Sleep and Menstrual Cycle
Original Editor - Ananya Bunglae Sudindar
Top Contributors - Ananya Bunglae Sudindar
Introduction[edit | edit source]
Sleep is an important human function. It plays a vital role in ensuring physical and mental well-being of a person. Beyond just providing rest, quality sleep is associated to the health of various body systems such as, cardiovascular health, renal function, immunity, and hormonal balance. [1][2]
In people who menstruate, it has been established that sleep and hormones have an intricate relationship. Hormonal fluctuations seen in the various phases of the menstrual cycle affect sleep and circadian rhythms. Additionally, it has also been well documented that poor sleep quality can disrupt hormonal health and correlate with menstrual disturbances. [3][4]
Menstrual Cycle Phases and Sleep[edit | edit source]
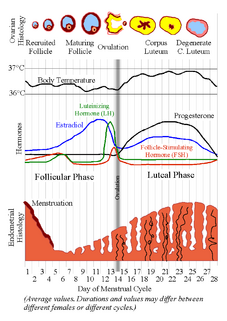
People who menstruate experience hormonal variations throughout their menstrual cycles. Based on these hormonal fluctuations the menstrual cycle is divided into the following phases:
- Menstrual phase
- Follicular phase
- Ovulation phase
- Luteal phase
In addition to reproductive functions, these hormonal variations throughout the cycles affect other body functions including sleep functions. [5] It is established that the menstrual cycle affects both sleep duration as well as sleep architecture. [6]
Influencing factors of sleep during the menstrual cycle[edit | edit source]
- Hormonal fluctuations: Fluctuations of the hormones oestrogen and progesterone during the menstrual cycle affects sleep. Studies show changes in REM and non-REM sleep patterns during the menstrual cycles are linked to fluctuations in hormones like oestrogen and progesterone. These hormones affect the types of sleep stages, impacting overall sleep quality. Increase in progesterone levels seen in the luteal phase result in the increase of body temperature making it difficult to fall asleep comfortably. Progesterone also impacts neurotransmitters such as serotonin and gamma-aminobutyric acid (GABA) which are crucial for regulating sleep and sleep quality.
- Pain and discomfort: Menstrual cramps, breast tenderness, headaches and general discomfort often seen in the menstrual phase and late luteal phase can impact the quality of sleep. This can result in difficulty falling asleep as well as disturbed sleep.
- Psychological and emotional factors: Stress, anxiety and mood fluctuations is often seen throughout the menstrual cycle which can impact sleep quality and lead to sleep disturbances. Increase in stress can lead to difficulty in falling asleep and maintaining sleep.
- In addition to the above factors, individualistic factors such as age, lifestyle diet, genetic factors and activity levels also influence sleep in people who menstruate.
Sleep disturbances in different phases of the menstrual cycle[edit | edit source]
Major sleep disturbances are observed in the menstrual, follicular and luteal phase.
Menstrual phase:
- Sleep disturbance in the menstrual phase is often individualistic and is influenced by specific symptoms experienced such as menstrual cramps, general body discomfort, headaches etc.
Follicular phase:
- Sleep continuity measures remain consistent in the follicular phase, indicating stable sleep patterns during this phase.
- Variable REM sleep is observed in the follicular phase, characterized by earlier onset and shorter episodes compared to other phases of the menstrual cycle.
- Subtle changes in sleep architecture are noted during the follicular phase, suggesting alterations in sleep stages.
Luteal phase:
- Some individuals who menstruate experience a reduction in sleep duration during the luteal phase compared to the follicular phase, possibly due to an increase in progesterone levels.
- Increased light sleep is observed during the luteal phase, indicating a shift in sleep stages.
- Decreased REM sleep is observed in the luteal phase, suggesting changes in REM sleep duration and quality.
- Decreased sleep efficiency is noted during the luteal phase, indicating more fragmented and disrupted sleep patterns during this phase.
Management of Sleep Disturbances During Menstruation[edit | edit source]
- Hormonal management: Hormonal management can be considered for individuals with irregular menstruation or increased hormonal fluctuation resulting in sleep disturbances. Hormonal therapy or contraceptives offer a potential solution to regulate hormonal fluctuations, enhancing sleep quality and overall health. The selection of hormonal intervention should be personalized, taking into account individual hormonal imbalances and health objectives.
- Lifestyle modification: Adding moderate physical activity, health diet, maintain regular sleep schedule and reduce daily stressors can help promote quality sleep.
- Sleep hygiene: Establishing proper sleep hygiene is essential for enhancing sleep quality across the menstrual cycle. This involves adhering to a regular sleep routine, ensuring a comfortable sleep environment, and avoiding stimulating activities before bedtime. These practices foster healthy sleep patterns and elevate overall sleep quality.
- Cognitive behavioural therapy: Cognitive behavioural therapy is an evidence based effective tool to help people with insomnia. It often includes adopting different strategies for better sleep quality.
Menstrual Disorders and Sleep[edit | edit source]
Studies have shown that there is a relationship between sleep and several menstrual disorders such as dysmenorrhea, irregular menstrual cycles, heavy bleeding, as well as several premenstrual syndrome (PMS) symptoms. People who menstruate who experience these challenges have reported sleep disturbances such as poor-quality sleep, daytime drowsiness, difficulty falling asleep and reduced sleep duration.
Although there is no established mechanism that links sleep disturbances with menstrual disorders or disturbances, poor quality of sleep that leads to irregular circadian rhythms has shown to impact menstrual health. Elevated levels of prostaglandins triggered by poor sleep can exacerbate menstrual disorders such as dysmenorrhea and heavy bleeding.
References[edit | edit source]
- ↑ Beroukhim G, Esencan E, Seifer DB. Impact of sleep patterns upon female neuroendocrinology and reproductive outcomes: a comprehensive review. Reproductive Biology and Endocrinology. 2022 Jan 18;20(1):16.
- ↑ Baranwal N, Phoebe KY, Siegel NS. Sleep physiology, pathophysiology, and sleep hygiene. Progress in cardiovascular diseases. 2023 Mar 1;77:59-69.
- ↑ Baker FC, Lee KA. Menstrual cycle effects on sleep. Sleep Medicine Clinics. 2022 Jun 1;17(2):283-94.
- ↑ Masuda H, Okada S. Menstruation-related symptoms are associated with physical activity and midpoint of sleep: a pilot study. Frontiers in Global Women's Health. 2023;4.
- ↑ 5.0 5.1 5.2 Baker FC, Lee KA. Menstrual cycle effects on sleep. Sleep Medicine Clinics. 2022 Jun 1;17(2):283-94.
- ↑ 6.0 6.1 6.2 Rugvedh P, Gundreddy P, Wandile B. The Menstrual Cycle’s Influence on Sleep Duration and Cardiovascular Health: A Comprehensive Review. Cureus. 2023 Oct 18;15(10).
- ↑ Meers J. Interaction of Sleep and Emotion across the Menstrual Cycle.
- ↑ Jeon B, Baek J. Menstrual disturbances and its association with sleep disturbances: a systematic review. BMC Women's Health. 2023 Sep 1;23(1):470.