Decompressive Craniectomy (DC)
Original Editor - Syeda Bushra Zehra Zaidi
Top Contributors - Syeda Bushra Zehra Zaidi, Kim Jackson, Vidya Acharya, Lucinda hampton and Carina Therese Magtibay
Decompressive Craniectomy (DC)[edit | edit source]
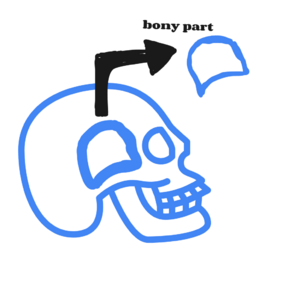
An injury to the brain may cause it to swell. Pressure within the skull then increases as the brain has no room to expand this excess pressure, known as intracranial pressure, can cause further brain injury. High intracranial pressure (ICP) is the most frequent cause of death and disability in brain‐injured patients. If high ICP cannot be controlled using general or first‐line therapeutic measures such as adjusting body temperature or carbon dioxide levels in the blood and sedation, second‐line treatments are initiated. One of these is a procedure called decompressive craniectomy (DC). DC involves the removal of a section of skull so that the brain has room to expand and the pressure decrease. There is however clinical uncertainty regarding the use of DC and a lack of consensus on the optimal management of traumatic brain injury.
Decompressive craniectomy is a neurosurgical procedure used to treat life-threatening elevations in intracranial pressure caused by cerebral edema. Removal of the cranial segment leaves the craniectomy site unprotected during the recovery period. Patients are left at risk for severe brain injury in the event of a traumatic impact to the craniectomy site[1]
Types of surgical decompression[edit | edit source]
Decompressive craniectomy can be performed in two completely different situations.
- Prophylactic decompression or primary decompressive craniectomy (P‐DC) is defined in this review as any surgical decompression performed, with or without brain tissue removal, in patients undergoing surgery primarily for the evacuation of any type of intradural lesion. The aim of prophylactic craniectomy is not to control refractory ICP but to avoid expected postsurgical increases in ICP. In these procedures, the decision taken by the surgeon is generally independent of ICP and is usually based on a CT scan or intraoperative surgical findings (brain swelling, a 'tight' brain, or difficulties in repositioning the bone flap), or both
- Therapeutic decompression or secondary decompressive craniectomy (S‐DC) is defined as the procedure performed in patients in whom continuous ICP monitoring is conducted and in whom high ICP is refractory to medical treatment. This therapeutic option is used in some centers after first‐ or second‐line therapeutic measures have failed to control ICP. In the category of S‐DC we also included patients who had undergone a first surgical procedure to evacuate a space‐occupying lesion and who had later developed delayed massive unilateral or bilateral brain swelling. Although previous surgery might have been performed in these patients, the purpose of surgical decompression is to control high ICP[2]
Surgical technique[edit | edit source]
Wide variability has been reported in the surgical procedures used for performing decompressive surgery. These variations include small to massive amounts of bone removal, uni‐ or bilateral bone decompression, opening the duramater or leaving it closed, scarifying the duramater to decrease its rigidity, and sectioning of the falx among others. Localization of bone removal can be unilateral, bilateral, bifrontal, or subtemporal; or it can be expanded to what has been called 'circumferential decompression[2]
Patients who undergo decompressive craniectomy (DC) are often fitted with a helmet that protects the craniectomy site from injury during rehabilitation. However, conventional "one-size-fits-all" helmets may not be feasible for certain craniectomy defects. We describe the production and use of a custom 3D-printed helmet for a DC patient where a conventional helmet was not feasible due to the craniectomy defect configuration.[3]
Reference[edit | edit source]
- ↑ Schirmer CM, Ackil AA Jr, Malek AM. Decompressive Craniectomy. Neurocrit Care. 2008;8(3):456-70. doi: 10.1007/s12028-008-9082-y. PMID: 18392785.
- ↑ 2.0 2.1 Sahuquillo J. Decompressive craniectomy for the treatment of refractory high intracranial pressure in traumatic brain injury. Cochrane Database Syst Rev. 2006;(1):CD003983. DOI: 10.1002/14651858.CD003983.pub2. Accessed May 26, 2023.
- ↑ Pang SS, Fang E, Chen KW, Leung M, Chow VL, Fang C. Patient-specific 3D-printed helmet for post-craniectomy defect - a case report. 3D Print Med. 2022 Jan 28;8(1):4. doi: 10.1186/s41205-022-00131-1. PMID: 35089457; PMCID: PMC8796519.