Wheelchair Assessment - Physical Assessment
Original Editor - Naomi O'Reilly as part of the Wheelchair Service Provision Content Development Project
Top Contributors - Naomi O'Reilly, Rucha Gadgil, Tarina van der Stockt, Kim Jackson, Amrita Patro and Olajumoke Ogunleye
Introduction[edit | edit source]
The Physical Assessment, often referred to as the Mechanical Assessment Tool (MAT) is commonly used by seating clinicians as part of the seating assessment process. It is a form of biomechanical assessment and physical evaluation, forms the second part of the Wheelchair Assessment Process, and consists of three elements, with information from each of these assisting wheelchair service personnel to decide how much support the wheelchair user needs.
- Identifying the Presence, Risk of or History of Pressure Areas;
- Identifying Method of Propulsion;
- Assessment of Sitting Balance.
In most cases the physical assessment will also include a full musculoskeletal examination of the users range of motion, joint flexibility, muscle length, and skeletal alignment, with neurological issues such as tone and spasm pattern also noted as they affect posture and muscle length. It also incorporates a postural assessment of the user in their existing wheelchair, in supine, and sitting on a firm surface. Throughout the wheelchair assessment, the wheelchair service personnel should continuously observe the wheelchair user and their interactions with their equipment, and with the family member / caregiver including both physical and psychological interactions. [1]
Identifying the Presence, Risk of or History of Pressure Areas[edit | edit source]
A skin check is indicated if there is a history or risk of skin breakdown. Many sitting-acquired pressure areas develop against seating support surfaces such as the cushion and back support. A skin check for redness or evidence of skin damage is conducted in supine or side lying position to assess these sites. If a wheelchair user highlights that they have a pressure area, always ask to see it. Ensure this is done in a private area. [1]
A wheelchair user is at risk of developing a pressure area if they cannot feel or have other risk factors including:
- decreased sensation;
- decreased mobility and/or paralysis;
- moisture from sweat, water or incontinence;
- poor posture;
- previous or current pressure sore;
- poor diet and not drinking enough water;
- aging;
- weight (underweight or overweight).
| Skin Inspection | ||||||
|---|---|---|---|---|---|---|
| /// = Does Not Feel | Can Feel Normally? | Yes ☐ | No ☐ | |||
| O = Previous Pressure Sore | Previous Pressure Sore? | Yes ☐ | No ☐ | |||
| ✗ = Existing Pressure Sore | Current Pressure Sore? | Yes ☐ | No ☐ | |||
| If Yes, Is It An Open Sore? | Yes ☐ | No ☐ | ||||
| If Yes, What Stage? | 1 ☐ | 2 ☐ | 3 ☐ | 4 ☐ | ||
| Duration and Cause: | ||||||
| Is This Person at Risk * of developing a Pressure Sore? | Yes ☐ | No ☐ | ||||
| * A person who cannot feel or has 3 or more risk factors is at risk of pressure sores.
Risk Factors: Cannot Move, Moisture, Poor Posture, Previous / Current Pressure Sore, Poor Diet, Ageing, Under or Over Weight | ||||||
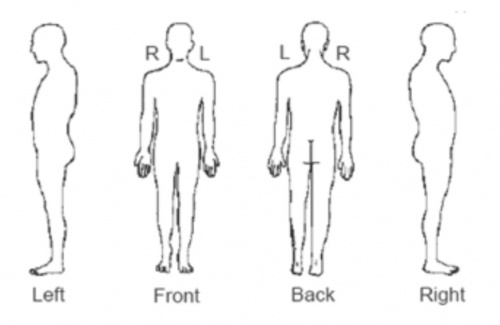
Mark on Body Diagram:
- Areas where the wheelchair user cannot feel; like this: ///
- Areas where the wheelchair user has had a pressure sore in the past; like this: O
- Areas where the wheelchair user has a current pressure sore; like this: ✗
Method of Propulsion[edit | edit source]
It is important to find out what method of propulsion the wheelchair user will use to push, as this can affect the choice of wheelchair and the way it is set up.
| Method of Propulsion | |||
|---|---|---|---|
| How Will the Wheelchair User Push Their Wheelchair? | Both Arms ☐ | Left Arm ☐ | Right Arm ☐ |
| Both Legs ☐ | Left Leg ☐ | Right Leg ☐ | |
| Pushed by a Helper ☐ | |||
| Comment: | |||
Assessment of Sitting Balance[edit | edit source]
The data should be gathered about the patient ‘s postural alignment at head, shoulder, trunk, pelvis and lower extremities using the visual observation and palpation skills. Assessment of Sitting Balance is completed to determine any additional postural support devices required through; [1]
- observation of sitting posture without support;
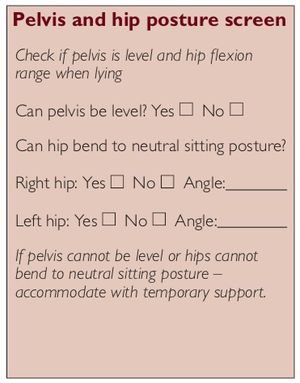
- completion of a pelvis and hip posture screen, which will identify how any problems around the pelvis or hips may affect the wheelchair user’s sitting posture; and
- carrying out hand simulation to ‘simulate’ the support that a wheelchair and additional postural supports may provide the wheelchair user;
Upright Sitting Posture[edit | edit source]
Not every wheelchair user can sit in an upright posture, even with support. Wheelchair users who have difficulty sitting upright will demonstrate a range of different sitting postures. The different postures are caused by part (or parts) of the body not being positioned in neutral. During the assessment, the wheelchair service personnel and wheelchair user need to find the most upright sitting posture the wheelchair user can safely and comfortably achieve and maintain without losing function. The wheelchair and PSDs should support this posture. There are three different final results that can be found when assessing posture which include: [1]
- Fixed Posture; The wheelchair user has a part of the body that is ‘fixed’. With gentle force there is no movement (strong force should never be used). Wheelchair service personnel should provide support to accommodate the non- neutral (fixed) posture
- Flexible to Neutral Posture; With gentle force the parts of the wheelchair user’s body that are not in neutral can be brought to neutral. In this situation the right support should be given to help the wheelchair user maintain a neutral sitting posture.
- Flexible Part way to Neutral Posture; With gentle force the parts of the wheelchair user’s body that are not in neutral can be moved only part way toward neutral. In this situation support is given to help the wheelchair user sit as close to neutral posture as is comfortable and functional for them.
A starting point for understanding the wheelchair user’s posture and what support may be needed is to observe his/her sitting posture – without support. For this part of the physical assessment the wheelchair user sits on an assessment bed. Make sure the wheelchair user is safe and that his/her feet are supported. Have an assistant or family member/caregiver sit with him/her if he/she cannot independently, sit safely. Observe whether the wheelchair user can sit in a neutral/upright sitting posture without support.
The purpose of observing sitting posture without support is to understand the wheelchair user’s postural tendency/habits. Observing sitting posture is a skill, which takes time and practice to develop.
Pelvis and Hip Posture Screen[edit | edit source]
Sitting posture is influenced by what is happening around the pelvis and the hips. In this part of the assessment wheelchair service personnel need to determine if the wheelchair user’s pelvis is level when viewed from the front, and whether the hips are able to bend to a neutral sitting posture (trunk to thigh angle is more than 90 degrees), with or without support.
If the pelvis is not level or the hips cannot bend to neutral sitting posture, the wheelchair service personnel need to consider whether the wheelchair user can sit in neutral posture with support or if not, how close to the neutral posture they can sit? If the wheelchair user cannot sit in a neutral sitting posture, it is also important to know if this is limited by a restriction either above the pelvis in the lumbar spine or below the pelvis in the hip joint.
In order for the wheelchair service personnel to answer all the questions above it is necessary to carry out a ‘pelvis and hip posture screen’ part of the assessment. This is not a full Range of Motion assessment but aims only to identify the factors noted above. You may choose to carry out a more extensive Range of Motion Assessment in order to gather more detailed information.
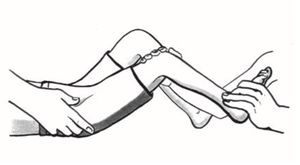
During the screen explain to the wheelchair user what you are going to do and why it is important; and ask the wheelchair user to lie down on their back on an assessment bed. Note: in these instructions, the person carrying out a pelvis and hip posture screen is called the ‘assessor’ and the person who assists the assessors is called ‘assistant’, who could be a co-worker, trained assistant, family member or caregiver. In order to conduct the Pelvis and Hip Posture Screen the wheelchair service personnel will need to be able to: [1]
- Locate bony landmarks of the pelvis
- Understand the structure of the wheelchair users skeleton and the influence of the various muscle groups on the articulation of the joints.
- Understand body planes and ranges of movement to identify fixed vs. flexible deformities.
Step 1 Pelvis Posture Screen[edit | edit source]
- assessor bends both the wheelchair user’s knees slightly and provides some support, which helps to relieve tension on the hips;
- assistant places their hands firmly on the wheelchair user’s trunk, around their lower ribs;
- assessor grips the pelvis gently with thumbs on the ASIS;
- assessor checks if thumbs/ASIS are level;
- if not level, assessor gently but firmly tries to align the pelvis so that both ASIS are level;
- assistant reports if he/she feels the trunk move, which means that there is some restriction to the movement;
- note how close to neutral/level it is possible to bring the pelvis;
- assessor records if the pelvis can be level on the intermediate wheelchair assessment form.
Step 2 Hip Posture Screen[edit | edit source]
- assistant gently but firmly holds the wheelchair user’s pelvis;
- assessor bends the leg that is not being tested slightly at the knee, resting the foot on the mat. This helps to reduce the tension in the hip being tested. This leg may need to be supported.
Step 3 Hip Posture Screen[edit | edit source]
- assessor gently moves the leg being tested into the neutral sitting posture;
- assistant reports if he/she feels the pelvis move, which means that there is some limit (restriction) to the movement;
- assessor feels how freely the hip joint can move;
- assessor repeats on the other side and compares;
- assessor records if right and left hip can bend to neutral sitting posture on the intermediate wheelchair assessment form.
Step 4 Hip Posture Screen[edit | edit source]
- assessor records how close to neutral posture each hip can reach with a goniometer with the help of an assistant;
- assessor places the pivot point of the goniometer on the hip joint. Assessor positions one arm of the goniometer along the thigh bone and one arm in line with the trunk;
- assessor holds the two arms together firmly;
- assessor records right and left hip angle degree measurements on the intermediate wheelchair assessment form. Assessor can also draw the angle of the goniometer on a separate piece of paper or on the back of the intermediate wheelchair assessment form.
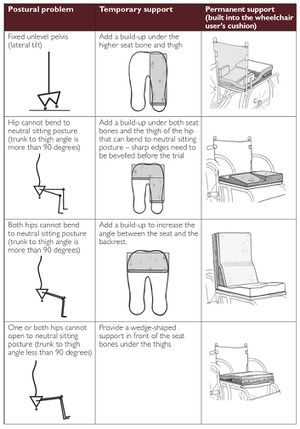
Consider temporary supports for a fixed unlevel pelvis and for the hips that cannot bend to neutral sitting posture. If the pelvis cannot be level or the hip cannot bend to a neutral sitting posture, it will need to be supported in the non-neutral posture in the final wheelchair. To continue the assessment, a temporary support should be made for the wheelchair user to sit on.
During an assessment, the temporary support will: allow the wheelchair user to sit with more stability and balance; stop the wheelchair user from compensating for the unlevel pelvis or hips that cannot bend to neutral sitting posture and allow the wheelchair service personnel to carry on the assessment and concentrate on the rest of the wheelchair user’s posture including pelvis, trunk, head, neck and legs.
A temporary support can be made of firm foam. The table below shows the different postural problems, temporary supports and possible permanent support for these problems. [1]Hand Simulation[edit | edit source]
Hand simulation helps to identify what support the wheelchair user needs. During the hand simulation, the wheelchair service personnel use their hands to determine if the wheelchair user sit in neutral posture with support and if not, then determine how close to the neutral posture they can sit in order to assess what support is needed and where. During a hand simulation, the wheelchair service personnel work with the wheelchair user and an assistant or family member/caregiver to provide support with hands. [1]
How to Carry Out the Hand Simulation[edit | edit source]
Important aspects to remember when carrying out a hand simulation are: explanation to the wheelchair user about what you are going to do and why. Ask the wheelchair user to sit on a firm but padded, flat surface. An assessment box is idea so the wheelchair service personnel and assistant or family member/ caregiver can easily provide support to the wheelchair user from the front, back and sides. If the wheelchair user cannot safely sit without support ask an assistant or family member/caregiver to support them. Ensure the wheelchair user’s feet are supported at the correct height for them. If the pelvis is unlevel or if one of the hips cannot bend to neutral sitting posture (trunk to thigh angle is more than 90 degrees), provide a temporary support as described above. [1]
It is often necessary to have more than one pair of hands when completing a Hand Simulation, so team work is key. Take help from the assistant, who could be a co-worker, trained assistant, family member or caregiver. Involving family members/caregiver will also help them to better understand the final Postural Support Device solution that is selected.
Communication is also vital, both with the wheelchair user and family member/caregiver. If the wheelchair user is non-verbal, ensure you find an appropriate method of communication with them so they can feedback to you in relation to how the changes feel. Remember to explain to the wheelchair user what you are doing at each step. Think carefully about what your hands are doing as they are providing the support that will later be provided by the wheelchair and postural support devices. Ensure you pay careful attention to; [1]
- where your hands are placed;
- the direction of force/support;
- how much force/support is being used;
- how much surface area your hands are covering (for example, are you using just one finger or a whole hand);
Always provide support at the pelvis first as the posture of the pelvis will affect the posture of the rest of the body. So if the wheelchair user’s pelvis is not in neutral, use your hands to encourage the pelvis towards neutral. When the pelvis has been supported, focus on other parts of the body in the following order:
- trunk/arms;
- head and neck;
- hips and thighs;
- lower legs.
Finally ensure you only make one change at a time and observe how the changes in one part of the body affect other parts, always getting feedback from the wheelchair user.
In order to begin hand simulation part of the physical assessment:
- kneel or squat in front of the wheelchair user;
- gently place hands on both sides of the wheelchair user’s pelvis;
- if the wheelchair user’s pelvis is not in neutral - use hands to bring the pelvis as close to neutral as is comfortable;
- do not use very strong force;
- find how close to neutral the pelvis can be supported;
- observe how moving the pelvis towards neutral affects the wheelchair user’s trunk, hips, head and neck.
- when the pelvis is supported as close to neutral as possible, the wheelchair service personnel can then consider what support is needed at the trunk;
- ask the assistant to hold the pelvis in the posture that you have identified as ‘as close to neutral as possible’ for this wheelchair user;
- explain carefully to the assistant where to hold and how to hold the pelvis. Check that he/she is able to do this before moving on.
Provide support at the trunk (if needed): As for the pelvis, if the wheelchair user’s trunk is not in neutral sitting posture, use your hands to provide support. Work in this order:
- stabilize the pelvis with your hands;
- straighten out the trunk so both shoulders are level (or as close to level as is possible) by providing support with your hands at both sides of the trunk;
- bring the trunk upright with head and neck balanced over the pelvis by providing support at the back and sometimes at the front with your hands;
- observe the contour of the pelvis and trunk from the side. This is important to plan the shape of the backrest to provide the best support.
Pay close attention to how trunk support affects the rest of the body. For example, does the trunk support help improve head and neck posture? Even with good pelvis and trunk support, some wheelchair users may find it hard to hold their head upright. Some suggestions to help improve head and neck posture are:
- allow the wheelchair user to recline slightly backwards;
- observe whether the wheelchair user is then able to better balance their head over their trunk;
- provide additional support for the arms.
During the hand simulation, ask the assistant supporting the pelvis if they feels any changes as you support the trunk. Remember to always ask the wheelchair user for their feedback.
Provide support for other body parts (if needed)
- Once the pelvis and trunk are supported in the most neutral sitting posture that is comfortable, check the posture of the head and neck, hips, thighs and lower legs.
- Use your hands to find out how close to neutral each body part can comfortably move. Continue to check how any change affects the rest of the body. Continue to ask the wheelchair user for their feedback.
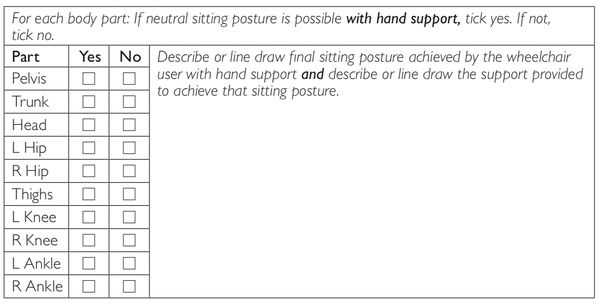
Recording the results from a hand simulation
Results of the hand simulation are recorded on the intermediate wheelchair assessment form. There is space to:
- record with a tick whether the wheelchair user is able to achieve a neutral sitting posture for each body part with hand support;
- describe or line draw the final sitting posture achieved by the wheelchair user with the hand support; and
- describe or line draw the support provided for the wheelchair user to achieve that sitting posture.
Resources[edit | edit source]
Assessment Forms[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Sarah Frost, Kylie Mines, Jamie Noon, Elsje Scheffler, and Rebecca Jackson Stoeckle. Wheelchair Service Training Package - Reference Manual for Participants - Intermediate Level. World Health Organization, Geneva. 2013
- ↑ CI. Spinal Seating - Finding Bony Landmarks in the Pelvis. Available from: https://vimeo.com/94479185[last accessed 06/07/18]
- ↑ Assistive Technology for All. WSTP Intermediate Video Series: 7. Pelvis and Hip Posture Screen. Available from: https://youtu.be/3gCM6G0nOok [last accessed 30/10/17]
- ↑ Assistive Technology for All. WSTP Intermediate Video Series: 9. Hand simulation demonstration - Deepak. Available from: https://youtu.be/jcq5S26bALg [last accessed 6/6/2018]
- ↑ Assistive Technology for All. WSTP Intermediate Video Series: 10. Hand simulation demonstration - Enith. Available from: https://youtu.be/jVC5un7zxxY[last accessed 15/07/18]
- ↑ Assistive Technology for All. WSTP Intermediate Video Series: 11. Hand Simulation Demonstration - Bahati. Available from: https://youtu.be/7QGWAATo86g[last accessed 30/06/18]