body_mass_index_chart.svg.png&veaction=edit§ion=1?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal BMI] of 21 (healthy/normal weight). | ||
== Clinical Impression == | == Clinical Impression == | ||
=== Physiotherapy Diagnosis === | === Physiotherapy Diagnosis === | ||
Jared is a 24-year-old male who presents to physiotherapy following a neurologist diagnosis of early-stage Amyotrophic Lateral Sclerosis (ALS) 6 months ago | Jared is a 24-year-old male who presents to physiotherapy following a neurologist diagnosis of early-stage Amyotrophic Lateral Sclerosis (ALS) 6 months ago<ref>Dal Bello-Haas V, Kloos AD, Mitsumoto H. Physical therapy for a patient through six stages of amyotrophic lateral sclerosis. Physical Therapy [Internet]. 1998, December 1 [Cited 2021 May 11]; 78(12), pp.1312-1324. doi: 10.1093/ptj/78.12.1312</ref>. Jared and his parents indicated that he is currently independent in all his ADLs; however, he is having difficulties with certain ADLs requiring greater hand and finger dexterity, such as brushing his teeth. Jared has recently stopped playing recreational soccer as he was experiencing an increase in falls, difficulties with his balance, increased cramping, and weakness in his legs. Jared’s decreased grip strength and impaired hand and finger dexterity led him to take a leave from work, and they are currently preventing him from applying to dentistry school. Jared has a good social support system at home as he is living with his sister and parents. He expressed being motivated to start physiotherapy to continue leisurely hiking with his family and returning to work at the grocery store. Therefore, Jared would benefit from physiotherapy treatment focusing on maintaining his functional independence and muscle strength. Treatment should also include education on lifestyle modification and energy conservation strategies related to ALS. | ||
=== Problem List (According to the [https://physio-pedia.com/International_Classification_of_Functioning,_Disability_and_Health_(ICF)?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal ICF Framework]) === | === Problem List (According to the [https://physio-pedia.com/International_Classification_of_Functioning,_Disability_and_Health_(ICF)?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal ICF Framework]) === | ||
| Line 175: | Line 176: | ||
* Mild muscle weakness globally, with upper and lower limb atrophy most notably in: Bilateral ankle dorsiflexion = 3-/5, Wrist extension = 3+/5, Hip flexion = 3+/5, Hip extension 3+/5, Knee extension = 3+/5. | * Mild muscle weakness globally, with upper and lower limb atrophy most notably in: Bilateral ankle dorsiflexion = 3-/5, Wrist extension = 3+/5, Hip flexion = 3+/5, Hip extension 3+/5, Knee extension = 3+/5. | ||
* Potentially experiencing body dysmorphia since his diagnosis, as he has seen noticeable changes in his muscle mass. | * Potentially experiencing body dysmorphia since his diagnosis, as he has seen noticeable changes in his muscle mass. | ||
* Demonstrated LMN hyperreflexia for upper and lower limb (Achilles 4+, patellar, triceps, biceps 3+) | * Demonstrated LMN hyperreflexia for upper and lower limb (Achilles 4+, patellar, triceps, biceps 3+). | ||
* Demonstrated UMN hyperreflexia (Babinski and clonus) | * Demonstrated UMN hyperreflexia (Babinski and clonus). | ||
* At risk of respiratory compromise with further neurodegeneration | * At risk of respiratory compromise with further neurodegeneration. | ||
| Line 185: | Line 186: | ||
* Decreased dynamic and anticipatory balance and increased risk of falls according to miniBEST balance testing. | * Decreased dynamic and anticipatory balance and increased risk of falls according to miniBEST balance testing. | ||
* ALSFRS-R score = 43/48. | * ALSFRS-R score = 43/48. | ||
* Decreased manual dexterity as shown in Purdue pegboard test | * Decreased manual dexterity as shown in Purdue pegboard test. | ||
* Drop foot gait patterning. | * Drop foot gait patterning. | ||
| Line 197: | Line 198: | ||
* Unable to study to become a dentist due to decreased upper limb strength and hand and finger dexterity which hinders practical ability to study dentistry. | * Unable to study to become a dentist due to decreased upper limb strength and hand and finger dexterity which hinders practical ability to study dentistry. | ||
=== Intervention === | === Intervention<ref>American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. Lippincott Williams & Wilkins; 2013 Mar 4</ref><ref>Dal Bello-Haas VD. Physical therapy for individuals with amyotrophic lateral sclerosis: current insights. Degenerative neurological and neuromuscular disease. 2018;8:45–54</ref> === | ||
{| class="wikitable" | {| class="wikitable" | ||
|+ | |+ | ||
| Line 302: | Line 303: | ||
== Outcome == | == Outcome == | ||
Jared was very motivated to follow the intervention and plans set out from his physiotherapy sessions. He understood the importance of physical activity and strengthening to maintain/delay the progression of ALS. After ''the 1st week'', Jared mentioned that he enjoyed the strength training and found the stretches, massages, and ischemic compressions to be helpful with his cramps and fatigue. He especially liked the hand-specific exercises, as he found himself more confident with his fine motor control skills (Ex., using his phone and laptop). He mentioned that his pain has become more tolerable and has only reached a maximum of 3/10 when using the NPRS compared to his previous score of 4/10 before physiotherapy sessions (in both calves and quads). Although Jared was doing well with all of his exercises, we did not believe that increasing the resistance/intensity of his exercises would benefit him. Increasing the intensity of the exercises may negatively affect his prognosis, and therefore we were cautious with progressing Jared’s interventions | Jared was very motivated to follow the intervention and plans set out from his physiotherapy sessions. He understood the importance of physical activity and strengthening to maintain/delay the progression of ALS. After ''the 1st week'', Jared mentioned that he enjoyed the strength training and found the stretches, massages, and ischemic compressions to be helpful with his cramps and fatigue. He especially liked the hand-specific exercises, as he found himself more confident with his fine motor control skills (Ex., using his phone and laptop). He mentioned that his pain has become more tolerable and has only reached a maximum of 3/10 when using the NPRS compared to his previous score of 4/10 before physiotherapy sessions (in both calves and quads). Although Jared was doing well with all of his exercises, we did not believe that increasing the resistance/intensity of his exercises would benefit him. Increasing the intensity of the exercises may negatively affect his prognosis, and therefore we were cautious with progressing Jared’s interventions<ref>O'Sullivan SB, Schmitz TJ, Fulk GD, O'Sullivan SB. Amyotrophic Lateral Sclerosis. In: Physical rehabilitation. 7th ed. Philadelphia: F.A. Davis; 2019. p. 739–40</ref>. | ||
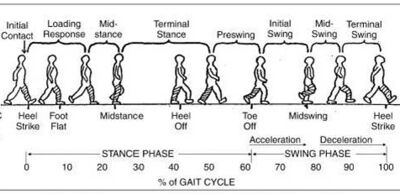
''After three weeks of therapy'', Jared’s global strength was reassessed through MMT and grip strength through the use of a dynamometer. His gait and balance were also reassessed. Overall, his strength was very similar to his initial assessment except for an increase in dorsiflexion strength to 3/5 bilaterally, wrist extensors to 4-/5 bilaterally, and knee extension strength to 4-/5 bilaterally. His grip strength slightly improved to 33kg on his L and 37kg on his R hand, but it is not clinically significant (4). His gait slightly improved, as Jared displayed better foot clearance and increased dorsiflexion during the swing phase bilaterally. Finally, Jared’s balance was re-assessed using the miniBESTest. He scored an 18/28 (Anticipatory: 4/6, Reactive Postural Control: 4/6, Sensory Orientation: 4/6, Dynamic Gait: 6/10). Jared's change in score does not represent a clinically significant difference; however, there were not any decreases in his balance skills. At this point, Jared felt slightly discouraged as there were no grand overall improvements. However, we had to re-emphasize the importance of maintaining his current physical performance, educating Jared on ALS and its prognosis, and the value of preventing the effects of ALS. | ''After three weeks of therapy'', Jared’s global strength was reassessed through MMT and grip strength through the use of a dynamometer. His gait and balance were also reassessed. Overall, his strength was very similar to his initial assessment except for an increase in dorsiflexion strength to 3/5 bilaterally, wrist extensors to 4-/5 bilaterally, and knee extension strength to 4-/5 bilaterally. His grip strength slightly improved to 33kg on his L and 37kg on his R hand, but it is not clinically significant (4). His gait slightly improved, as Jared displayed better foot clearance and increased dorsiflexion during the swing phase bilaterally. Finally, Jared’s balance was re-assessed using the miniBESTest. He scored an 18/28 (Anticipatory: 4/6, Reactive Postural Control: 4/6, Sensory Orientation: 4/6, Dynamic Gait: 6/10). Jared's change in score does not represent a clinically significant difference; however, there were not any decreases in his balance skills. At this point, Jared felt slightly discouraged as there were no grand overall improvements. However, we had to re-emphasize the importance of maintaining his current physical performance, educating Jared on ALS and its prognosis, and the value of preventing the effects of ALS. | ||
| Line 311: | Line 312: | ||
== Discussion == | == Discussion == | ||
ALS is a progressive neurodegenerative disease associated with the degeneration of upper and lower motor neurons, and results in a vast presentation of symptoms relating to motor control. | ALS is a progressive neurodegenerative disease associated with the degeneration of upper and lower motor neurons, and results in a vast presentation of symptoms relating to motor control<ref name=":0" />. In addition to the impact on the motor neurons, ALS has devastating implications for one’s overall wellbeing, often leading to depression and feelings of hopelessness. Although there is no cure for ALS, multidisciplinary management is important for optimizing functional independence and QOL. This can be done through maintaining strength, mobility, lifestyle modifications, energy preservation strategies, and preparation for end of life<ref>Soriani MH, Desnuelle C. Care management in amyotrophic lateral sclerosis. Revue neurologique. 2017 May 1 [cited 2021 May 10];173(5):288-99. doi: 0.1016/j.neurol.2017.03.031 </ref>. | ||
This fictional case study was developed to illustrate the progressive nature of ALS through a physiotherapy subjective and objective assessment and to demonstrate a potential physiotherapy management plan. Jared is a 24-year-old soccer player who presents with juvenile ALS. After completing a physiotherapy assessment, it was found that Jared has mild muscular atrophy in his hands, quadriceps, and calves, increased muscle tone in both the upper and lower extremities, a moderate overall decrease in strength, decreased ROM in his distal extremities, and modest changes in gait. As a young athlete and aspiring dentist, Jared expresses feeling discouraged regarding the progressive nature of this condition. However, with encouragement from his support system, Jared feels motivated to attend physiotherapy to improve his overall strength and balance, and hopes return to work and leisurely hiking with his family. | This fictional case study was developed to illustrate the progressive nature of ALS through a physiotherapy subjective and objective assessment and to demonstrate a potential physiotherapy management plan. Jared is a 24-year-old soccer player who presents with juvenile ALS. After completing a physiotherapy assessment, it was found that Jared has mild muscular atrophy in his hands, quadriceps, and calves, increased muscle tone in both the upper and lower extremities, a moderate overall decrease in strength, decreased ROM in his distal extremities, and modest changes in gait. As a young athlete and aspiring dentist, Jared expresses feeling discouraged regarding the progressive nature of this condition. However, with encouragement from his support system, Jared feels motivated to attend physiotherapy to improve his overall strength and balance, and hopes return to work and leisurely hiking with his family. | ||
The discussion of whether individuals with progressive degenerative diseases—such as ALS—should exercise has been a controversial topic. Previous literature has been inconclusive regarding the benefits of exercise in ALS; it was traditionally thought that exercise may enhance deterioration ( | The discussion of whether individuals with progressive degenerative diseases—such as ALS—should exercise has been a controversial topic. Previous literature has been inconclusive regarding the benefits of exercise in ALS; it was traditionally thought that exercise may enhance deterioration<ref name=":5">Meng L, Li X, Li C, Tsang RCC, Chen Y, Ge Y, Gao Q. Effects of exercise in patients with amyotrophic lateral sclerosis. American Journal of Physical Medicine & Rehabilitation [Internet]. 2020, September [cited 2021 May 09]; 99(9): 801-810. doi: 10.1097/PHM.0000000000001419 </ref>. However, recent literature has demonstrated the potential of exercise to delay the progression of the condition, and thus, improve functional ability<ref name=":5" />. Meng et al.<ref name=":5" /> found that the benefits of exercise were better demonstrated in the long-term, which is likely observed in patients who have a slower disease course. Majmudar et al.<ref name=":3" /> suggest that moderate exercise is safe for those with ALS, however, the delivery of these guidelines requires specific attention to the status of the patient. | ||
Jared’s management plan focuses on strengthening and endurance exercises for the upper and lower extremities, as well balance training, with the goal being to maintain or recover strength and balance required for functional independence. Endurance exercises include ambulation on a treadmill, and balance exercises include exercises such as single leg stance. In addition, the multidisciplinary team provided Jared with the necessary education and tools for optimizing his function and QOL. This education included information on juvenile ALS, pain science, energy conservation, gait aids, and lifestyle modifications. Jared was referred to an | Jared’s management plan focuses on strengthening and endurance exercises for the upper and lower extremities, as well balance training, with the goal being to maintain or recover strength and balance required for functional independence. Endurance exercises include ambulation on a treadmill, and balance exercises include exercises such as single leg stance. In addition, the multidisciplinary team provided Jared with the necessary education and tools for optimizing his function and QOL. This education included information on juvenile ALS, pain science, energy conservation, gait aids, and lifestyle modifications. Jared was referred to an occupational therapist for assistance with performing ADLs, and a registered dietitian for guidance on obtaining optimal nutrition throughout his degenerative condition. Various outcome measures were used to assess his strength and balance; after 6 weeks of physiotherapy, Jared’s strength and balance were both maintained. Due to the rapid and unpredictable nature of ALS, the maintenance of his current status is a positive finding and has optimistic implications on his functioning and QOL. | ||
Jared’s case provides a framework for management of patients with ALS who are diagnosed at a young age. The onset of ALS most commonly occurs between the ages of 50 and 75, and therefore, research has focused on ALS as a disease that impacts those later in life. However, it is important for members of the interdisciplinary team to not only be aware of juvenile ALS, but also be able to alter their treatment to target the goals of this younger population. Age is a strong predictor for prognosis, indicating that the older the age of diagnosis, the worse the outcome ( | Jared’s case provides a framework for management of patients with ALS who are diagnosed at a young age. The onset of ALS most commonly occurs between the ages of 50 and 75, and therefore, research has focused on ALS as a disease that impacts those later in life. However, it is important for members of the interdisciplinary team to not only be aware of juvenile ALS, but also be able to alter their treatment to target the goals of this younger population. Age is a strong predictor for prognosis, indicating that the older the age of diagnosis, the worse the outcome<ref>Chiò A, Logroscino G, Hardiman O, Swingler R, Mitchell D, Beghi E, Traynor BG, Consortium E. Prognostic factors in ALS: A critical review. Amyotroph Lateral Scler [Internet]. 2009, October [cited 2021 May 11]; 99(5-6): 310–323. doi: 0.3109/17482960802566824</ref>. In this fictional case study, Jared was diagnosed with ALS at the age of 24, which is much younger than the typical age of onset. For this reason, it is predicted that Jared will have a slower advancement of symptoms; this was demonstrated throughout the case study. Furthermore, this case study was used to illustrate the variability of ALS symptoms and progression of disease. Despite having the same diagnosis, each patient will have a unique experience of symptoms, needs, and goals. Thus, it is imperative that health care professionals incorporate the patient into their management plan, and tailor their treatment specifically to each patient. | ||
== Interdisciplinary Management of ALS == | == Interdisciplinary Management of ALS == | ||
[[File:ALS multidisciplinary team.jpg|alt=Diagram showing all of the health care professions involved in the management of ALS|thumb|250x250px|[https://www.ajmc.com/view/als-managed-care-considerations Figure 5] All members involved in management of ]] | [[File:ALS multidisciplinary team.jpg|alt=Diagram showing all of the health care professions involved in the management of ALS|thumb|250x250px|[https://www.ajmc.com/view/als-managed-care-considerations Figure 5] All members involved in management of ]]Patient-centred, interdisciplinary, and comprehensive rehabilitation is vital for individuals with ALS and has been shown to significantly improve their care and QOL<ref>Paganoni S, Karam C, Joyce N, Bedlack R, Carter GT. Comprehensive rehabilitative care across the spectrum of amyotrophic lateral sclerosis. NeuroRehabilitation. 2015 Jan 1 [cited 2021 May 8];37(1):53-68. doi: 10.3233/NRE-151240</ref>. Health care professionals who may be involved in the care of individuals with ALS include the patient’s family and friends, family physician, neurologist, physiotherapists, occupational therapists (OTs), registered dieticians, speech language therapists, social workers and palliative care. | ||
Patient-centred, interdisciplinary, comprehensive rehabilitation | |||
=== Occupational Therapist === | === Occupational Therapist === | ||
OTs play an integral role in the interdisciplinary care of individuals with ALS. There are many tasks that an OT can perform to help ALS patients maintain | OTs play an integral role in the interdisciplinary care of individuals with ALS. There are many tasks that an OT can perform to help ALS patients maintain maximum functional independence. They can also play a role in altering the patient’s attitude and perspective, to shift towards focussing on tasks that they can perform, rather than those they can’t. Although Jared is currently independent in his ADLs, he is experiencing increasing difficulty with ADLs requiring hand motor dexterity. Therefore, an OT can play a role in fitting and prescribing Jared with upper extremity bracing or adaptive devices. For example, adaptive large grip utensils may be recommended to allow individuals with ALS to maintain independence while eating or a resting hand splint may be recommended to prevent wrist and finger flexion contractures<ref name=":3" />. Jared is currently able to ambulate independently, however, as his disease progresses, he will likely require the use of an Ankle-Foot Orthosis (AFO) or a gait aid. Gait aids may include a cane, walker and eventually a wheelchair<ref name=":3" />. An OT will play a major role in fitting and prescribing an AFO and/or a gait aid to Jared. | ||
Additionally, an OT | Additionally, an OT plays a role in educating individuals with ALS and their families on energy conservation and fatigue management. For example, OTs can provide education on the benefits of breaking up high-energy tasks by incorporating rest breaks into their daily activities and planning their day to prioritize the tasks that are most important to them. This type of education has shown to be effective in reducing fatigue, managing fatigue symptoms and improving different aspects such as health-related quality of life<ref>De-Bernardi-Ojuel L, Torres-Collado L, García-de-la-Hera M. Occupational therapy interventions in adults with multiple sclerosis or amyotrophic lateral sclerosis: a scoping review. International Journal of Environmental Research and Public Health [Internet]. 2021 Feb 3 [cited 2021 May 9];18(4):1432. doi: 10.3390/ijerph18041432</ref>. | ||
Finally, | Finally, during the later stages of ALS, the OT may conduct a home assessment and provide recommendations to the family on certain modifications that they may want to make to enhance the individual’s mobility and safety. For example, a ramp may be recommended to enter the home, or a stair lift if the individual with ALS lives in a multi-story home like Jared. In addition, the OT will likely give instructions to the family members and caregivers on how they can assist and support their family member with ALS with their exercises, proper positioning, how to lift and transfer the individual and how to use the assistive devices<ref>MDA-ALS Center. Occupational and physical therapy [Internet]. Pittsburgh, PA 15213: University of Pittsburgh; [updated 2021 May 3, cited 2021 May 11]. Available from: https://www.alsclinic.pitt.edu/patient-issues/occupational-and-physical-therapy</ref>. Therefore, it is evident that OTs play an essential role in the interdisciplinary care team for patients with ALS as they can assist in a multitude of ways throughout the disease progression. | ||
=== Registered Dietician === | === Registered Dietician === | ||
A second key member of the interdisciplinary care team | A second key member of the interdisciplinary care team for patients with ALS are registered dieticians (RD). RDs can provide a variety of different treatment options for ALS depending on the physical and nutritional status of the individual. As previously indicated, muscle weakness is a common symptom with ALS. This weakness can affect eating and swallowing, thus RDs can help individuals with ALS to optimize their diet, maintain or improve their nutritional status, minimize weight loss and maintain fluid intake. | ||
In our case study, Jared is recently diagnosed with juvenile ALS and still has a high level of function. He is experiencing some muscle weakness; however, he does not currently have any difficulties with swallowing. Therefore, the role of the RD may be centred around assisting Jared to optimize his diet and maintain or improve his nutritional status. This may be through evidence-based nutritional guidance in the form of nutritional monitoring, meal planning, and an individualized diet targeted for optimal nutrition. Throughout this process, the RD would focus on areas such as caloric and hydration requirements, macronutrient and micronutrient requirements, and supplementation to optimize Jared’s QOL. This is important for Jared as his score on the ALSSQOL-R is 7.2/10, which indicates that there are areas that need to be addressed in order to improve his QOL. | |||
Additionally, as Jared is still walking and wants to get back to hiking with his family, a RD could help him to monitor or improve his nutritional status to maintain his energy levels for these activities. By monitoring his nutritional status, Jared and the RD will be able to identify and address any potential risks for malnutrition<ref name=":6">Rio A, Cawadias E. Nutritional advice and treatment by dietitians to patients with amyotrophic lateral sclerosis/motor neurone disease: a survey of current practice in England, Wales, Northern Ireland and Canada. Journal of human nutrition and dietetics. 2007 Feb [cited 2021 May 11];20(1):3-13. doi: 10.1111/j.1365-277X.2007.00745.x</ref>. | |||
Moreover, individuals with ALS are at an increased risk of weight loss due to several factors, including malnutrition, difficulties swallowing, potential increased caloric expenditure from muscular fasciculations and decreased caloric intake due to comorbid mental illnesses<ref>Körner S, Hendricks M, Kollewe K, Zapf A, Dengler R, Silani V, Petri S. Weight loss, dysphagia and supplement intake in patients with amyotrophic lateral sclerosis (ALS): impact on quality of life and therapeutic options. BMC neurology. 2013 Dec [cited 2021 May 7];13(1):1-9. doi: 10.1186/1471-2377-13-84</ref>. Jared currently has a healthy BMI of 21, however, has noticed a decrease in muscle mass. An increased BMI is associated with more favourable outcomes in individuals with ALS<ref name=":7">Ning P, Yang B, Li S, Mu X, Shen Q, Hu F, Tang Y, Yang X, Xu Y. Systematic review of the prognostic role of body mass index in amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. 2019 Jul 3 [cited 2021 May 10];20(5-6):356-67. doi: 10.1080/21678421.2019.1587631</ref>. Therefore, an RD can assist Jared with minimizing weight loss and maintaining his BMI<ref name=":7" />. | |||
Finally, as the disease progresses, 85% of individuals with ALS will experience difficulties swallowing, also known as dysphagia<ref>Onesti E, Schettino I, Gori MC, Frasca V, Ceccanti M, Cambieri C, Ruoppolo G, Inghilleri M. Dysphagia in amyotrophic lateral sclerosis: impact on patient behavior, diet adaptation, and riluzole management. Frontiers in Neurology [Internet]. 2017 Mar 21 [Cited 2021 May 13]; 8:94. doi: 10.3389/fneur.2017.00094</ref>. Therefore, the role of the RD will transition to having a large focus on assessing the severity of dysphagia and providing nutritional management<ref name=":8">College of Dieticians of Ontario. Scope of practice and controlled acts [Internet]. Toronto, ON: College of Dietitians of Ontario [cited 2021 May 10]. Available from: https://www.collegeofdietitians.org/programs/practice-advisory-program/professional-practice-resources/scope-of-practice.aspx#:~:text=The%20Dietetic%20Scope%20of%20Practice,related%20disorders%20by%20nutritional%20means.%E2%80%9D</ref>. The purpose of the assessment of dysphagia is to identify the risk of aspiration, developing pneumonia, and choking, and whether oral or non-oral routes of hydration and nutrition are indicated<ref name=":8" />. In these cases, RDs assess the individual’s need for alternative methods to oral feeding such as a percutaneous endoscopic gastrostomy in which a feeding tube bypasses the esophagus and is inserted through the abdominal wall into the stomach for enteral nutrition<ref name=":6" />. This alternative to oral feeding helps to improve or maintain nutritional status when more severe dysphagia is present in the advanced stages of ALS. Maintaining nutritional status is critical to prevent weight loss and fatigue. Although Jared is still in the early stages of the condition, both Jared and his family should work together with an RD in the future to discuss potential options. | |||
In summation, RDs are an essential part of the interdisciplinary healthcare team for individuals with ALS and should be incorporated to help manage nutrition in both the early and more advanced stages of the condition. | |||
== Self-study questions == | == Self-study questions == | ||
Latest revision as of 20:34, 14 May 2021
Top Contributors - Darcy Chassé, Daniel Habashi, Kara Blair, Halle Pawson, Nicholas Mutton, Katie Milliere and Kim Jackson
Abstract[edit | edit source]
Amyotrophic Lateral Sclerosis (ALS) is a rare neurological disease that involves the degeneration of neurons responsible for controlling voluntary muscle movement[1]. Ultimately, most people with ALS die within 3-5 years after symptom onset due to respiratory failure[1]. This fictional case study involves a 24-year-old male diagnosed with early-stage juvenile ALS 6 months prior. This case study documents the subjective and objective findings from the patient’s initial physiotherapy assessment, and additional findings 6-weeks after beginning physiotherapy treatment. Moreover, potential physiotherapy interventions are outlined, with the goal being to maintain the patient’s strength, balance, and overall functional independence despite having a progressive degenerative disease. Furthermore, this case study highlights the importance of a multidisciplinary team approach to managing progressive degenerative diseases such as ALS. Together, the interdisciplinary team can address the wide range of signs and symptoms, the various biopsychosocial implications, and finally, work towards achieving patient specific goals.
Introduction[edit | edit source]
Amyotrophic lateral sclerosis (ALS) is a progressive neuromuscular disease that involves the neurons responsible for controlling voluntary muscle movement[1]. ALS most commonly appears between the ages of 55 to 75 but can impact individuals within any age group[1]. In ALS, both the upper motor neurons and lower motor neurons degenerate, and therefore, stop sending signals to the muscles[1]. This interruption in signalling results in weakening of the muscles, twitching—known as fasciculations—and muscle wasting. The early symptoms usually involve muscle weakness and eventually progress to the inability to speak, eat, move, or breathe[1]. Respiratory failure is the dominant cause of death in individuals with ALS and usually occurs within 3 to 5 years from the onset of symptoms[1]. Approximately 70% of patients with ALS present with limb-onset ALS—weakness in the arms and legs—and the remaining patients present with bulbar-onset ALS, which manifests with dysarthria—motor speech disorder—and dysphagia—difficulty swallowing[3].
The clinical presentation of ALS is not homogenous. There is considerable variability in the phenotypical expression of ALS, as shown throughout the literature. Jamorzik et al.[3] discuss a 68-year-old man who first presented with dysarthria in July 2012, and began experiencing generalized fasciculations several months later. A year later, the patient’s speech became more slurred, but he did not present with muscular atrophy or weakness. Clinical evaluations supported by electrophysiological and biochemical testing led to the diagnosis of bulbar-onset ALS[3]. Conversely, Venizelos, Park & Fisher[4] presented a case of a 57-year-old Caucasian male who began experiencing unexplained bilateral lower extremity weakness and fasciculations. Within five months, his lower extremity weakness progressed until he was unable to stand independently. He also presented with muscular atrophy in the upper extremities, specifically in the intrinsic hand muscles. Despite being diagnosed with multiple other diseases, including chronic inflammatory demyelinated polyneuropathy (CIDP), the patient was later diagnosed with ALS and died one year after symptom onset[3]. In an additional study, Majmudar, Wu, and Paganoni[5] discussed a case involving a 45-year-old female patient who presented with an early stage of ALS. This patient first began experiencing right leg and arm weakness, fatigue and suffered from several falls while playing with her kids. Additionally, she expressed having difficulty with activities involving fine motor control, such as cutting food and doing up buttons on clothing[5].
There is currently no cure for ALS, however, riluzole is a medication that is moderately effective at prolonging life for individuals with ALS by two to three months[4]. Moreover, physiotherapy in conjunction with other forms of healthcare has shown to be beneficial for symptom management, optimizing functional independence, and increasing quality of life in those with ALS. Management for ALS should be tailored to the individual to meet their individual needs and goals[5]. Majmudar et al.[5] suggested that exercise, energy conservation techniques, stretching, and range of motion (ROM), as well as assistive devices for gait, may be appropriate for early-stage ALS. However, the individual should be monitored for signs of overexertion, excessive fatigue, and an increase in pain[5]. Tsitkanou et al.[6] demonstrated that both endurance and resistance training have a beneficial impact on quality of life; however, they do not extend life expectancy.
The purpose of this report is to create a realistic picture of a young individual diagnosed with early-stage ALS. A fictional case study will be used to illustrate the progressive nature of the disease, outline the process of a physiotherapy assessment and identify the likely findings for patients with ALS. Physiotherapy interventions for ALS, supported by the work of other healthcare professionals, focus on maximizing patients’ mobility, respiratory function, independence, and quality of life[5]. Therefore, this report will also outline various physiotherapy interventions that assist in improving quality of life in patients with ALS. This case study was developed by integrating evidence-based research and clinical findings to educate other healthcare professionals on ALS and inform clinical decision-making.
When taking on this project, we were aware that ALS is a very challenging condition, and much research is needed to fully understand the cause of the disease and develop a cure. However, an additional challenge we faced was developing a physiotherapy treatment plan that targeted the multitude of impairments experienced by those with ALS. This progressive disease can lead to impairments in balance, gait, dexterity, strength, and so on. Therefore, the requirement for a treatment plan to tackle the immense number of symptoms, as well as work to achieve patient specific goals, adds to the complexity of the disorder.
Client Characteristics[edit | edit source]
A 24-year-old, R-hand dominant, Caucasian male, named Jared Miller. Jared lives with his parents—Jane and James Miller—and his sister Jaya in Perth, Ontario. Jared was previously an athlete on his high school soccer team. After completing his undergraduate degree in Kinesiology at Queen's University, Jared hoped to obtain a doctorate in Dentistry. However, Jared unable able to pursue this career aspiration after being diagnosed with ALS 6-months ago. He first noticed changes in muscle strength after falling several times on the soccer field, and he has expressed a general feeling of weakness. Since the onset of these initial symptoms, Jared has been experiencing ongoing muscle weakness, cramping, and associated pain. Moreover, Jared was referred to physiotherapy by a neurologist. Despite having been diagnosed with ALS, Jared has no comorbid conditions[7].
Examination Findings[edit | edit source]
Subjective[edit | edit source]
Chief Concern[edit | edit source]
Feeling of general weakness, muscle cramping, and 4/10 pain in arms and legs. Additionally, Jared is concerned with his recent falls as it is limiting participation in work, hiking, and navigating his environment.
Patient Profile[edit | edit source]
24-year-old male with ALS. DOB: 1996/06/02
During the initial assessment the patient was friendly yet appeared to be saddened and of low spirit. Jared has done an abundance of research on ALS and was very focused on the poor prognosis associated with the disease. The patient reports feeling defeated due to a lack of available treatments for ALS and feeling as if he was a burden to his mother. Additionally, the patient communicated feelings as if his dreams were taken away from him. He explained that he stopped playing soccer as a result of increased cramping and weakness in his legs, as well as having difficulty breathing while running on the field. Jared stated that he misses both the physical and social aspect of playing soccer. His parents have noticed changes in Jared’s voice, but reported that Jared’s friends and other family members haven’t noticed much change. Jared explained that his body image has been impacted since his diagnosis, as he has seen noticeable changes in his muscle mass. With that said, Jared expressed being motivated to start physiotherapy. Jared hopes to improve his lower extremity strength and balance, in order to go on leisurely hikes with his parents.
History of Present Illness[edit | edit source]
One year ago, the patient noticed general weakness and cramping in his legs while playing soccer, which led to numerous falls on the field over several games. He spoke with his family doctor after two weeks of frequent falling and cramping. His family doctor referred him to a neurologist in Ottawa. Jared was diagnosed with ALS six months ago by his neurologist on November 10, 2020. Treatment to date has been Riluzole medication prescribed by his doctor.
Pain: Site: calves, quads Radiation: not radiating Nature: deep cramping Periodicity: intermittent Duration: noticed it last 30 days Intensity: 4/10 Quality: sharp , cramping Aggravating factors: walking upstairs, running, walking distances >100 m Alleviating factors: massage, rest
Past medical history[edit | edit source]
No significant past medical history. Patient had tonsillectomy at age 10.
Medications[edit | edit source]
Riluzole, 100mg orally/day[8], Acetaminophen as needed.
Health Habits[edit | edit source]
Patient does not smoke cigarettes, drink alcohol, or do recreational drugs.
Family history[edit | edit source]
No known family history of ALS. Patient’s father has asthma. Mother has Type II diabetes.
Social history[edit | edit source]
Lives in a 3-storey home, with mom, dad, and younger sister. He enjoys playing and watching sports and hiking with his family. Patient meets up with friends every weekend to watch the soccer game. The patient used to work at the Independent Grocer in the grocery department performing tasks such as stocking shelves and unloading skids. He left this job 3 months ago on medical leave, as it was challenging for him to lift heavy objects and have the dexterity and control to place small objects onto the shelves.
Current functional status[edit | edit source]
The patient reports difficulty performing common activities of daily living (ADLs), including washing dishes, cutting food, shaving, and brushing his teeth. Jared explains that he has challenges walking long distances and running due to muscle cramping and balance difficulties. However, he does not use any mobility aids to assist him. Additionally, he describes that his handwriting is impaired. Jared explains that he experienced shortness of breath during exercise, however, since his diagnosis, he has not recognized any additional breathing challenges at rest. The patient reports experiencing no changes in bowel or bladder functioning, difficulty with swallowing, and changes in cognitive function.
Subjective outcome measures administered[edit | edit source]
- ALS-specific Quality of Life-Revised (ALSSQOL-R): a measure of QOL of individuals with ALS including aspects such as religiosity and intimacy. Jared’s ALSSQOL-R score= 7.2/10[9].
- Numeric Pain Rating Scale (NPRS): a self-report measure regarding the patient’s pain experience, where the patient selects a whole number between 0-10 that best reflects their intensity of his/her pain over the last 24 hours. Jared indicates a pain score of 4[10].
Objective[edit | edit source]
General Observations[edit | edit source]
- Jared has slightly stooped posture including a forward head posture while sitting and standing.
- There is mild muscle atrophy in Jared’s hands and lower extremities including the quadriceps and calf muscles.
- There is mild bruising on Jared’s elbows and hips secondary to falls.
- There is visible fasciculations of Jared’s quadriceps bilaterally.
Speech and Language[edit | edit source]
Jared’s parents and family physician indicated a slightly slower and hyper-nasal voice.
Tone and Sensation[edit | edit source]
- Sensation tested using a dermatomal pattern for the hot/cold and sharp/dull testing. No significant findings were found.
- To rule out combined cortical sensation impairments, testing including graphesthesia and stereognosis was completed. No significant findings were found.
- Tone was assessed using the Modified Ashworth Spasticity Scale [11]. Findings include:
- Increased tone in global muscles.
- UE = 1+; LE = 1
Motor Control[edit | edit source]
- Global strength was measured using manual muscle testing (MMT)[12]. Findings include:
- Bilateral ankle dorsiflexion = 3-/5
- Wrist extension = 3+/5
- Hip flexors = 3+/5
- Hip extensors = 3+/5
- Knee extension = 3+/5
- Grip Strength was measured using held dynamometer (HHD)[7]. Findings include:
- Lower than average grip strength
- L = 30kg; R =35kg
- Active Range of Motion (AROM) was measured using goniometry
- All AROM are WNL except:
- Bilateral wrist extension = 50°
- Bilateral finger extension (DIP, PIP, MCP) = MCP 30-45°; PIP, 0°; DIP, 20°
- Bilateral elbow extension = 10°
- Bilateral dorsiflexion = 0°
- All AROM are WNL except:
- Passive Range of Motion (PROM)
- Able to straighten out trunk/posture when asked and held it for 30 seconds then went back to stoop posture
- PROM all WNL
- Manual dexterity was assessed using the Purdue Pegboard Test (PPBT)[13][14].
- Jared’s overall dexterity was slowed bilaterally with his non-dominant (L) hand scoring slightly slower than his R hand.
- Right hand: 9
- Left hand: 8
- Both hands: 10
- Right + Left + Both hands: 27
- Assembly: 32
- Jared’s overall dexterity was slowed bilaterally with his non-dominant (L) hand scoring slightly slower than his R hand.
Neurological Testing[edit | edit source]
- Upper Motor Neurons (UMN)
- Positive Babinski's sign bilaterally
- Positive Clonus Test bilaterally
- Lower Motor Neurons (LMN)
- Increased Achilles reflex - Grade 4+
- Increased patellar reflex - Grade 3+
- Increased biceps reflex - Grade 3+
- Increased triceps reflex - Grade 3+
Balance[edit | edit source]
Balance was measured using the miniBESTest for a baseline[15].
- Jared got a total score of 17/28.
- Subscores
- Anticipatory: 3/6
- Reactive Postural Control: 4/6
- Sensory Orientation: 4/6
- Dynamic Gait: 6/10
- Minimal Detectable Change: 5.5
Gait[edit | edit source]
Gait was assessed using the Ranchos Los Amigos Stages of Gait.
- Overall impression, Jared ambulates safely with some minimal balance deficits and decreased dorsiflexion in both feet. His step length was decreased bilaterally, which resulted in an increased double stance time. He also walked with a forward stooped posture.
- Initial contact - decreased heel strike bilaterally
- Loading response - normal
- Mid stance - normal
- Terminal stance - normal
- Pre-Swing - decreased hip extension bilaterally
- Initial Swing - Increased knee flexion bilaterally
- Mid-Swing - decreased dorsiflexion bilaterally
- Terminal Swing - no foot clearance bilaterally
ALS Functional rating scale - Revised (ALSFRS-R)[edit | edit source]
ALSFRS-R is a test used to measure the functional status of individuals with ALS. The ALSFRS-R is scored using 12 activities of daily living measured using a 5-point scale. The highest score for each item is 4 which represents normal function. The lowest score for each item is 0 which represents loss of the function being assessed. The total score for the scale is 48, with a higher score indicating a higher functioning individual[16][17].
Ventilatory Muscle Strength [edit | edit source]
- Maximal Inspiratory Pressure (MIP) = -102 cmH20 and Maximal Expiratory Pressure (MEP) = 143 cmH2O.
BMI [edit | edit source]
- 6 foot 1 in, 158 pounds:BMI of 21 (healthy/normal weight).
Clinical Impression[edit | edit source]
Physiotherapy Diagnosis[edit | edit source]
Jared is a 24-year-old male who presents to physiotherapy following a neurologist diagnosis of early-stage Amyotrophic Lateral Sclerosis (ALS) 6 months ago[18]. Jared and his parents indicated that he is currently independent in all his ADLs; however, he is having difficulties with certain ADLs requiring greater hand and finger dexterity, such as brushing his teeth. Jared has recently stopped playing recreational soccer as he was experiencing an increase in falls, difficulties with his balance, increased cramping, and weakness in his legs. Jared’s decreased grip strength and impaired hand and finger dexterity led him to take a leave from work, and they are currently preventing him from applying to dentistry school. Jared has a good social support system at home as he is living with his sister and parents. He expressed being motivated to start physiotherapy to continue leisurely hiking with his family and returning to work at the grocery store. Therefore, Jared would benefit from physiotherapy treatment focusing on maintaining his functional independence and muscle strength. Treatment should also include education on lifestyle modification and energy conservation strategies related to ALS.
Problem List (According to the ICF Framework)[edit | edit source]
Body Structure and Function
- Decreased grip strength in kg bilaterally.
- Decreased active wrist extension which influences dexterity and decreased dorsiflexion which influences ambulation.
- Mild muscle weakness globally, with upper and lower limb atrophy most notably in: Bilateral ankle dorsiflexion = 3-/5, Wrist extension = 3+/5, Hip flexion = 3+/5, Hip extension 3+/5, Knee extension = 3+/5.
- Potentially experiencing body dysmorphia since his diagnosis, as he has seen noticeable changes in his muscle mass.
- Demonstrated LMN hyperreflexia for upper and lower limb (Achilles 4+, patellar, triceps, biceps 3+).
- Demonstrated UMN hyperreflexia (Babinski and clonus).
- At risk of respiratory compromise with further neurodegeneration.
Activity
- Decreased speed while climbing stairs due to potential pain, cramping, and fatigue.
- Decreased dynamic and anticipatory balance and increased risk of falls according to miniBEST balance testing.
- ALSFRS-R score = 43/48.
- Decreased manual dexterity as shown in Purdue pegboard test.
- Drop foot gait patterning.
Participation
- Unable to work due to frequent moderate muscle cramping, 4/10 pain and general upper and lower extremity weakness.
- Unable to hike with family on the weekends due to weakness and pain.
- Unable to study to become a dentist due to decreased upper limb strength and hand and finger dexterity which hinders practical ability to study dentistry.
Intervention[19][20][edit | edit source]
| Type | Intensity | Frequency | Time |
|---|---|---|---|
Strength Exercises
|
8-12 reps making sure to reach muscle fatigue
(70-80% 1RM)
|
3x per week, with at least 48hrs rest between same muscle groups | 2-3 mins rest between sets |
Endurance Exercises
|
Moderate intensity (able to have a conversation while working) | 3x per week (every other day) | 30 minutes |
Inspiratory Muscle Training
|
8-12 reps making sure to reach muscle fatigue
(70-80% 1RM)
|
3x per week | 2-3 mins rest between sets |
Dexterity Training
|
To mental / physical fatigue
2-3 sets |
Recommended daily, but 3x a week minimum | 30 minutes recommended, or as tolerated |
| Stretching
Static stretching of:
|
Stretching sensation to the point of mild discomfort | Recommended daily, but 3x a week minimum | 30 second hold 3x a day |
Ischemic Compression/Trigger point release
|
Pressure into discomfort/pain (5/10 max pain) | Recommended daily, but 3x a week minimum | 30-60 second hold at each point |
Blance
|
As tolerated | Recommended daily, but 3x a week minimum | 30 seconds hold x3 sets |
Thermotherapy
|
Mild warm sensation | As needed | 15 minutes on, 45 minutes off (or until skin is back to normal temp) |
Education
|
N/A | N/A | N/A |
Outcome[edit | edit source]
Jared was very motivated to follow the intervention and plans set out from his physiotherapy sessions. He understood the importance of physical activity and strengthening to maintain/delay the progression of ALS. After the 1st week, Jared mentioned that he enjoyed the strength training and found the stretches, massages, and ischemic compressions to be helpful with his cramps and fatigue. He especially liked the hand-specific exercises, as he found himself more confident with his fine motor control skills (Ex., using his phone and laptop). He mentioned that his pain has become more tolerable and has only reached a maximum of 3/10 when using the NPRS compared to his previous score of 4/10 before physiotherapy sessions (in both calves and quads). Although Jared was doing well with all of his exercises, we did not believe that increasing the resistance/intensity of his exercises would benefit him. Increasing the intensity of the exercises may negatively affect his prognosis, and therefore we were cautious with progressing Jared’s interventions[21].
After three weeks of therapy, Jared’s global strength was reassessed through MMT and grip strength through the use of a dynamometer. His gait and balance were also reassessed. Overall, his strength was very similar to his initial assessment except for an increase in dorsiflexion strength to 3/5 bilaterally, wrist extensors to 4-/5 bilaterally, and knee extension strength to 4-/5 bilaterally. His grip strength slightly improved to 33kg on his L and 37kg on his R hand, but it is not clinically significant (4). His gait slightly improved, as Jared displayed better foot clearance and increased dorsiflexion during the swing phase bilaterally. Finally, Jared’s balance was re-assessed using the miniBESTest. He scored an 18/28 (Anticipatory: 4/6, Reactive Postural Control: 4/6, Sensory Orientation: 4/6, Dynamic Gait: 6/10). Jared's change in score does not represent a clinically significant difference; however, there were not any decreases in his balance skills. At this point, Jared felt slightly discouraged as there were no grand overall improvements. However, we had to re-emphasize the importance of maintaining his current physical performance, educating Jared on ALS and its prognosis, and the value of preventing the effects of ALS.
Finally, Jared was re-assessed after six weeks of therapy. From the general observation, we did not find any significant differences or changes. Additionally, there were no significant changes in Jared's overall AROM or PROM. We then measured various outcome measures, and their results were as follows: ALSSQOL-R: 7.2/10, NPRS: 4/10 most notably in his calves, ALSFRS-R: 44/48, MiniBESTest: 17/28 (Anticipatory: 4/6, Reactive Postural Control: 4/6, Sensory Orientation: 3/6, Dynamic Gait: 6/10), Purdue Pegboard Test: overall = 31, assembly = 36 (right hand:11, left hand: 9, both hands: 11). In terms of gait, Jared displayed a similar gait pattern; however, his overall posture was better with a decreased forward stooped posture, in comparison to three weeks ago. However, he mentioned that the pain in his calves had forced him to take more breaks when walking. Jared indicated that the pain comes on after 10 minutes of constant walking, but a 5-minute break is enough for him to continue walking before the cycle continues again. As a 5-minute break is enough, Jared's endurance interventions were altered slightly. Since Jared was doing both the endurance exercises and participating in frequent walks with his family, we had proposed to Jared to continue his frequent walks with his family and eliminate any extra endurance activities (ellipticals and walking on a treadmill) on those days. That way, we hoped to reduce his general pain and control his lower extremity muscle fatigue. In terms of overall strength, there were few deviations compared to Jared's strength that was assessed three weeks ago. His R grip strength was 37kg, and his L grip strength was 34kg. His MMT scores were similar; however, there was an increase in strength bilaterally in his dorsiflexion (3+/5) and an increase in strength bilaterally in his hip flexors and extensors (4-/5).
Although there were no significant changes in most of Jared's results/measures compared to six weeks ago, having stable/consistent scores in many of the outcome measures was seen as a positive due to the progressive nature of ALS. In other words, the interventions that were given by the PT, along with the other interventions implemented by the rest of the healthcare team (neurologist, family doctor, OT, dietician, etc.), may have been effective in preventing the acute progressive nature of Jared’s juvenile ALS.
Discussion[edit | edit source]
ALS is a progressive neurodegenerative disease associated with the degeneration of upper and lower motor neurons, and results in a vast presentation of symptoms relating to motor control[1]. In addition to the impact on the motor neurons, ALS has devastating implications for one’s overall wellbeing, often leading to depression and feelings of hopelessness. Although there is no cure for ALS, multidisciplinary management is important for optimizing functional independence and QOL. This can be done through maintaining strength, mobility, lifestyle modifications, energy preservation strategies, and preparation for end of life[22].
This fictional case study was developed to illustrate the progressive nature of ALS through a physiotherapy subjective and objective assessment and to demonstrate a potential physiotherapy management plan. Jared is a 24-year-old soccer player who presents with juvenile ALS. After completing a physiotherapy assessment, it was found that Jared has mild muscular atrophy in his hands, quadriceps, and calves, increased muscle tone in both the upper and lower extremities, a moderate overall decrease in strength, decreased ROM in his distal extremities, and modest changes in gait. As a young athlete and aspiring dentist, Jared expresses feeling discouraged regarding the progressive nature of this condition. However, with encouragement from his support system, Jared feels motivated to attend physiotherapy to improve his overall strength and balance, and hopes return to work and leisurely hiking with his family.
The discussion of whether individuals with progressive degenerative diseases—such as ALS—should exercise has been a controversial topic. Previous literature has been inconclusive regarding the benefits of exercise in ALS; it was traditionally thought that exercise may enhance deterioration[23]. However, recent literature has demonstrated the potential of exercise to delay the progression of the condition, and thus, improve functional ability[23]. Meng et al.[23] found that the benefits of exercise were better demonstrated in the long-term, which is likely observed in patients who have a slower disease course. Majmudar et al.[5] suggest that moderate exercise is safe for those with ALS, however, the delivery of these guidelines requires specific attention to the status of the patient.
Jared’s management plan focuses on strengthening and endurance exercises for the upper and lower extremities, as well balance training, with the goal being to maintain or recover strength and balance required for functional independence. Endurance exercises include ambulation on a treadmill, and balance exercises include exercises such as single leg stance. In addition, the multidisciplinary team provided Jared with the necessary education and tools for optimizing his function and QOL. This education included information on juvenile ALS, pain science, energy conservation, gait aids, and lifestyle modifications. Jared was referred to an occupational therapist for assistance with performing ADLs, and a registered dietitian for guidance on obtaining optimal nutrition throughout his degenerative condition. Various outcome measures were used to assess his strength and balance; after 6 weeks of physiotherapy, Jared’s strength and balance were both maintained. Due to the rapid and unpredictable nature of ALS, the maintenance of his current status is a positive finding and has optimistic implications on his functioning and QOL.
Jared’s case provides a framework for management of patients with ALS who are diagnosed at a young age. The onset of ALS most commonly occurs between the ages of 50 and 75, and therefore, research has focused on ALS as a disease that impacts those later in life. However, it is important for members of the interdisciplinary team to not only be aware of juvenile ALS, but also be able to alter their treatment to target the goals of this younger population. Age is a strong predictor for prognosis, indicating that the older the age of diagnosis, the worse the outcome[24]. In this fictional case study, Jared was diagnosed with ALS at the age of 24, which is much younger than the typical age of onset. For this reason, it is predicted that Jared will have a slower advancement of symptoms; this was demonstrated throughout the case study. Furthermore, this case study was used to illustrate the variability of ALS symptoms and progression of disease. Despite having the same diagnosis, each patient will have a unique experience of symptoms, needs, and goals. Thus, it is imperative that health care professionals incorporate the patient into their management plan, and tailor their treatment specifically to each patient.
Interdisciplinary Management of ALS[edit | edit source]
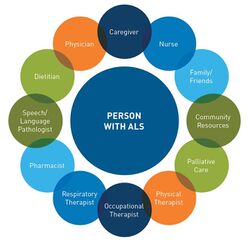
Patient-centred, interdisciplinary, and comprehensive rehabilitation is vital for individuals with ALS and has been shown to significantly improve their care and QOL[25]. Health care professionals who may be involved in the care of individuals with ALS include the patient’s family and friends, family physician, neurologist, physiotherapists, occupational therapists (OTs), registered dieticians, speech language therapists, social workers and palliative care.
Occupational Therapist[edit | edit source]
OTs play an integral role in the interdisciplinary care of individuals with ALS. There are many tasks that an OT can perform to help ALS patients maintain maximum functional independence. They can also play a role in altering the patient’s attitude and perspective, to shift towards focussing on tasks that they can perform, rather than those they can’t. Although Jared is currently independent in his ADLs, he is experiencing increasing difficulty with ADLs requiring hand motor dexterity. Therefore, an OT can play a role in fitting and prescribing Jared with upper extremity bracing or adaptive devices. For example, adaptive large grip utensils may be recommended to allow individuals with ALS to maintain independence while eating or a resting hand splint may be recommended to prevent wrist and finger flexion contractures[5]. Jared is currently able to ambulate independently, however, as his disease progresses, he will likely require the use of an Ankle-Foot Orthosis (AFO) or a gait aid. Gait aids may include a cane, walker and eventually a wheelchair[5]. An OT will play a major role in fitting and prescribing an AFO and/or a gait aid to Jared.
Additionally, an OT plays a role in educating individuals with ALS and their families on energy conservation and fatigue management. For example, OTs can provide education on the benefits of breaking up high-energy tasks by incorporating rest breaks into their daily activities and planning their day to prioritize the tasks that are most important to them. This type of education has shown to be effective in reducing fatigue, managing fatigue symptoms and improving different aspects such as health-related quality of life[26].
Finally, during the later stages of ALS, the OT may conduct a home assessment and provide recommendations to the family on certain modifications that they may want to make to enhance the individual’s mobility and safety. For example, a ramp may be recommended to enter the home, or a stair lift if the individual with ALS lives in a multi-story home like Jared. In addition, the OT will likely give instructions to the family members and caregivers on how they can assist and support their family member with ALS with their exercises, proper positioning, how to lift and transfer the individual and how to use the assistive devices[27]. Therefore, it is evident that OTs play an essential role in the interdisciplinary care team for patients with ALS as they can assist in a multitude of ways throughout the disease progression.
Registered Dietician [edit | edit source]
A second key member of the interdisciplinary care team for patients with ALS are registered dieticians (RD). RDs can provide a variety of different treatment options for ALS depending on the physical and nutritional status of the individual. As previously indicated, muscle weakness is a common symptom with ALS. This weakness can affect eating and swallowing, thus RDs can help individuals with ALS to optimize their diet, maintain or improve their nutritional status, minimize weight loss and maintain fluid intake.
In our case study, Jared is recently diagnosed with juvenile ALS and still has a high level of function. He is experiencing some muscle weakness; however, he does not currently have any difficulties with swallowing. Therefore, the role of the RD may be centred around assisting Jared to optimize his diet and maintain or improve his nutritional status. This may be through evidence-based nutritional guidance in the form of nutritional monitoring, meal planning, and an individualized diet targeted for optimal nutrition. Throughout this process, the RD would focus on areas such as caloric and hydration requirements, macronutrient and micronutrient requirements, and supplementation to optimize Jared’s QOL. This is important for Jared as his score on the ALSSQOL-R is 7.2/10, which indicates that there are areas that need to be addressed in order to improve his QOL.
Additionally, as Jared is still walking and wants to get back to hiking with his family, a RD could help him to monitor or improve his nutritional status to maintain his energy levels for these activities. By monitoring his nutritional status, Jared and the RD will be able to identify and address any potential risks for malnutrition[28].
Moreover, individuals with ALS are at an increased risk of weight loss due to several factors, including malnutrition, difficulties swallowing, potential increased caloric expenditure from muscular fasciculations and decreased caloric intake due to comorbid mental illnesses[29]. Jared currently has a healthy BMI of 21, however, has noticed a decrease in muscle mass. An increased BMI is associated with more favourable outcomes in individuals with ALS[30]. Therefore, an RD can assist Jared with minimizing weight loss and maintaining his BMI[30].
Finally, as the disease progresses, 85% of individuals with ALS will experience difficulties swallowing, also known as dysphagia[31]. Therefore, the role of the RD will transition to having a large focus on assessing the severity of dysphagia and providing nutritional management[32]. The purpose of the assessment of dysphagia is to identify the risk of aspiration, developing pneumonia, and choking, and whether oral or non-oral routes of hydration and nutrition are indicated[32]. In these cases, RDs assess the individual’s need for alternative methods to oral feeding such as a percutaneous endoscopic gastrostomy in which a feeding tube bypasses the esophagus and is inserted through the abdominal wall into the stomach for enteral nutrition[28]. This alternative to oral feeding helps to improve or maintain nutritional status when more severe dysphagia is present in the advanced stages of ALS. Maintaining nutritional status is critical to prevent weight loss and fatigue. Although Jared is still in the early stages of the condition, both Jared and his family should work together with an RD in the future to discuss potential options.
In summation, RDs are an essential part of the interdisciplinary healthcare team for individuals with ALS and should be incorporated to help manage nutrition in both the early and more advanced stages of the condition.
Self-study questions[edit | edit source]
1. Why would a PT utilize a peak flow meter in the management of a neurological condition such as ALS?
A) To self-manage and identify respiratory status, and be able to implement an emergency action plan when peak flow rates decline
B) For expiratory muscle training associated with decreased strength in progressive ALS
C) To determine the strength of a cough to clear secretions that accumulate in the airways with immobility
D) A+C
E) All of the above
2. What is the pathophysiology of ALS?
A) Degeneration of upper and lower motor nerves
B) Degeneration of peripheral sensory nerves
C) Demyelination of the myelin sheath of peripheral sensory nerves
D) All of the above
E) None of the above
3. When recently diagnosed with limb-onset ALS, what are typical initial symptoms?
A) Impaired sensation in the distal upper and lower limb
B) Respiratory compromise
C) Muscle weakness and atrophy in distal limbs
D) Presence of cognitive deficits
E) None of the above
Answer Key
1. D
2. A
3. C
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 Amyotrophic Lateral Sclerosis (ALS) Fact Sheet [Internet]. Bethesda, MD 20892: National Institute of Neurological Disorders and Stroke; [cited 2021May11]. Available from: https://www.ninds.nih.gov/disorders/patient-caregiver-education/fact-sheets/amyotrophic-lateral-sclerosis-als-fact-sheet
- ↑ The ALS Association. What is ALS?. Available from: https://www.youtube.com/watch?v=aDpN-6EAd3k [last accessed 5/10/2021]
- ↑ 3.0 3.1 3.2 3.3 Jamrozik Z, Gawel M, Szacka K, Bakon L. A case report of amyotrophic lateral sclerosis in a patient with Klippel–Feil Syndrome—a familial occurrence: A potential ole of TGF-β signaling pathway. Medicine[Internet]. 2015 Jan [cited 2021 May 10];94(4). doi: 10.1097/MD.0000000000000441
- ↑ 4.0 4.1 Venizelos A, Park Y, Fisher MA. A patient with amyotrophic lateral sclerosis and atypical clinical and electrodiagnostic features: a case report. Journal of medical case reports. 2011 Dec [cited 2021 May 13];5(1):1-5. doi: 10.1186/1752-1947-5-538
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 Majmudar S, Wu J, Paganoni S. Rehabilitation in amyotrophic lateral sclerosis: why it matters. Muscle & Nerve [Internet]. 2014 Jul [cited 2021 May 9];50(1):4-13. doi: 10.1002/mus.24202.
- ↑ Tsitkanou S, Della Gatta P, Foletta V, Russell A. The role of exercise as a non-pharmacological therapeutic approach for amyotrophic lateral sclerosis: beneficial or detrimental?. Frontiers in neurology [Internet]. 2019 Jul 17 [cited 2021 May 13];10:783. doi: 10.3389/fneur.2019.00783
- ↑ 7.0 7.1 Norman K, Stobäus N, Gonzalez MC, Schulzke JD, Pirlich M. Hand grip strength: outcome predictor and marker of nutritional status. Clin Nutr [Internet]. 2011 Apr 1 [cited 2021 May 9];30(2):135-42. doi: 10.1016/j.clnu.2010.09.010
- ↑ Miller RG, Mitchell JD, Moore DH. Riluzole for amyotrophic lateral sclerosis (ALS)/motor neuron disease (MND). Cochrane Database of Syst Rev [Internet]. 2002 [cited 2021 May 9];(3). doi: 10.1002/14651858.CD001447
- ↑ Felgoise SH, Simmons Z, Brothers A, Stephens HE, Walsh SM. The ALS Specific Quality of Life-Revised (ALSSQOL-R) User’s Guide [Internet]. 2011 [cited 2021 May 11]. Available from: https://www.pennstatehealth.org/sites/default/files/Neurology/ALSSQOL-%20Manual.pdf
- ↑ Numeric Pain Rating Scale [Internet]. Shirley Ryan AbilityLab. [cited 2021 May 11]. Available from: https://www.sralab.org/rehabilitation-measures/numeric-pain-rating-scale
- ↑ Ashworth Scale / Modified Ashworth Scale [Internet]. Chicago, IL: Shirley Ryan AbilityLab. [updated 2016 May 26, cited 2021May11]. Available from: https://www.sralab.org/rehabilitation-measures/ashworth-scale-modified-ashworth-scale
- ↑ Cudkowicz M, Qureshi M, Shefner J. Measures and markers in amyotrophic lateral sclerosis. NeuroRx [Internet]. 2004 Apr 1 [Cited 2021 May 9];1(2):273-83. doi: 10.1602/neurorx.1.2.273
- ↑ Marvin K. Purdue Pegboard Test (PPT) [Internet]. Strokengine. [updated 2012 September 9, cited 2021May11]. Available from: https://strokengine.ca/en/assessments/purdue-pegboard-test-ppt/
- ↑ Purdue Pegboard Test [Internet]. Lafayette, IN: Lafayette Instrument [updated 2021 March 3, cited 2021 May 9]. Available from: https://lafayetteevaluation.com/products/purdue-pegboard
- ↑ Mini balance evaluation systems test [Internet]. Chicago, IL: Shirley Ryan AbilityLab; [updated 2013 June 4, cited 2021 May 11]. Available from: https://www.sralab.org/rehabilitation-measures/mini-balance-evaluation-systems-test
- ↑ Outcome measures [Internet]. Utrecht, the Netherlands: ENCALS; [cited 202 1May 11]. Available from: https://www.encals.eu/outcome-measures/
- ↑ The ALS C.A.R.E. Program. Interpretation guides to standardized questionnaires employed in the ALS CARE database [Internet]. Worcester, MA: University of Massachusetts Medical School; [cited 2021 May 11]. Available from: https://www.outcomes-umassmed.org/als/sf12.aspx
- ↑ Dal Bello-Haas V, Kloos AD, Mitsumoto H. Physical therapy for a patient through six stages of amyotrophic lateral sclerosis. Physical Therapy [Internet]. 1998, December 1 [Cited 2021 May 11]; 78(12), pp.1312-1324. doi: 10.1093/ptj/78.12.1312
- ↑ American College of Sports Medicine. ACSM's guidelines for exercise testing and prescription. Lippincott Williams & Wilkins; 2013 Mar 4
- ↑ Dal Bello-Haas VD. Physical therapy for individuals with amyotrophic lateral sclerosis: current insights. Degenerative neurological and neuromuscular disease. 2018;8:45–54
- ↑ O'Sullivan SB, Schmitz TJ, Fulk GD, O'Sullivan SB. Amyotrophic Lateral Sclerosis. In: Physical rehabilitation. 7th ed. Philadelphia: F.A. Davis; 2019. p. 739–40
- ↑ Soriani MH, Desnuelle C. Care management in amyotrophic lateral sclerosis. Revue neurologique. 2017 May 1 [cited 2021 May 10];173(5):288-99. doi: 0.1016/j.neurol.2017.03.031
- ↑ 23.0 23.1 23.2 Meng L, Li X, Li C, Tsang RCC, Chen Y, Ge Y, Gao Q. Effects of exercise in patients with amyotrophic lateral sclerosis. American Journal of Physical Medicine & Rehabilitation [Internet]. 2020, September [cited 2021 May 09]; 99(9): 801-810. doi: 10.1097/PHM.0000000000001419
- ↑ Chiò A, Logroscino G, Hardiman O, Swingler R, Mitchell D, Beghi E, Traynor BG, Consortium E. Prognostic factors in ALS: A critical review. Amyotroph Lateral Scler [Internet]. 2009, October [cited 2021 May 11]; 99(5-6): 310–323. doi: 0.3109/17482960802566824
- ↑ Paganoni S, Karam C, Joyce N, Bedlack R, Carter GT. Comprehensive rehabilitative care across the spectrum of amyotrophic lateral sclerosis. NeuroRehabilitation. 2015 Jan 1 [cited 2021 May 8];37(1):53-68. doi: 10.3233/NRE-151240
- ↑ De-Bernardi-Ojuel L, Torres-Collado L, García-de-la-Hera M. Occupational therapy interventions in adults with multiple sclerosis or amyotrophic lateral sclerosis: a scoping review. International Journal of Environmental Research and Public Health [Internet]. 2021 Feb 3 [cited 2021 May 9];18(4):1432. doi: 10.3390/ijerph18041432
- ↑ MDA-ALS Center. Occupational and physical therapy [Internet]. Pittsburgh, PA 15213: University of Pittsburgh; [updated 2021 May 3, cited 2021 May 11]. Available from: https://www.alsclinic.pitt.edu/patient-issues/occupational-and-physical-therapy
- ↑ 28.0 28.1 Rio A, Cawadias E. Nutritional advice and treatment by dietitians to patients with amyotrophic lateral sclerosis/motor neurone disease: a survey of current practice in England, Wales, Northern Ireland and Canada. Journal of human nutrition and dietetics. 2007 Feb [cited 2021 May 11];20(1):3-13. doi: 10.1111/j.1365-277X.2007.00745.x
- ↑ Körner S, Hendricks M, Kollewe K, Zapf A, Dengler R, Silani V, Petri S. Weight loss, dysphagia and supplement intake in patients with amyotrophic lateral sclerosis (ALS): impact on quality of life and therapeutic options. BMC neurology. 2013 Dec [cited 2021 May 7];13(1):1-9. doi: 10.1186/1471-2377-13-84
- ↑ 30.0 30.1 Ning P, Yang B, Li S, Mu X, Shen Q, Hu F, Tang Y, Yang X, Xu Y. Systematic review of the prognostic role of body mass index in amyotrophic lateral sclerosis. Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration. 2019 Jul 3 [cited 2021 May 10];20(5-6):356-67. doi: 10.1080/21678421.2019.1587631
- ↑ Onesti E, Schettino I, Gori MC, Frasca V, Ceccanti M, Cambieri C, Ruoppolo G, Inghilleri M. Dysphagia in amyotrophic lateral sclerosis: impact on patient behavior, diet adaptation, and riluzole management. Frontiers in Neurology [Internet]. 2017 Mar 21 [Cited 2021 May 13]; 8:94. doi: 10.3389/fneur.2017.00094
- ↑ 32.0 32.1 College of Dieticians of Ontario. Scope of practice and controlled acts [Internet]. Toronto, ON: College of Dietitians of Ontario [cited 2021 May 10]. Available from: https://www.collegeofdietitians.org/programs/practice-advisory-program/professional-practice-resources/scope-of-practice.aspx#:~:text=The%20Dietetic%20Scope%20of%20Practice,related%20disorders%20by%20nutritional%20means.%E2%80%9D