Noonan Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 23: | Line 23: | ||
* the PTPN11 gene | * the PTPN11 gene | ||
* the SOS1 gene | * the SOS1 gene | ||
* the | * the RIT1 gene | ||
* the KRAS | * the KRAS gene | ||
[[File:Autosomal Dominant Gene Structure.png|thumb|345x345px|Autosomal Dominant Gene Structure ]] | [[File:Autosomal Dominant Gene Structure.png|thumb|345x345px|Autosomal Dominant Gene Structure ]] | ||
Even though the symptoms are usually the same for all different genes, two of them are associated with specific conditions. The faulty '''PTPN11''' '''gene''' is commonly associated with pulmonary stenosis | Even though the symptoms are usually the same for all different genes, two of them are associated with specific conditions. The faulty '''PTPN11''' '''gene''' is commonly associated with pulmonary stenosis and the faulty '''RAF1''' '''gene''', associated with cardiomyopathy. | ||
Noonan Syndrome can be caused by mutations in multiple genes. Mutations in the altered genes occur at different degrees. The mutations in the PTPN11 gene cause about half of all cases. SOS1 gene mutations seem to be the second biggest with an additional 10 to 15 percent, followed by the genes RAF1 and RIT1 that account each for about 5 percent of cases. Mutations in other genes each account for a small number of cases. The cause of Noonan syndrome in 15 to 20 percent of people with this disorder is unknown. No matter how they acquired the gene mutation, people with Noonan syndrome have a 50% (1 in 2) chance of passing it onto their children.<ref name=":5">Noonan Syndrome. Available from https://www.stjude.org/disease/noonan-syndrome.html ( accessed 22 September, 2020)</ref> | Noonan Syndrome can be caused by mutations in multiple genes. Mutations in the altered genes occur at different degrees. The mutations in the PTPN11 gene cause about half of all cases. SOS1 gene mutations seem to be the second biggest with an additional 10 to 15 percent, followed by the genes RAF1 and RIT1 that account each for about 5 percent of cases. Mutations in other genes each account for a small number of cases. The cause of Noonan syndrome in 15 to 20 percent of people with this disorder is unknown. No matter how they acquired the gene mutation, people with Noonan syndrome have a 50% (1 in 2) chance of passing it onto their children.<ref name=":5">Noonan Syndrome. Available from https://www.stjude.org/disease/noonan-syndrome.html ( accessed 22 September, 2020)</ref> | ||
| Line 159: | Line 159: | ||
<div class="col-md-6"> {{#ev:youtube|28ID5WP2lAw|250}} <div class="text-right"><ref>Noonan Foundation. Overview of the genetics of Noonan syndrome. Available from: http://www.youtube.com/watch?v=28ID5WP2lAw&t=327s [last accessed 3/10/2020]</ref></div></div> | <div class="col-md-6"> {{#ev:youtube|28ID5WP2lAw|250}} <div class="text-right"><ref>Noonan Foundation. Overview of the genetics of Noonan syndrome. Available from: http://www.youtube.com/watch?v=28ID5WP2lAw&t=327s [last accessed 3/10/2020]</ref></div></div> | ||
<div class="col-md-6"> {{#ev:youtube|Ctp6Msz3Kgc|250}} <div class="text-right"><ref>The Traveling Awareness Bears. Noonan Syyndrome Awarenenss. Available from: http://www.youtube.com/watch?v=Ctp6Msz3Kgc [last accessed 3/10/2020]</ref></div></div> | <div class="col-md-6"> {{#ev:youtube|Ctp6Msz3Kgc|250}} <div class="text-right"><ref>The Traveling Awareness Bears. Noonan Syyndrome Awarenenss. Available from: http://www.youtube.com/watch?v=Ctp6Msz3Kgc [last accessed 3/10/2020]</ref></div></div> | ||
Revision as of 00:17, 4 October 2020
<div class="editorbox"> '''Original Editor '''- [[User:Kirenga Bamurange Liliane]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div>
<div class="editortbox">This article or area is currently under construction and may only be partially complete. Please come back soon to see the finished work! ({{REVISIONDAY}}/{{REVISIONMONTH}}/{{REVISIONYEAR}})</div>
Top Contributors - Kirenga Bamurange Liliane, Lucinda hampton, Chelsea Mclene, Naomi O'Reilly, Kim Jackson, Rucha Gadgil and Leana Louw
Definition[edit | edit source]
Noonan Syndrome (NS) is an autosomal dominant condition or a genetic mutation that prevents the normal development of different parts of the body. [1] It is a genetic condition that affects both girls and boys in so many ways including:
- distinctive facial features such as the broad or webbed neck, drooping eyelids, and a wider-than-usual distance between the eyes
- health problems such as short stature
- chest deformity
- congenital heart disease
- pulmonary stenosis
- physical problems
- possible developmental delays
Noonan and Ehmke were the first to describe a succession of patients with the same similarities including unusual facies and multiple malformations like congenital heart disease. As a result, these patients were previously thought to have a form of Turner Syndrome, which has a lot of similarities in its clinical features with Noonan Syndrome.[1]
The eponym “Noonan syndrome” was then adopted in recognition of Dr. Jacqueline Noonan who was the first to indicate that this condition occurs in both genders; could be associated with normal chromosomes included congenital heart defects and could be familial.[2]
Epidemiology / Pathological Process[edit | edit source]
The Noonan Syndrome is caused by a mutation of a gene or a faulty gene that is usually inherited from one of the parents. The most commonly altered genes are:
- the PTPN11 gene
- the SOS1 gene
- the RIT1 gene
- the KRAS gene
Even though the symptoms are usually the same for all different genes, two of them are associated with specific conditions. The faulty PTPN11 gene is commonly associated with pulmonary stenosis and the faulty RAF1 gene, associated with cardiomyopathy.
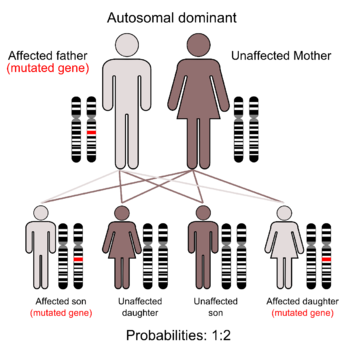
Noonan Syndrome can be caused by mutations in multiple genes. Mutations in the altered genes occur at different degrees. The mutations in the PTPN11 gene cause about half of all cases. SOS1 gene mutations seem to be the second biggest with an additional 10 to 15 percent, followed by the genes RAF1 and RIT1 that account each for about 5 percent of cases. Mutations in other genes each account for a small number of cases. The cause of Noonan syndrome in 15 to 20 percent of people with this disorder is unknown. No matter how they acquired the gene mutation, people with Noonan syndrome have a 50% (1 in 2) chance of passing it onto their children.[3]
There are 2 types of mutations that cause Noonan Syndrome:
- Inherited. Children who have one parent with Noonan syndrome who carries the defective gene (autosomal dominant) have a 50 percent chance of developing the disorder.
- Random. Noonan syndrome can develop because of a new mutation in children who don't have a genetic predisposition for the disorder (de novo).[4]
The condition is present from before birth, although milder cases may not be diagnosed until a child gets older. Its incidence is believed to be between 1 in 1000 and 1 in 2500 children.[5]
Clinical Presentation[edit | edit source]
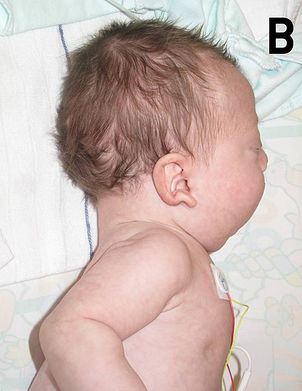
NS is most often characterized by facial and musculoskeletal features. Although these features are more present during early childhood, they change over time and appear less characteristic during adulthood:
- In the newborn infant, the head is large with a small face, a tall forehead, wide-spaced eyes, short nose, low set ears, and a broad or webbed neck
Many infants with NS also have heart (cardiac) defects such as
- Pulmonary valvular stenosis
- Hypertrophic cardiomyopathy
- Septal defects
The following characteristics are also seen among individuals with NS:
- Short stature: up to 83% of people with NS have a short stature
- Pectus deformity of the chest with pectus carinatum (protrusion of sternum and rib) and pectus excavatum (hollow chest)
- Kyphosis
- Scoliosis
- Cubitus valgus (outward deviation of the elbows)
- Rounded shoulders
- Rib abnormalities
- Genu valgum ( Knock knees)
- Joint hyperextensibility
- Talipes equinovarus[6]
Individuals with NS may also present less common problems including:
- Learning disability: children with NS tend to often have a mild learning disability due to a lower IQ average
- Feeding problems: children with NS may have problems with sucking and chewing
- Speech problems: articulation difficulty due to a high arched palate and weak muscles
- behavioral problems: some children with NS may have attention problems or difficulty to describe their or people emotions
- Eyes condition such as squint, lazy eye, strabism
- Hearing loss
- Hypotonia: decreased muscle tone will make children with NS reach early milestones later compared to other children
- Undescended testicles: one or both testicles may fail to drop into the scrotum in boys with NS
- Infertility can be diagnosed in boys if undescended testicles are not corrected at an early age
- Lymphoedema
- Bone marrow problems- Leukemia
- Skin problems such as dystrophic nails; extra prominence on pads of fingers and toes; follicular keratosis; hyperelastic skin; moles; thick curly hair or thin sparse hair.[5]
Diagnostic Procedures[edit | edit source]
NS may be suspected before birth based on the results of fetal ultrasonography which is used to create an image of the developing fetus.[7] The diagnosis of Noonan syndrome can be made clinically by observing the specific characteristics associated with the condition. These specific characteristics include congenital heart defect; a developmental delay that may vary depending on people; short stature; chest malformations as well as facial features.[8] However, because these symptoms can have different causes, further testing is suggested. These tests help to determine the extent of the symptoms and may include:
- Genetic Testing
- Electrocardiogram (ECG)
- Echocardiogram
- Blood Tests
- Educational Assessment
- Eye Test
- Hearing Test.[9]
- Plotting of growth parameters on NS growth charts
- Renal ultrasound examination
- Clinical and radiographic assessment of spine and rib cage
- Brain and cervical spine MRI if neurologic symptoms are present
- Multidisciplinary developmental evaluation[7].
Differential Diagnosis[edit | edit source]
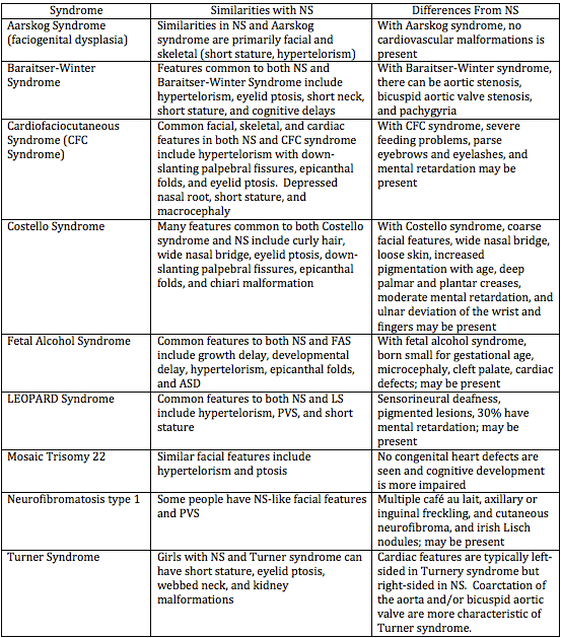
Several conditions have been found to have similarities with Noonan Syndrome and are identified as RASopathies. These conditions all have similar signs and symptoms and are caused by changes in the same cell signaling pathway. Besides Noonan syndrome, the RASopathies consist of cardiofaciocutaneous syndrome, Costello syndrome, Neurofibromatosis type 1, Legius syndrome, and Noonan syndrome with multiple lentigines.[10] The differential diagnosis, therefore, includes Williams syndrome, intrauterine exposure to primidone, fetal alcohol syndrome, and Aarskog syndrome. Other cardiocutaneous syndromes such as LEOPARD syndrome, neurofibromatosis, and Watson syndrome have a markedly overlapping phenotype.[11]
Similarities and Differences between NS and Other Disorders[edit | edit source]
Management / Interventions[edit | edit source]
Although it's possible to treat many aspects of NS, there is no typical treatment of NS.[12] Because the presentation of NS can be mild and the typical facial features lessen with age, the diagnosis might be neglected or missed. Therefore, a regular comprehensive follow-up in a multidisciplinary approach is needed to manage the medical and developmental complications of Noonan syndrome.[4]
Medical Management[edit | edit source]
The medical treatment will focus observed such as:
- Heart Defects:
- with pulmonary stenosis: no treatment will be required if it's mild. If it's severe a surgery will be required to narrow the valves
- hypertrophic cardiomyopathy may need to be treated with either medication such as beta-blockers or surgery to remove or destroy some of the excess heart muscle
- septal defects usually get better with age and thus do not need any treatment.[13]
- Growth issues: a growth hormone therapy is given around 4 to 5 years old. The medication Somatropin, a single daily injection is the most used. By adulthood, some people with Noonan syndrome may have normal height, but short stature is more common.
- Feeding and speech problems: speech therapy to effectively use the muscles of the mouth and develop them
- Undescended testicles: a surgical procedure called orchidopexy is performed
- Learning Disabilities: special educational needs and the assessment procedure.[13]
- Gross and fine motor delays to be assessed and treated by Occupational Therapists and Physiotherapy
People of any age with Noonan syndrome may be at an increased risk of cancer. They need to adopt healthy habits throughout life. It is imperative that they regularly do have physical checkups and screenings.[3]
Physiotherapy Management[edit | edit source]
In addition to medical management, patients may need to be referred for physiotherapy. The physiotherapy treatment will focus on patient education, improvement of the range of motion; strengthening exercises as well as pain management.
Early Intervention is crucial for a child diagnosed with Noonan Syndrome as they tend to delay in meeting motor milestones. The following exercises improve and maintain flexibility, endurance, strength, coordination, and balance in children diagnosed with Noonan Syndrome:[14]
- Sit-ups: from lying down on their back the child comes up to a full sitting position by holding the therapist's fingers
- Tall kneel: Place your child in a tall kneel position at the couch and let them play with their favorite toys placed on top of the couch. This is a great exercise for balance and core strength
- Sitting balance: the child sits criss-cross on a balance disc while doing another activity. It is a great activity for core balance, strength, and body awareness.
- Sit to stand from step stool: This is a great leg strengthening activity as the child stands up from the sitting position.
- Stepping over obstacles: Balance is challenging for children with Noonan syndrome so it’s important to practice stepping over obstacles
- Crawling over pillows: Place 4-5 pillows in a row on the floor and have your child crawl across the pillows to reach a toy. This is a great overall strengthening and motor planning activity.
- Stair negotiation skills: This is so important to practice with children diagnosed with Noonan Syndrome. These children have a hard time alternating their feet on the stairs secondary to poor balance and short stature.
- Therapy ball: the child lies on their back over the ball and reaches back for something, and comes up to a sitting position
- Passive bicycle kicks while singing
- Standing or walking on different surfaces (barefoot on the hardwood floor, barefoot on pillows, barefoot on a balance disc, shoes on grass, shoes on wood chips at the playground).
- Lying on the back as you massage the bottom of their feet for proprioceptive input; which will help with independent walking and balance on the stairs.
- Joint Compressions: help in body awareness with independent standing/walking and balance on various surfaces.
In their study on perceived motor problems in daily life, Croonen et.al (2016); showed that people with NS reported particular problems related to pain, decreased muscle strength, fatigue, and clumsiness and their evident impact on functioning in their daily activities. Most people with NS believed that exercise, appropriate physiotherapy advice, and other supportive intervention are key elements to improved motor performance.[15]
Other names for this condition[edit | edit source]
- Familial Turner syndrome female pseudo-Turner syndrome
- Male Turner syndrome
- Noonan-Ehmke syndrome
- NS
- Pseudo-Ullrich-Turner syndrome
- Turner-like syndrome
- Turner phenotype with normal karyotype
- Turner syndrome in females with X chromosome
- Ullrich-Noonan syndrome.[16]
Prevention[edit | edit source]
There is no known way to prevent Noonan Syndrome because it occurs spontaneously, However, it is recommended that people with a history of this syndrome get genetic counseling before they have children. If Noonan syndrome is detected early, it's possible that ongoing and comprehensive care may lessen some of its complications such as heart disease.[4]
Prognosis[edit | edit source]
Noonan Syndrome is a lifelong condition. People with NS are differently affected and therefore their life expectancy will depend on the presence and severity of congenital heart defects.[17]
References[edit | edit source]
- ↑ 1.0 1.1 Noonan Syndrome: Practice Essentials. Available from:https://emedicine.medscape.com/article/947504-overview#a4 ( accessed 14 September, 2020)
- ↑ Noonan Syndrome: What Physicians need to know. Available from:https://www.medscape.org/viewarticle/563459 (accessed 15 September, 2020)
- ↑ 3.0 3.1 Noonan Syndrome. Available from https://www.stjude.org/disease/noonan-syndrome.html ( accessed 22 September, 2020)
- ↑ 4.0 4.1 4.2 Noonan Syndrome. Available from:https://www.mayoclinic.org/diseases-conditions/noonan-syndrome/symptoms-causes/syc-20354422 ( accessed 15 September, 2020)
- ↑ 5.0 5.1 Bhambhani V, Muenke M. Noonan syndrome. Am Fam Physician. 2014; 89(1):37-43.
- ↑ Van der Burgt I. Noonan syndrome. Orphanet journal of rare diseases. 2007 Dec;2(1):1-6.
- ↑ 7.0 7.1 Allanson JE, AE R. Noonan Syndrome. 2001 Nov 15 [Updated 2011 Aug 4]. GeneReviews™[Internet]. Seattle (WA): University of Washington, Seattle. 1993.
- ↑ Tomislav Meštrović P. Noonan Syndrome Diagnosis [Internet]. News-Medical.net. 2020 [cited 25 September 2020]. Available from: https://www.news-medical.net/health/Noonan-Syndrome-Diagnosis.aspx
- ↑ Noonan syndrome. Available from: https://www.nhs.uk/conditions/noonan-syndrome/diagnosis/#:~:text=You%20may%20be%20referred%20to,t%20rule%20out%20Noonan%20syndrome.( accessed 16 September, 2020)
- ↑ Noonan Syndrome - Genetics Home Reference. U.S National Library of Medicine. Available from: https://ghr.nlm.nih.gov/condition/noonan-syndrome#sourcesforpage (accessed 19 September, 2020)
- ↑ Allanson, JE. Noonan Syndrome. Journal of Medical Genetics,1987, 4: 9-13
- ↑ Tafazoli A, Eshraghi P, Koleti ZK, Abbaszadegan M. Noonan syndrome - a new survey. Arch Med Sci. 2017;13:215–222. doi: 10.5114/aoms.2017.64720. Published online 2016 Dec 19.
- ↑ 13.0 13.1 Noonan syndrome - Treatment [Internet]. nhs.uk. 2020 [cited 25 September 2020]. Available from: https://www.nhs.uk/conditions/noonan-syndrome/treatment/
- ↑ 4. [Internet]. Bigleapsct.com. 2020 [cited 25 September 2020]. Available from: https://www.bigleapsct.com/single-post/2016/05/16/Noonan-Syndrome
- ↑ Croonen EA, Harmsen M, Van der Burgt I, Draaisma JM, Noordam K, Essink M, Nijhuis‐van der Sanden MW. Perceived motor problems in daily life: Focus group interviews with people with Noonan syndrome and their relatives. American Journal of Medical Genetics Part A. 2016 Sep;170(9):2349-56.
- ↑ Bigleapsct.com. 2020 [cited 20 September 2020]. Available from: https://www.bigleapsct.com/single-post/2016/05/16/Noonan-Syndrome
- ↑ Noonan Syndrome. Available from:https://rarediseases.info.nih.gov/diseases/10955/noonan-syndrome ( Accessed 28 September, 2020)
- ↑ Noonan Foundation. Overview of the genetics of Noonan syndrome. Available from: http://www.youtube.com/watch?v=28ID5WP2lAw&t=327s [last accessed 3/10/2020]
- ↑ The Traveling Awareness Bears. Noonan Syyndrome Awarenenss. Available from: http://www.youtube.com/watch?v=Ctp6Msz3Kgc [last accessed 3/10/2020]