Lesch-Nyhan Syndrome
Original Editor - User Name
Top Contributors - Pacifique Dusabeyezu, Kim Jackson, Kirenga Bamurange Liliane, Bruno Serra and Ines Musabyemariya
Introduction[edit | edit source]
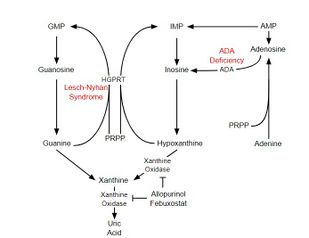
Lesch-Nyhan Syndrome (LNS) is a rare, inherited X-linked genetic disorder caused by a deficiency of the enzyme hypoxanthine-guanine phosphoribosyl transferase (HPRT),an enzyme of purine salvage pathway. The enzyme is responsible for recycling purines by converting guanine and hypoxanthine into guanosine monophosphate and inosine monophosphate, respectively. Lack of the enzyme causes an increase in guanine and hypoxanthine, which eventually gets converted into uric acid,[1] Uric acid levels are abnormally high in people with Lesch-Nyhan syndrome and sodium urate crystals may abnormally accumulate in the joints and kidneys.
LNS is inherited as an X-linked recessive genetic disorder that mostly affects males, with rare female exceptions.[2] Lesch-Nyhan syndrome was first described in 1964 by Lesch and Nyhan, when two brothers originally diagnosed with cerebral palsy were later recognized as living with a previously undescribed inherited metabolic disease because of the familial occurrence and unusual clinical features.[3]
Causes[edit | edit source]
Lesch-Nyhan Syndrome is an X-linked recessive disorder resulting from mutation of the HPRT1 gene, located at a q26-27 position on the long arm of the X chromosome. Though only a single gene is associated with this syndrome, over 600 mutations have been identified, each leading to varying levels of severity of clinical presentations making HPRT enzyme deficiency a spectrum rather than a single disease.[5] Males who receive the defective X chromosome from the carrier mothers manifest the disease. Females are mostly carriers but may develop the disease if the healthy X chromosome undergoes lionization, and the defective X chromosome is expressed phenotypically.
Signs and Symptoms[edit | edit source]
The lack of HPRT causes a build-up of uric acid in all body fluids, and leads to symptoms such as:
- Severe gout
- Poor muscle control
- Moderate developmental disabilities, which appear in the first year of life.
- Banging the head or limbs.[6]
- Poking the eyes.
Other common symptoms include muscle control problems such as:
- Constant repetitive movement of the arms or legs (ballismus).
- Difficulty crawling, walking or feeding with hands.
- Difficulty swallowing (dysphagia).
- Exaggerated reflexes (hyperreflexia).
- Arched back due to muscle spasms (opisthotonos).
- Involuntary movements (dystonia) or facial expressions.
- Involuntary twitching, wiggling or writhing (choreoathetosis).
- Jerking movements (chorea).
- Muscles that stiffen or tighten, preventing movement (spasticity).
- Slurred or slow speech (dysarthria).
That increase in uric acids causes them to appear normal when they are born, but by about the third month they are unable to lift their heads or sit up. They display hypotonia, a lack of muscle tone, and many also suffer from dystonia, a lack of motor control. Clinically, LNS is characterized by mental retardation, choreoathetosis(Involuntary writhing), spastic cerebral palsy, and aggressive self-mutilating behaviors,[7]like biting lips, fingers, cheeks.(Dermatophagia)[8]
Other neurological sign and symptoms in people with LNS includes the following:
- Facial grimacing
- Repetitive movements of the arms and legs similar to Huntington's disease
The absence of HGPRT enzyme is the cause of hyperuricemia in LNS patients. As a result, orange deposits also known as "orange sand" can sometimes be seen the diapers of infants as the first manifestation of LNS which when present can contribute to the early diagnosis and management before the progression of manifestations.
Epidemiology[edit | edit source]
The prevalence of Lesch-Nyhan Syndrome has been estimated to be between 1:235,000 and 1:380,000.[9]Although it is an X-linked genetic disorder manifesting mostly in males, a few females with LNS have been reported and studies show that it occurs in relatively equal frequencies in all populations.
Diagnosis[edit | edit source]
The diagnosis of Lesch-Nyhan Syndrome (LNS) typically involves a combination of clinical evaluation, laboratory tests, and genetic testing. [10]
- Clinical examination: Medical history and physical examination can be done by healthcare providers to look for characteristic signs and symptoms associated with LNS, such as neurological abnormalities, self-injurious behavior, developmental delays, and the presence of uric acid crystals in urine.
- Genetic testing: This is the definitive method of confirming LNS diagnosis. The HPRT gene (HPRT1)is analyzed for mutations or deletions. This can be done through various techniques such as DNA sequencing or molecular genetic testing. This can also help in identifying the carriers of LNS genes in the family.[1]
- Enzyme analysis: Enzymatic assay or molecular testing can be used to diagnose LNS. Enzymatic diagnosis is an estimate of HPRT enzyme activity in erythrocyte lysate.[1] Since LNS is due to the deficiency of this enzyme, low or no HPRT activity supports the diagnosis.
- Blood tests: Blood samples can be used to measure uric acid, hypoxanthine, and guanine levels. LNS patients usually have a significantly elevated level of urinary acid in the blood.
- Prenatal(before birth) testing in case the pregnant woman has taken an ultrasound scan and found that she will be giving birth to a male baby. In that case, amniocentesis can be done before birth at 14 to 15 weeks of gestation.[11][12]
Complications[edit | edit source]
- Nephrolithiasis(Kidney and bladder stones)
- Gout
- Kidney failure
- Megaloblastic anemia due to a lack of vitamin B12.
- Repeated vomiting.
- Learning issues
Differential diagnosis[edit | edit source]
Many conditions have symptoms that resemble Lesch-Nyhan syndrome. For example, autism spectrum disorder and cerebral palsy both have similarities to LNS. Getting an accurate diagnosis is important, so your child can receive the appropriate care for their needs.
Other conditions similar to Lesch-Nyhan syndrome include:
Management/ Interventions[edit | edit source]
Managing Lesch-Nyhan syndrome (LNS) involves a multidisciplinary approach to address the various symptoms and complications associated with the condition. As there is currently no cure for LNS, treatment aims to improve the quality of life for the affected individuals and provide support for their families.[13]
Medical and Pharmacological management[edit | edit source]
As there is no cure for LNS , there are ways to help improve the individual’s quality of life[13] and the treatment aims to alleviate symptoms and prevent complications. These include using medications such as allopurinol in the management of hyperuricemia which prevents renal and musculoskeletal complications, allopurinol inhibits the xanthine oxidase enzyme and blocks the conversion of xanthine and hypoxanthine into uric acid, which prevents uric acid crystalluria, renal lithiasis and gouty arthrosis.[14]
Neurological dysfunctions are not totally comprehended, thus, there are no effective treatments for them. Benzodiazepines and gamma-aminobutyric acid (GABA) inhibitors, such as baclofen or other muscle relaxants might be used to treat dystonia and spasticity.[14] The anxiety of patients with LNS can be treated with the use of antipsychotic medications like Benzodiazepines which inhibit the reuptake of serotonin and may be prescribed under the guidance of a specialist.[14]
Depending on the severity of motor symptoms, assistive devices like braces, splints, or mobility aids may be recommended to improve mobility and independence. The use of special devices to restrict the movement of limbs and to avoid mutilating lesions and programs for posture correction to prevent deformities are complementary alternative therapies.[14]
Nutritional management[edit | edit source]
There are no dietary restrictions for people with LNS . Some nutritionists recommend a "low purine" diet including fruits and vegetables, but there is no evidence that the diet has any important influence on the condition. Some individuals with LNS has trouble of swallowing, and some have trouble with frequent vomiting. If there is trouble with swallowing, the food must be cut into small pieces or made into a soft consistency.[15]
Physiotherapy management[edit | edit source]
Although physiotherapy cannot directly address the cause of the disease, it can help to manage symptoms and improve the quality of life of people with LNS. The physiotherapy interventions for individuals with LNS varies depending on the individual's unique needs, age, functional abilities and symptoms severity. The following are potential physiotherapy interventions in individuals with LNS:
- Range of motion exercises: LNS is associated with stiffness of joints and limited mobility. Physiotherapists can design stretching and movement exercises by targeting all major joints that are generally affected in individuals with LNS in order to maintain the flexibility of the joints and prevent contractures.[16]
- Balance and coordination training: Individuals with LNS may experience challenges with balance and coordination. This should be achieved by improving these skills through various balance, coordination exercises and proprioceptive training. The exercise program should involve walking on one leg, walking straight, or using a balance board.
- Assistive devices: Depending on the individual's needs and level of mobility, physiotherapists can recommend and provide guidance on using assistive devices such as orthotics, walking aids and devices to maintain posture and help prevent deformities.[16]
- Managing pain: Musculoskeletal pain is highly associated in individuals with LNS. The pain experienced by these individuals may be linked to factors such as dystonia, spasticity or even joint stiffness. Pain management techniques such as heat or cold therapy, transcutaneous electrical nerve stimulation (TENS), passive stretching or gentle manual therapy to alleviate discomfort and improve overall well-being can be applied.
- Caregiver and patient education: Training persons with LNS and their caregivers on appropriate techniques and strategies to manage physical symptoms can help them to optimize their functions. This includes guidance on exercise, positioning, safe transport, and handling techniques to ensure that the environment for individuals is safe and supportive.
Prognosis[edit | edit source]
The outlook of individuals with Lesch-Nyhan syndrome is generally poor. They usually cannot walk and require a wheelchair. Most have short lifespans, rarely living more than 20 years due to disease complications. A care team can help you and your child manage symptoms so your child can be as comfortable and active as possible.[16]Case reports have documented sudden unexpected death in some patients.[17]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Fu R, Sutcliffe D, Zhao H, Huang X, Schretlen DJ, Benkovic S, Jinnah HA. Clinical severity in Lesch-Nyhan disease: the role of residual enzyme and compensatory pathways. Mol Genet Metab. 2015,114(1):55-61.
- ↑ Lesch-Nyhan Syndrome [Internet]. 2023 [cited 2023 Jul 8]. Available from: https://www.ninds.nih.gov/health-information/disorders/lesch-nyhan-syndrome#
- ↑ Lesch M, Nyhan WL. A familial disorder of uric acid metabolism and central nervous system function. Am J Med. 1964;36:561-570.
- ↑ Animated biology With Arpan. Lesch-Nyhan syndrome | What are the symptoms of Lesch-Nyhan syndrome? | Treatment options | USMLE. Available from: https://www.youtube.com/watch?v=7FbM5VtKWz0 [last accessed 24/6/2023]
- ↑ Fu R, Ceballos-Picot I, Torres RJ, Larovere LE, Yamada Y, Nguyen KV, Hegde M, Visser JE, Schretlen DJ, Nyhan WL, Puig JG, O'Neill PJ, Jinnah HA., Lesch-Nyhan Disease International Study Group. Genotype-phenotype correlations in neurogenetics: Lesch-Nyhan disease as a model disorder. Brain. 2014:1282-303.
- ↑ Pozzi M, Piccinini L, Gallo M, Motta F, Radice S, Clementi E. Treatment of motor and behavioural symptoms in three Lesch-Nyhan patients with intrathecal baclofen. 2014;9–12.
- ↑ Jathar P, Panse AM, Jathar M, Gawali PN. Lesch-Nyhan Syndrome: Disorder of Self-mutilating Behavior. Int J Clin Pediatr Dent 2016;9(2):139-142.
- ↑ Cohen PR. Skin Biter: Dermatodaxia Revisited. Cureus. 2022;14(2):1–7.
- ↑ Jinnah HA, Ceballos-Picot I, Torres RJ, et al. Attenuated variants of Lesch-Nyhan disease. Brain 2010;133:671–89
- ↑ Jinnah HA, Ceballos-Picot I, Torres RJ, et al. Lesch–Nyhan Disease international study group. Attenuated variants of Lesch–Nyhan disease. Brain. 2010;133:671–89.
- ↑ Nyhan WL, Vuong LUC, Broock R. Prenatal diagnosis of Lesch-Nyhan disease. Prenat Diagn. 2003;23(10):807–9.
- ↑ Evans J, Sirikumara BM, Gregory M, Eng F, Ed F, Newport C, et al. Lesch-Nyhan syndrome and the lower lip guard. 1993;437–40.
- ↑ 13.0 13.1 Cleveland clinic. Lesch-Nyhan Syndrome [Internet]. 2022 [cited 2023 Aug 7]. Available from: https://my.clevelandclinic.org/health/diseases/23493-lesch-nyhan-syndrome
- ↑ 14.0 14.1 14.2 14.3 Campolo González A, Díaz AV, Riesco DF, Chávez MH. Oral self-mutilation in Lesch-Nyhan Syndrome. Case Report. Rev Chil Pediatr. 2018;89(1):86–90.
- ↑ Seaworld. Diet and eating habits [Internet]. Lesch-nyhan organization. 2019. Available from: https://seaworld.org/animals/all-about/elephants/diet/
- ↑ 16.0 16.1 16.2 Nanagiri A, Shabbir N. Lesch-Nyhan Syndrome. [Updated 2023 Apr 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK556079/
- ↑ Neychev VK, Jinnah HA. Sudden death in Lesch-Nyhan disease. Dev Med Child Neurol. 2006;48(11):923–6.