Bennett's fracture: Difference between revisions
(Created page with "{{subst:VUB}}") |
(added category) |
||
| (34 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Annelies Noppe|Annelies Noppe]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
'''Original | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div | |||
== Definition/Description == | == Definition/Description == | ||
[[File:Bennett-Fracture.jpg|right|frameless|643x643px]] | |||
<br>A Bennett fracture is a [[fracture]] of the base of the thumb resulting from forced abduction of the first metacarpal. It is defined as an intra-articular two-part fracture of the base of the first metacarpal bone.<ref name=":1">Radiopedia [https://radiopaedia.org/articles/bennett-fracture Bennett Fracture] Available from:https://radiopaedia.org/articles/bennett-fracture (last accessed 21.3.2020)</ref> | |||
* Despite a relatively simple appearance on [[X-Rays|radiographs]], Bennett fractures are considered unstable. | |||
* In evaluating and treating these fractures positioning the patient with thumb extension (hitchhikers position) should be avoided as this will cause further fracture displacement. | |||
* If there is a good alignment of the fracture fragments at postsurgical fixation, clinical outcomes are generally good.<ref name=":2">Carter KR, Nallamothu SV. [https://www.ncbi.nlm.nih.gov/books/NBK500035/ Bennett Fracture]. InStatPearls [Internet] 2019 May 18. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK500035/ (last accessed 21.3.2020)</ref> | |||
* Named after '''Edward Hallaran Bennett''' (1837-1907), a surgeon from Dublin, Ireland.<ref name=":1" /> | |||
=== Clinically Relevant Anatomy and Pathophysiology === | |||
[[File:Hand bones Ro 2.jpeg|right|frameless|400x400px]] | |||
== Clinically Relevant Anatomy | <br>The first CMCJ is unique, it has only articulation between the [[trapezium]] and the base of the first [[Metacarpal Fractures|metacarpal]]. | ||
* The articulation is saddle-shaped which allows greater motion. <ref name=":0">C. Brownlie. Bennett Fracture Dislocation: Review and Management; Australian Family Physician vol 40, No. 6, June 2011</ref> | |||
* The [[Ligament|ligaments]] in this joint are the anterior (volar) and posterior oblique ligaments, the anterior and posterior intermetacarpal ligaments, and the dorsal radial ligament. | |||
* The anterior oblique ligament is the most important for stability in the carpometacarpal joint.<ref>Mark E Baratz, MD; Chief editor: Harris Gellman, Bennett Fracture, Medscap reference http://emedicine.medscape.com/article/1238036-overview#a05<nowiki/>(Accessed 5/05/2013)</ref> | |||
= | The fracture pattern is distinct. | ||
* The base of the first metacarpal is fractured with an intraarticular extension due to the palmar ulnar fragment of the first metacarpal held in place by its ligamentous attachment to the trapezium (anterior oblique ligament) during the axial loading with the rest of the metacarpal moving in the opposite direction and the main fracture line occurring along with this point of weakness. | |||
* Due to this fracture, the first metacarpal shaft subluxes dorsally, proximally, and radially due to the pull of the [[Abductor pollicis longus|abductor pollicis longus,]] extensor pollicis longus, [[Extensor Pollicis Brevis|extensor pollicis brevis]], and the adductor pollicus brevis, which remain attached to the fracture fragment.<ref name=":2" /><br> | |||
= | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
<br>Other common injuries involving the first metacarpal include Rolando fractures, extra-articular fractures and [http://orthopedics.about.com/cs/handcondiitions/a/gamekeepers.htm gamekeepers thumb] | |||
The first differentiation clue can be found during the inspection/palpation of the location of the injury. Bennett fractures are associated with pain and weakness of the pinch grasp and swelling and ecchymosis over the carpal metacarpal joint of the thumb. The patient will be <u>unable to perform</u> functional tasks such as tying a shoe or using a key. Possible complications can be an infection, malunion or nonunion, arthritis and stiffness with contracture.<ref>KJAER-PETERSEN K. et al.; “Bennett’s fracture”, Journal of Hand Surgery, 1990 Feb; 15(1):58-61</ref><sup></sup><br> | |||
== Examination == | == Examination == | ||
If a Bennett fracture is suspected, the subjective history of the patient should include trauma to the hand or thumb followed by immediate pain and swelling or ischemia.<ref>HOWARD FM.; “Fractures of the basal joint of the thumb”, Clinical Orthopaedics and Related Research, 1987 Jul;(220):46-51</ref> The most common mechanism of injury is an axial force (compression) applied to the thumb whilst in flexion. | |||
On physical examination Bennett's fracture of the first carpometacarpal joint may present with: | |||
* visible deformity if the fracture is displaced | |||
* pain and swelling +/- ecchymosis over carpo metacarpal joint of the thumb | |||
* tenderness to touch | |||
* warmth over the area in acute phase | |||
* decreased pinch grasp and decreased grip strength<sup>13 </sup> | |||
== | Although [[X-Rays|X-ray]] films can be used to diagnose this condition, a [[CT Scans|CT scan]] should be ordered to evaluate the extent of the damage. On these CT scans a Bennett fracture will present can as an intra-articular fracture and dislocation of base of the first metacarpal. Even though there is a dislocation there should still be a small fragment of the first metacarpal that continues to articulate with trapezium. | ||
== Medical Management == | |||
Non-operative treatment in a thumb spica cast for 3-4 weeks can be considered in stable, non-displaced fractures. | |||
Operative treatment is recommended for unstable fracture patterns and intra-articular displacement of >1 mm. While open reduction and internal fixation with a screw or K-wire are both common practice, screws are often preferred as K-wires must be removed after union. | |||
The treatment algorithm is also influenced by the age and profession/hobbies of the patient. | |||
= | Untreated or malreduced fractures can lead to secondary [[Wrist and Hand Osteoarthritis|osteoarthritis]]. Osteoarthritis or malunion can cause significant pain and functional decline.<ref name=":1" /><sup></sup><sup></sup><sup></sup> | ||
=== Physical Therapy Management === | |||
[[File:Wrist Exercise Handout.jpg|right|frameless]] | |||
Generally, hand fractures are treated by immobilization with a cast or splint regardless of whether surgical or conservative treatment was required. | |||
= | Physical therapists and / or occupational therapists are usually heavily involved in creating and adapting these in consultation with the treating team or surgeon. | ||
* Protocols for rehabilitation must be based upon stability of the fracture and fracture management (operative or nonoperative). | |||
* Following the immobilisation period, physiotherapists and specialist hand therapists are involved in the facilitation of restoring maximal function to the hand<ref>Dell, P. C., and R. B. Dell. "Management of Carpal Fractures and Dislocations." Hunter - Mackin - Callahan Rehabilitation of the Hand and Upper Extremity. Eds. E. J. Mackin, et al. 5th ed. Philadelphia: Mosby, Inc.,2002. 1171-1184.</ref>. | |||
* The range of motion exercises may begin 5 to 10 days post screw fixation and after four weeks after pinning (after the pins are removed).<ref name=":2" /> | |||
* <sup></sup>Modalities employed include [[cryotherapy]], joint mobilisation, strengthening & flexibility exercises, [[Dexterity Tests|dexterity]] re-education and specific education. | |||
* Exercise intensity and complexity should be progressed appropriately following designated protocol usually provided by the surgeon.<ref>MDGuidelines.com, Return to work is the best measure of healthcare outcomes. www.mdguidelines.com/fracture-fingers-and-thumb (Accessed 5/05/2013)</ref><ref>Joe Godges, “Physical Therapy Protocols for Conditions of Wrist and Hand Region”, KP So Cal Ortho PT Residency , 2004</ref> | |||
* Evidence supports the positive impact of early physiotherapy intervention to facilitate optimal return to function and return to work/sport in hand fractures.<ref>Feehan, L. M., and K. Bassett. "Is There Evidence for Early Mobilization Following an Extraarticular Hand Fracture." Journal of Hand Therapy 24 Nov. 2008</ref> | |||
== Conclusion == | |||
The management of Bennet fracture is complex and best done with an interprofessional team that includes a hand surgeon/orthopedic surgeon, specialty care nurse, and physical therapist. | |||
When the fracture is encountered by the emergency department physician and nurse practitioner, it is important to refer the patient promptly to a hand surgeon. | |||
Poorly treated bennet fracture has very high morbidity. Even after adequate treatment, extensive rehabilitation is required. | |||
The outcomes for Bennet fracture are guarded | |||
== References == | |||
<references /> | <references /> | ||
[[Category: | [[Category:Primary Contact]] | ||
[[Category:Conditions]] | |||
[[Category:Fractures]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
Latest revision as of 17:27, 1 July 2020
Definition/Description[edit | edit source]
A Bennett fracture is a fracture of the base of the thumb resulting from forced abduction of the first metacarpal. It is defined as an intra-articular two-part fracture of the base of the first metacarpal bone.[1]
- Despite a relatively simple appearance on radiographs, Bennett fractures are considered unstable.
- In evaluating and treating these fractures positioning the patient with thumb extension (hitchhikers position) should be avoided as this will cause further fracture displacement.
- If there is a good alignment of the fracture fragments at postsurgical fixation, clinical outcomes are generally good.[2]
- Named after Edward Hallaran Bennett (1837-1907), a surgeon from Dublin, Ireland.[1]
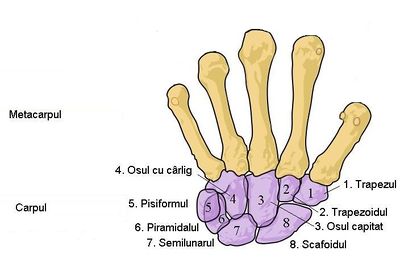
Clinically Relevant Anatomy and Pathophysiology[edit | edit source]
The first CMCJ is unique, it has only articulation between the trapezium and the base of the first metacarpal.
- The articulation is saddle-shaped which allows greater motion. [3]
- The ligaments in this joint are the anterior (volar) and posterior oblique ligaments, the anterior and posterior intermetacarpal ligaments, and the dorsal radial ligament.
- The anterior oblique ligament is the most important for stability in the carpometacarpal joint.[4]
The fracture pattern is distinct.
- The base of the first metacarpal is fractured with an intraarticular extension due to the palmar ulnar fragment of the first metacarpal held in place by its ligamentous attachment to the trapezium (anterior oblique ligament) during the axial loading with the rest of the metacarpal moving in the opposite direction and the main fracture line occurring along with this point of weakness.
- Due to this fracture, the first metacarpal shaft subluxes dorsally, proximally, and radially due to the pull of the abductor pollicis longus, extensor pollicis longus, extensor pollicis brevis, and the adductor pollicus brevis, which remain attached to the fracture fragment.[2]
Differential Diagnosis[edit | edit source]
Other common injuries involving the first metacarpal include Rolando fractures, extra-articular fractures and gamekeepers thumb
The first differentiation clue can be found during the inspection/palpation of the location of the injury. Bennett fractures are associated with pain and weakness of the pinch grasp and swelling and ecchymosis over the carpal metacarpal joint of the thumb. The patient will be unable to perform functional tasks such as tying a shoe or using a key. Possible complications can be an infection, malunion or nonunion, arthritis and stiffness with contracture.[5]
Examination[edit | edit source]
If a Bennett fracture is suspected, the subjective history of the patient should include trauma to the hand or thumb followed by immediate pain and swelling or ischemia.[6] The most common mechanism of injury is an axial force (compression) applied to the thumb whilst in flexion.
On physical examination Bennett's fracture of the first carpometacarpal joint may present with:
- visible deformity if the fracture is displaced
- pain and swelling +/- ecchymosis over carpo metacarpal joint of the thumb
- tenderness to touch
- warmth over the area in acute phase
- decreased pinch grasp and decreased grip strength13
Although X-ray films can be used to diagnose this condition, a CT scan should be ordered to evaluate the extent of the damage. On these CT scans a Bennett fracture will present can as an intra-articular fracture and dislocation of base of the first metacarpal. Even though there is a dislocation there should still be a small fragment of the first metacarpal that continues to articulate with trapezium.
Medical Management[edit | edit source]
Non-operative treatment in a thumb spica cast for 3-4 weeks can be considered in stable, non-displaced fractures.
Operative treatment is recommended for unstable fracture patterns and intra-articular displacement of >1 mm. While open reduction and internal fixation with a screw or K-wire are both common practice, screws are often preferred as K-wires must be removed after union.
The treatment algorithm is also influenced by the age and profession/hobbies of the patient.
Untreated or malreduced fractures can lead to secondary osteoarthritis. Osteoarthritis or malunion can cause significant pain and functional decline.[1]
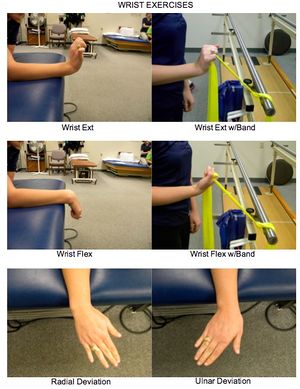
Physical Therapy Management[edit | edit source]
Generally, hand fractures are treated by immobilization with a cast or splint regardless of whether surgical or conservative treatment was required.
Physical therapists and / or occupational therapists are usually heavily involved in creating and adapting these in consultation with the treating team or surgeon.
- Protocols for rehabilitation must be based upon stability of the fracture and fracture management (operative or nonoperative).
- Following the immobilisation period, physiotherapists and specialist hand therapists are involved in the facilitation of restoring maximal function to the hand[7].
- The range of motion exercises may begin 5 to 10 days post screw fixation and after four weeks after pinning (after the pins are removed).[2]
- Modalities employed include cryotherapy, joint mobilisation, strengthening & flexibility exercises, dexterity re-education and specific education.
- Exercise intensity and complexity should be progressed appropriately following designated protocol usually provided by the surgeon.[8][9]
- Evidence supports the positive impact of early physiotherapy intervention to facilitate optimal return to function and return to work/sport in hand fractures.[10]
Conclusion[edit | edit source]
The management of Bennet fracture is complex and best done with an interprofessional team that includes a hand surgeon/orthopedic surgeon, specialty care nurse, and physical therapist.
When the fracture is encountered by the emergency department physician and nurse practitioner, it is important to refer the patient promptly to a hand surgeon.
Poorly treated bennet fracture has very high morbidity. Even after adequate treatment, extensive rehabilitation is required.
The outcomes for Bennet fracture are guarded
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Radiopedia Bennett Fracture Available from:https://radiopaedia.org/articles/bennett-fracture (last accessed 21.3.2020)
- ↑ 2.0 2.1 2.2 Carter KR, Nallamothu SV. Bennett Fracture. InStatPearls [Internet] 2019 May 18. StatPearls Publishing. Available from:https://www.ncbi.nlm.nih.gov/books/NBK500035/ (last accessed 21.3.2020)
- ↑ C. Brownlie. Bennett Fracture Dislocation: Review and Management; Australian Family Physician vol 40, No. 6, June 2011
- ↑ Mark E Baratz, MD; Chief editor: Harris Gellman, Bennett Fracture, Medscap reference http://emedicine.medscape.com/article/1238036-overview#a05(Accessed 5/05/2013)
- ↑ KJAER-PETERSEN K. et al.; “Bennett’s fracture”, Journal of Hand Surgery, 1990 Feb; 15(1):58-61
- ↑ HOWARD FM.; “Fractures of the basal joint of the thumb”, Clinical Orthopaedics and Related Research, 1987 Jul;(220):46-51
- ↑ Dell, P. C., and R. B. Dell. "Management of Carpal Fractures and Dislocations." Hunter - Mackin - Callahan Rehabilitation of the Hand and Upper Extremity. Eds. E. J. Mackin, et al. 5th ed. Philadelphia: Mosby, Inc.,2002. 1171-1184.
- ↑ MDGuidelines.com, Return to work is the best measure of healthcare outcomes. www.mdguidelines.com/fracture-fingers-and-thumb (Accessed 5/05/2013)
- ↑ Joe Godges, “Physical Therapy Protocols for Conditions of Wrist and Hand Region”, KP So Cal Ortho PT Residency , 2004
- ↑ Feehan, L. M., and K. Bassett. "Is There Evidence for Early Mobilization Following an Extraarticular Hand Fracture." Journal of Hand Therapy 24 Nov. 2008