Total Knee Athroplasty Neuropathic Pain
Original Editor - Lucinda hampton
Top Contributors - Lucinda hampton
Introduction[edit | edit source]
Knee joint arthroplasty (KJA) procedures are regularly performed. Post-KJA neuropathy not common, usually requiring no intervention, resolving within 1 year. Post-TKA neuropathy most often affects those nerves at risk during surgery[1]. However up to 1/5 of these replacements cause patients to have a degree of chronic pain or are not satisfied with their surgery.
Neuropathic pain rates post KJA reach their max at six to twelve weeks after surgery, and approximately 6% patients will go on to have long term neuropathic pain.
- Post-surgical pain with a neuropathic component is likely to be greater than pure nociceptive pain, affecting QOL.
- Neuropathic pain may stem from sensitisation of peripheral nociceptors many sources eg inflamed synovium, damaged subchondral bone, surgery trauma.
- Patients with a pre existing neuropathic pain elsewhere have a greater potential for chronic nociceptor stimulation and central pain transmission.
Features[edit | edit source]
Neuropathic pain is distinguished by the following features: pain not relieved by rest and analgesia; diffuse and difficult to localise pain; pain that radiates towards or away from the knee; pain associated with feelings of pressure, numbness, sensitivity, burning, stinging, electric shocks or rigidity.
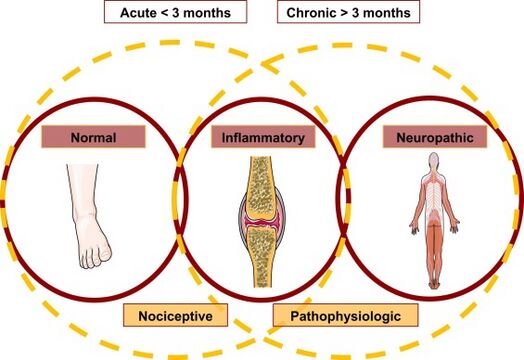
Image shows Venn diagram for type of pain and chronicity. Pain from a minor foot sprain considered normal and nociceptive, signaled by tissue injury (i.e., a normal mechanism). Inflammatory pain from eg arthritis (center) is a nociceptive mechanism because inflammation is the cause of pain. Inflammation is also pathophysiologic because it involves an altered (i.e., disease) state. NP is at the right, considered only as pathophysiologic because pain is elicited by abnormal pain mechanisms. Normal pain is only acute, whereas inflammatory or NP may be acute or chronic.
Assessing[edit | edit source]
Neuropathic pain can be assessed by various validated scoring systems, the most commonly used is the PainDETECT, a helpful assessment tool in this patient group. By identifying neuropathic pain components, treatment choices can be directed at targeting more specific pain mechanisms.
Various guidelines exist for the assessment and treatment of neuropathic pain. These include Neuropathic pain medication , such as:
- Amitriptyline, duloxetine, gabapentin or pregabalin as initial treatment.
- Capsaicin cream or topical lidocaine is an option for localised neuropathic pain or neuroma.[2]
Various factors have been identified as potential causal factors, including the "yellow flags", and include symptoms of depression, anxiety, and catastrophizing.[3]
References[edit | edit source]
- ↑ Speelziek SJ, Staff NP, Johnson RL, Sierra RJ, Laughlin RS. Clinical spectrum of neuropathy after primary total knee arthroplasty: A series of 54 cases. Muscle & nerve. 2019 Jun;59(6):679-82. Available:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6520178/ (accessed 4.4.2024)
- ↑ J.R.A.Phillips, N.Howellsand A.D.Toms,Pain after knee replacement, TheKnee, https://doi.org/10.1016/j. Available:https://www.thekneejournal.com/article/S0968-0160(20)30261-1/abstract (accessed 4.4.2024)
- ↑ Colovic D, Draschl A, Reinbacher P, Hecker A, Schittek G, Fischerauer SF, Leithner A, Klim SM, Koutp A, Wittig U, Brunnader K. Evaluation of Neuropathic Pain after Total Knee Arthroplasty: Do Yellow Flags Matter?. Journal of Clinical Medicine. 2023 Dec 15;12(24):7708.Available:https://pubmed.ncbi.nlm.nih.gov/38137778/ (accessed 4.4.2024)