Hypertension: Difference between revisions
No edit summary |
No edit summary |
||
| Line 8: | Line 8: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
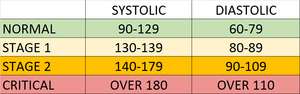
[[File:Hypertension ranges chart.png|right|frameless]] | [[File:Hypertension ranges chart.png|right|frameless]] | ||
The current definition of hypertension (HTN) is systolic [[Blood Pressure|blood pressure]] (SBP) values of 130mmHg or more and/or diastolic blood pressure (DBP) more than 80 mmHg. | The current definition of hypertension (HTN) is systolic [[Blood Pressure|blood pressure]] (SBP) values of 130mmHg or more and/or diastolic blood pressure (DBP) more than 80 mmHg. Persistent BP readings of 140/90mmHg or more should undergo treatment with the usual therapeutic target of 130/80mmHg or less.<ref name=":0">Iqbal AM, Jamal SF. [https://www.ncbi.nlm.nih.gov/books/NBK539859/?report=reader Essential Hypertension.] InStatPearls [Internet] 2019 Dec 1. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK539859/?report=reader (last accessed 11.12.2020)</ref> | ||
Salient Facts | Salient Facts | ||
| Line 17: | Line 16: | ||
* In 2015, 1 in 4 men and 1 in 5 women had hypertension. | * In 2015, 1 in 4 men and 1 in 5 women had hypertension. | ||
* Fewer than 1 in 5 people with hypertension have the problem under control. | * Fewer than 1 in 5 people with hypertension have the problem under control. | ||
* Hypertension is a major cause of premature death worldwide. | * Hypertension is a major cause of premature death worldwide and ranks among the most common [[Chronic Disease|chronic medical condition]].<ref name=":0" /> | ||
* One of the global targets for noncommunicable diseases is to reduce the prevalence of hypertension by 25% by 2025 (baseline 2010)<ref>WHO [https://www.who.int/news-room/fact-sheets/detail/hypertension Hypertension] Available from:https://www.who.int/news-room/fact-sheets/detail/hypertension (last accessed 11.12.2020)</ref>. | * One of the global targets for noncommunicable diseases is to reduce the prevalence of hypertension by 25% by 2025 (baseline 2010)<ref name=":1">WHO [https://www.who.int/news-room/fact-sheets/detail/hypertension Hypertension] Available from:https://www.who.int/news-room/fact-sheets/detail/hypertension (last accessed 11.12.2020)</ref>. | ||
== Etiology == | |||
Most cases of hypertension are idiopathic which is also known as essential hypertension. | |||
* It has long been suggested that an increase in salt intake increases the risk of developing hypertension. | |||
* One of the described factors for the development of essential hypertension is the patient genetic ability to salt response. About 50 to 60% of the patients are salt sensitive and therefore tend to develop hypertension<ref name=":0" /> | |||
== Risk Factors == | |||
Modifiable risk factors include unhealthy diets (excessive salt consumption, a diet high in saturated fat and trans fats, low intake of fruits and vegetables), physical inactivity, consumption of tobacco and alcohol, and being overweight or obese. | |||
Non-modifiable risk factors include a family history of hypertension, age over 65 years and co-existing diseases such as diabetes or kidney disease<ref name=":1" />. | |||
== Signs and Symptoms == | |||
Hypertension is called a "silent killer". Most people with hypertension are unaware of the problem because it may have no warning signs or symptoms. | |||
* When symptoms do occur they include: early morning headaches; nosebleeds; irregular heart rhythms; vision changes; buzzing in the ears. | |||
* Severe hypertension can cause: fatigue; nausea; vomiting; confusion; anxiety; chest pain; muscle tremors. | |||
* An evaluation of BP by a health professional is important for assessment of risk and associated conditions<ref name=":1" />. | |||
== Epidemiology == | |||
* More than one billion adults worldwide have hypertension with up to 45% of the adult populace being affected with the disease. | |||
* The high prevalence of hypertension is consistent across all socio-economic and income strata, and the prevalence rises with age accounting for up to 60% of the population above 60 years of age. | |||
* In the year 2010, the global health survey report (which comprised of patient data from 67 countries), reported Hypertension as the leading cause of death and disability-adjusted life years worldwide since the year 1990. | |||
== Pathophysiology == | |||
== Sub Heading 2 == | == Sub Heading 2 == | ||
== Non Pharmacological management == | |||
Non-pharmacological and lifestyle management are recommended for all individuals with raised BPs regardless of age, gender, comorbidities or cardiovascular risk status. | |||
* Patient education is paramount to effective management and should always include detailed instructions regarding weight management, salt restriction, smoking management, adequate management of obstructive sleep apnea and exercise. | |||
* Reducing and managing mental stress | |||
* Regularly checking blood pressure | |||
* Managing other medical conditions<ref name=":0" /><ref name=":1" /> | |||
== [[Pharmacological Management of Hypertension]] == | |||
Pharmacological therapy consists of angiotensin-converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARBs), diuretics (usually thiazides), calcium channel blockers (CCBs) and beta-blockers (BBs), which are instituted taking into account age, race and comorbidities such as presence of renal dysfunction, LV dysfunction, heart failure and cerebrovascular disease. See link above. | |||
== Complications == | |||
Coronary heart disease (CHD) | |||
Myocardial infarction (MI): Long-standing high blood pressure leads to left ventricular hypertrophy and diastolic dysfunction that cause an increase in myocardial rigidity, which renders the myocardium less compliant to changes in the preload, afterload, and sympathetic tone. Adequate blood pressure control must be achieved in patients with hypertension to prevent progression to overt heart failure<ref>Oh GC, Cho HJ. [https://clinicalhypertension.biomedcentral.com/articles/10.1186/s40885-019-0132-x Blood pressure and heart failure.] Clinical Hypertension. 2020 Dec 1;26(1):1.Available from:https://clinicalhypertension.biomedcentral.com/articles/10.1186/s40885-019-0132-x (last accessed 12.12.2020)</ref>. | |||
Stroke (CVA), either ischemic or intracerebral hemorrhage | |||
Hypertensive encephalopathy | |||
Renal failure, acute versus chronic | |||
Peripheral arterial disease | |||
Atrial fibrillation | |||
Aortic aneurysm | |||
Death (usually due to coronary heart disease, vascular disease, stroke-related) | |||
== Sub Heading 3 == | == Sub Heading 3 == | ||
Revision as of 07:21, 12 December 2020
This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! (12/12/2020)
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton, Nupur Smit Shah, Rishika Babburu and Areeba Raja
Introduction[edit | edit source]
The current definition of hypertension (HTN) is systolic blood pressure (SBP) values of 130mmHg or more and/or diastolic blood pressure (DBP) more than 80 mmHg. Persistent BP readings of 140/90mmHg or more should undergo treatment with the usual therapeutic target of 130/80mmHg or less.[1]
Salient Facts
- Hypertension - or elevated blood pressure - is a serious medical condition that significantly increases the risks of heart, brain, kidney and other diseases.
- An estimated 1.13 billion people worldwide have hypertension, most (two-thirds) living in low- and middle-income countries.
- In 2015, 1 in 4 men and 1 in 5 women had hypertension.
- Fewer than 1 in 5 people with hypertension have the problem under control.
- Hypertension is a major cause of premature death worldwide and ranks among the most common chronic medical condition.[1]
- One of the global targets for noncommunicable diseases is to reduce the prevalence of hypertension by 25% by 2025 (baseline 2010)[2].
Etiology[edit | edit source]
Most cases of hypertension are idiopathic which is also known as essential hypertension.
- It has long been suggested that an increase in salt intake increases the risk of developing hypertension.
- One of the described factors for the development of essential hypertension is the patient genetic ability to salt response. About 50 to 60% of the patients are salt sensitive and therefore tend to develop hypertension[1]
Risk Factors[edit | edit source]
Modifiable risk factors include unhealthy diets (excessive salt consumption, a diet high in saturated fat and trans fats, low intake of fruits and vegetables), physical inactivity, consumption of tobacco and alcohol, and being overweight or obese.
Non-modifiable risk factors include a family history of hypertension, age over 65 years and co-existing diseases such as diabetes or kidney disease[2].
Signs and Symptoms[edit | edit source]
Hypertension is called a "silent killer". Most people with hypertension are unaware of the problem because it may have no warning signs or symptoms.
- When symptoms do occur they include: early morning headaches; nosebleeds; irregular heart rhythms; vision changes; buzzing in the ears.
- Severe hypertension can cause: fatigue; nausea; vomiting; confusion; anxiety; chest pain; muscle tremors.
- An evaluation of BP by a health professional is important for assessment of risk and associated conditions[2].
Epidemiology[edit | edit source]
- More than one billion adults worldwide have hypertension with up to 45% of the adult populace being affected with the disease.
- The high prevalence of hypertension is consistent across all socio-economic and income strata, and the prevalence rises with age accounting for up to 60% of the population above 60 years of age.
- In the year 2010, the global health survey report (which comprised of patient data from 67 countries), reported Hypertension as the leading cause of death and disability-adjusted life years worldwide since the year 1990.
Pathophysiology[edit | edit source]
Sub Heading 2[edit | edit source]
Non Pharmacological management[edit | edit source]
Non-pharmacological and lifestyle management are recommended for all individuals with raised BPs regardless of age, gender, comorbidities or cardiovascular risk status.
- Patient education is paramount to effective management and should always include detailed instructions regarding weight management, salt restriction, smoking management, adequate management of obstructive sleep apnea and exercise.
- Reducing and managing mental stress
- Regularly checking blood pressure
- Managing other medical conditions[1][2]
Pharmacological Management of Hypertension[edit | edit source]
Pharmacological therapy consists of angiotensin-converting enzyme inhibitors (ACEi), angiotensin receptor blockers (ARBs), diuretics (usually thiazides), calcium channel blockers (CCBs) and beta-blockers (BBs), which are instituted taking into account age, race and comorbidities such as presence of renal dysfunction, LV dysfunction, heart failure and cerebrovascular disease. See link above.
Complications[edit | edit source]
Coronary heart disease (CHD)
Myocardial infarction (MI): Long-standing high blood pressure leads to left ventricular hypertrophy and diastolic dysfunction that cause an increase in myocardial rigidity, which renders the myocardium less compliant to changes in the preload, afterload, and sympathetic tone. Adequate blood pressure control must be achieved in patients with hypertension to prevent progression to overt heart failure[3].
Stroke (CVA), either ischemic or intracerebral hemorrhage
Hypertensive encephalopathy
Renal failure, acute versus chronic
Peripheral arterial disease
Atrial fibrillation
Aortic aneurysm
Death (usually due to coronary heart disease, vascular disease, stroke-related)
Sub Heading 3[edit | edit source]
Resources[edit | edit source]
- bulleted list
- x
or
- numbered list
- x
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Iqbal AM, Jamal SF. Essential Hypertension. InStatPearls [Internet] 2019 Dec 1. StatPearls Publishing.Available from:https://www.ncbi.nlm.nih.gov/books/NBK539859/?report=reader (last accessed 11.12.2020)
- ↑ 2.0 2.1 2.2 2.3 WHO Hypertension Available from:https://www.who.int/news-room/fact-sheets/detail/hypertension (last accessed 11.12.2020)
- ↑ Oh GC, Cho HJ. Blood pressure and heart failure. Clinical Hypertension. 2020 Dec 1;26(1):1.Available from:https://clinicalhypertension.biomedcentral.com/articles/10.1186/s40885-019-0132-x (last accessed 12.12.2020)