Introduction to Gunshot Injury Rehabilitation
Original Editor - Zafer Altunbezel
Top Contributors - Ewa Jaraczewska and Jess Bell
Introduction[edit | edit source]
Gunshot injuries are one of the most common injury patterns in conflict settings, with civilians becoming more vulnerable in 21st-century armed conflicts. Gunshot injuries are high-energy injuries which can cause significant tissue damage, paralysis or death. The extent of the injury depends on a number of factors. Rehabilitation professionals should have an understanding of the potential consequences and appropriate management strategies throughout each phase of rehabilitation to enhance patient outcomes.
Definition of Gunshot Injury[edit | edit source]
A gunshot injury is "the penetrating injury and its related consequences caused by a projectile from a firearm."[1]
Epidemiology[edit | edit source]
The epidemiology of gunshot injuries is difficult to assess, and it varies based on the population, conflict set, country, characteristics of the conflict, and time it occurred:[1]
- Wild et al. aimed to describe "conflict-related injuries sustained by civilians and local combatants in twenty-first century conflict".[2] They found that:[2]
- gunshot injuries caused 22% of injuries in civilians and local combatants
- gunshot injuries are the second most common mechanism of injury among US military personnel during armed conflict, causing 19.9% of injuries
- Wild et al.[2] also found that urban and semi-urban settings have higher rates of gunshot injuries
- gunshot injuries accounted for 42.2% of injuries in urban settings
- gunshot injuries accounted for 26.7% of injuries in semi-urban settings
- gunshot injuries accounted for 7.5% of injuries in rural settings
- in the USA in 2020, over 45,000 deaths were attributed to gun-related injuries[3] (i.e. 13.6 per 100,000 people[4])
Types of Firearms and Severity of Gunshot Injury[edit | edit source]
The wounding potential of a firearm depends on various factors, including:
- the type of the firearm (muzzle velocity)
- the type of bullet
- the distance to the target
- the size of the pellets
Based on the muzzle velocity, firearms can be divided into low-velocity, medium-velocity, or high-velocity firearms.[1]
Classification[edit | edit source]
Gunshot injuries can be classified based on the type of firearm and the Gustilo-Anderson open fracture classification. You can find out more about this classification system here: Gustilo Classification.
Low-Velocity Firearms[edit | edit source]
Low-velocity firearms, including small handguns and pistols, have a muzzle velocity of less than 1200 feet.[1] They tend to cause injuries that are similar to Gustilo-Anderson Type I and Type II injuries.[5]
- Type I[5][6]
- low energy
- wound size is less than one centimetre
- minimal soft tissue damage and fracture comminution
- wound is clean
- no neuromuscular injury
- Type II[5][6]
- moderate energy
- wound size is between 1 and 10 centimetres
- moderate soft tissue damage and fracture comminution
- moderate wound contamination
- no neuromuscular injury
Medium-Velocity Firearms[edit | edit source]
Medium-velocity firearms, including high-calibre handguns and shotguns, have a muzzle velocity between 1200-2000 feet per second.[1] However, wound severity depends on various factors, including the distance and projectile.[1][7]
Example: shotguns are medium-velocity firearms, but because of the "large total mass of their lead pellets can increase their kinetic energy dramatically. [...] Depending on the distance to the target and the size of pellets, shotguns can reflect the wounding potential of high-velocity firearms or multiple low-velocity weapons. [...] Very close proximity of shotgun to the target (< 2 m) results in not only the pellet projection, but also shell fragments and wadding."[8]
High-Velocity Firearms[edit | edit source]
High-velocity firearms, including military and hunting rifles, have a muzzle velocity greater than 2000 feet per second,[1] and they are associated with more substantial tissue damage.[7] They tend to cause Gustilo-Anderson Type III wounds.[5]
- Type III (A, B, or C)[5][6]
- high energy
- wound size is usually greater than 10 centimetres
- extensive soft tissue damage
- severe fracture comminution
- extensive wound contamination
- periosteal stripping present
- may require flap coverage (III B and III C)
- exposed fracture with arterial damage that requires repair may be present (III C)
Mechanism of Gunshot Injuries[edit | edit source]
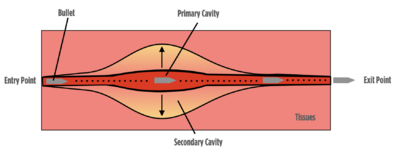
- The projectile hits the body and transfers its kinetic energy and heat to the tissues
- This creates a permanent cavity approximately the size of the projectile's cross-sectional area
- The momentarily extreme pressure around the projectile's trajectory can create a vortex effect[1]
- This vortex effect causes the tissue around the projectile's trajectory to momentarily stretch out, forming a temporary cavity, before contracting back[1]
- The projectile may exit the body, usually creating a bigger exit point, remain in the body or change direction
- Sometimes the projectile fragments or explodes inside the body, causing further damage[1]
Effects of Gunshot Injuries[edit | edit source]
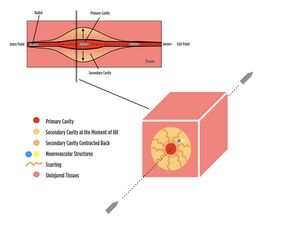
"While the tissues in the primary cavity sustain direct injury due to energy transfer, surrounding tissues within the temporary cavity sustain secondary injuries due to burns and extreme stretching."[1]
Gunshot wounds can have a range of effects, including diffuse soft tissue damage, muscle damage, nerve injury, vascular injury / haemorrhage, bone injury and severe pain.[9] These injuries are discussed in more detail below.
Soft-tissue Injury[edit | edit source]
The permanent cavity or temporary cavitation causes soft tissue damage:[9]
- tissues in the primary (permanent) cavity are injured by the projectile and extreme kinetic energy transfer[1]
- tissues in the temporary cavity are "destroyed by projectile compression and shearing that leaves a projectile trail"[9]
There may be partial or complete damage to the soft tissues, including ruptures, lacerations, internal burns and scarring in the later stages.[1]
Muscle Injury[edit | edit source]
"Skeletal muscle is suggested to be more sensitive to permanent cavitation, with temporary cavitation thought to induce less damage (unless the vasculature is disrupted) due to skeletal muscle’s inherent elasticity."[9]
Skeletal muscles can be affected by laceration, contusion or crush injury, denervation, haemorrhage, ischaemia, burns, and volumetric muscle loss. Primary trauma can be complicated by secondary trauma, including:[9]
- infection and sepsis as a result of contamination from the bullet or debris accumulated on clothing or the skin
- surgical debridement of damaged tissue
- excessive physical movement
Immobilisation and nutrient deficiency can lead to volumetric muscle loss after a gunshot injury.
Nerve Injury[edit | edit source]
Gunshot injuries can cause:[10]
- direct transection of the nerve
- indirect injury from thermal damage, shock waves, and laceration from fracture fragment displacement
- compression due to swelling or subacute scar formation
Therefore, gunshot-related injuries can cause axonotmesis, neuropraxia and neurotmesis.[11] Axonotmesis "describes the range of peripheral nerve injuries that are more severe than a minor insult, such as those resulting in neurapraxia, yet less severe than the transection of the nerve, as observed in neurotmesis."[12] Neuropraxia is the "focal segmental demyelination at the site of injury without disruption of axon continuity and its surrounding connective tissues."[13] Neurotmesis is a "complete transection of a peripheral nerve."[14]
The most frequently affected nerves in the upper extremities are the ulnar nerve and the brachial plexus.[10] Sheilds et al. also note that, in gunshot injuries, "vascular injury and fractures increase the risk of nerve injury".[10]
Vascular Injury / Haemorrhage[edit | edit source]
Blood vessels can be directly injured or affected by secondary circulatory compromise.[1] Vascular injury can lead to blood loss or haemorrhage (internal or external). A haemorrhagic area can form around irreversibly damaged tissue following gunshot injury. This extra vacation zone "is characterized by interstitial bleeding but the absence of macroscopically evident tissue destruction."[15]

Bone Injury[edit | edit source]
Gunshot injuries usually result in comminuted, displaced fractures:[1]
- caused by high-energy ballistic penetration
- a secondary effect of cavitation associated with the fluid properties of bone marrow
- associated with a high incidence of secondary complications, including infection and nonunion[16]
A drill-hole effect is often caused by low-energy injuries to porous, low-density / cancellous bone[8]:
- more common in the pelvis, distal femur, proximal humerus and spine[8]
- low-energy ballistic penetration
- affects the metaphyseal region of long bones
Unicortical fractures:
- can be due to "low-energy missile impact that creates only a tangential bone defect"[8]
Transverse or spiral fractures:
- can be caused by lower-energy gunshots to dense and highly-mineralised diaphyseal cortical bone
Gunshot injuries can result in secondary injuries (e.g. a fall), which can also result in fracture.[8][17]
Pain[edit | edit source]
- Patients with gunshot wounds in a combat setting have a high risk of chronic pain, "45% higher than the general population in civilian trauma patients"[18]
- 70% of individuals with gunshot injuries develop chronic pain[19]
- Kuchyn and Horoshko[18] found that individuals who were injured by gunshots in three or more areas had a higher percentage of chronic pain than those with injuries to one or two areas
- Complex regional pain syndrome (CRPS) can occur after traumatic events, including gunshot injuries[20]
Determinants of Injury Severity[edit | edit source]
- Projectile: velocity, mass, shape, calibre, material, yawing and impact distance:[9][1]
- mass / shape: as projectile diameter / length increase, more damage is likely
- velocity: as the velocity increases, the amount of kinetic energy dramatically increases, causing more harm
- impact distance: as projectiles travel longer distances, they lose more of their kinetic energy and cause less harm, whereas even smaller projectiles from close distances can cause extensive damage
- yaw is "the angle between the long axis of the bullet and its direction of flight."[21] As the distance increases, the projectile loses its stability and starts to yaw off. While this decreases the amount of kinetic energy transfer, it can increase the cross-sectional area, causing more damage[1]
- Type of tissue: density, elasticity, and thickness[9]
- high elasticity and low density equal less damage[21]
- skin has a high degree of elasticity and relatively low density
- lungs have a much lower density and absorb less energy
- bones are dense and absorb more energy
- The entry and exit points and trajectory within the body[1]
- if they are close to the nervous plexus, more severe damage can occur
- if they are close to main arteries or veins, the clinical presentation can be more complicated
- Projectile fragmentation
- more fragments = more than one trajectory within the body, which results in more severe internal issues to manage in the following days and months[1]
Potential Challenges and Secondary Complications of Gunshot Injuries[edit | edit source]
The management of the secondary complications related to the gunshot injury is complex. Early intervention and in-depth knowledge are required to maximise rehabilitation outcomes.
Some secondary complications of gunshot injuries are listed below:[1]
- joint contractures can develop as a result of periods of immobilisation after comminuted and complex open fractures that require external / internal fixation
- myofascial, chronic, or neuropathic pain can develop due to internal scarring, internal burns, wound or bone infection
- peripheral nerve injuries that are initially undetected due to heterogeneity and the conditions on the field may require referral to a specialist
- deep vein thrombosis or different types of embolism
- complex regional pain syndrome (causalgia) known as military pain syndrome - "tends to affect combat soldiers after they sustain wartime injuries from blasts and gunshots"[22]
- central sensitisation
- mental health issues, including post-traumatic stress disorder, anxiety or depression, which tend to worsen over time with long-term declines in mental health status[23]
Skills and Knowledge Required to Treat Gunshot Injuries[edit | edit source]
It is recommended that rehabilitation professionals treating gunshot injuries have a solid understanding of the following topics:[1]
- neuroanatomy
- to perform a neurological examination
- to plan treatment
- to recognise signs and symptoms that warrant referral to speciality services
- pain neuroscience
- to provide pain education to help manage chronic / persistent pain
- clinical reasoning
- to manage complex cases
- to participate in / lead a multidisciplinary team
- manual skills
- to help manage joint contractures, internal scarring, and neurogenic compromise
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 Altunbezel Z. Introduction to Gunshot Injury Rehabilitation Course. Plus, 2024.
- ↑ 2.0 2.1 2.2 Wild H, Stewart BT, LeBoa C, Stave CD, Wren SM. Epidemiology of Injuries Sustained by Civilians and Local Combatants in Contemporary Armed Conflict: An Appeal for a Shared Trauma Registry Among Humanitarian Actors. World J Surg. 2020 Jun;44(6):1863-1873.
- ↑ Stewart S, Tunstall C, Stevenson T. Gunshot wounds in civilian practice: a review of epidemiology, pathophysiology and management. Orthopaedics and Trauma 2023; 37(4):216-221.
- ↑ Menezes JM, Batra K, Zhitny VP. A nationwide analysis of gunshot wounds of the head and neck: morbidity, mortality, and cost. J Craniofac Surg. 2023 Sep 1;34(6):1655-60.
- ↑ 5.0 5.1 5.2 5.3 5.4 Gustilo Classification. Available from https://www.orthobullets.com/trauma/1003/gustilo-classification [last access 14.04.2024]
- ↑ 6.0 6.1 6.2 Kim PH, Leopold SS. In brief: Gustilo-Anderson classification. [corrected]. Clin Orthop Relat Res. 2012 Nov;470(11):3270-4. doi: 10.1007/s11999-012-2376-6. Epub 2012 May 9. Erratum in: Clin Orthop Relat Res. 2012 Dec;470(12):3624. Erratum in: Clin Orthop Relat Res. 2019 Oct;477(10):2388.
- ↑ 7.0 7.1 Baum GR, Baum JT, Hayward D, MacKay BJ. Gunshot Wounds: Ballistics, Pathology, and Treatment Recommendations, with a Focus on Retained Bullets. Orthop Res Rev. 2022 Sep 5;14:293-317.
- ↑ 8.0 8.1 8.2 8.3 8.4 Gugala Z, Lindsey RW. Classification of Gunshot Injuries in Civilians. Clinical Orthopaedics and Related Research 2003;408():p 65-81.
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 9.6 Moriscot A, Miyabara EH, Langeani B, Belli A, Egginton S, Bowen TS. Firearms-related skeletal muscle trauma: pathophysiology and novel approaches for regeneration. NPJ Regen Med. 2021 Mar 26;6(1):17.
- ↑ 10.0 10.1 10.2 Shields LBE, Iyer VG, Zhang YP, Shields CB. Gunshot-related nerve injuries of the upper extremities: clinical, electromyographic, and ultrasound features in 22 patients. Front Neurol. 2024 Jan 11;14:1333763.
- ↑ Straszewski AJ, Schultz K, Dickherber JL, Dahm JS, Wolf JM, Strelzow JA. Gunshot-Related Upper Extremity Nerve Injuries at a Level 1 Trauma Center. J Hand Surg Am. 2022 Jan;47(1):88.e1-88.e6.
- ↑ Chaney B, Nadi M. Axonotmesis. 2023 Sep 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–.
- ↑ Biso GMNR, Munakomi S. Neuroanatomy, Neurapraxia. [Updated 2022 Oct 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from https://www.ncbi.nlm.nih.gov/books/NBK557746/ [last access 16.04.2024]
- ↑ Matos Cruz AJ, De Jesus O. Neurotmesis. [Updated 2023 Aug 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK559108/
- ↑ Stefanopoulos PK, Hadjigeorgiou GF, Filippakis K, Gyftokostas D. Gunshot wounds: A review of ballistics related to penetrating trauma. Journal of Acute Disease 2014;3(3):178-185.
- ↑ 16.0 16.1 16.2 Yeganeh A, Amiri S, Otoukesh B, Moghtadaei M, Sarreshtedari S, Daneshmand S, Mohseni P. Characteristic Features and Outcomes of Open Gunshot Fractures of Long-bones with Gustilo Grade 3: A Retrospective Study. Arch Bone Jt Surg. 2022 May;10(5):453-458.
- ↑ Smith HW, Wheatley KK Jr. Biomechanics of femur fractures secondary to gunshot wounds. J Trauma. 1984 Nov;24(11):970-7.
- ↑ 18.0 18.1 Kuchyn I, Horoshko V. Chronic pain in patients with gunshot wounds. BMC Anesthesiol. 2023 Feb 7;23(1):47.
- ↑ Horoshko V. Value of the number of injured anatomical parts of the body and surgeries for pain chronicity in patients with gunshot wounds and blast injuries. Emergency Medicine 2023;19(3):141–143.
- ↑ Tieppo Francio V, Barndt B, Towery C, Allen T, Davani S. Complex regional pain syndrome type II arising from a gunshot wound (GSW) associated with infective endocarditis and aortic valve replacement. BMJ Case Rep. 2018 Oct 16;2018:bcr2018224702.
- ↑ 21.0 21.1 Gunshot Wounds: Management and Myths (2012). Available from https://www.reliasmedia.com/articles/76797-gunshot-wounds-management-and-myths [last access 16.04.2024]
- ↑ Nelson CN, Glauser G, Kessler RA, Jack MM. Causalgia: a military pain syndrome. Neurosurgical Focus 2022;53(3): E9.
- ↑ Greenspan AI, Kellermann AL. Physical and psychological outcomes 8 months after serious gunshot injury. J Trauma. 2002 Oct;53(4):709-16.