Wrist and Hand Osteoarthritis: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Reiter's Syndrome" to "[[Reactive Arthritis") |
||
| (44 intermediate revisions by 10 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | <div class="editorbox"> | ||
'''Original Editor '''- | '''Original Editor '''- [[User:Kristin Johnson|Kristin Johnson]] and [[User:Yuliya Bugera|Yuliya Bugera]] as part of the [[Temple University Evidence-Based Practice Project|Temple University EBP Project]] '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
''' | |||
</div> | </div> | ||
== | == Introduction == | ||
[[File:Finger_arthritis.jpg|right|frameless|240x240px]] | |||
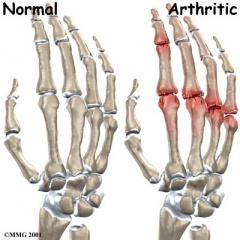
Hand [[osteoarthritis]] (OA) is a common chronic condition involving one or more joints of the thumb and fingers. It is associated with pain, reduced grip strength, loss of range of motion (ROM), and joint stiffness leading to impaired hand function and difficulty with daily activities. | |||
* Estimates of the prevalence of symptomatic hand OA range from 13% to 26% and are greater in women | |||
Evidence suggests the following: | |||
* Long-term use of a night splint offers significant benefits to improve pain, hand function, strength, and ROM for patients with OA | |||
* Programs of joint protection, advice, and home exercises are effective at improving grip strength and hand function. | |||
* Low-level laser therapy is effective at improving ROM | |||
* No rehabilitation interventions were found to improve stiffness.<ref>Ye L, Kalichman L, Spittle A, Dobson F, Bennell K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3241372/ Effects of rehabilitative interventions on pain, function and physical impairments in people with hand osteoarthritis: a systematic review.] Arthritis research & therapy. 2011 Feb;13(1):R28.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3241372/ (last accessed 18.3.2020)</ref> | |||
< | == Clinically Relevant Anatomy == | ||
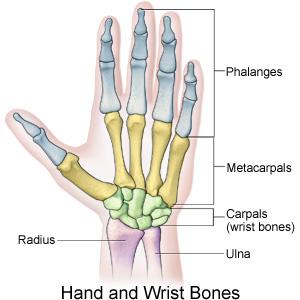
The [[Wrist and Hand|wrist and hand]] are composed of 27 bones: 8 bones of the wrist, 5 metacarpals and 14 bones of the phalanges.[[File:Hand_and_wrist_bones_II.JPG|right|frameless]]In this degenerative disorder, the articular cartilage wears away, exposing the bones. [[Cartilage]] is an elastic connective tissue whose purpose is to allow for a smooth, gliding motion between joints<ref name="Kaufmann">Kaufmann RA, Logters TT, Verbruggen G, Windolf J, Goitz RJ. Osteoarthritis of the Distal Interphalangeal Joint. Journal of Hand Surgery. 2010; 35A: 2117-2125.</ref>. | |||
=== Epidemiology === | |||
< | Epidemiologic studies of hand osteoarthritis, especially symptomatic hand osteoarthritis, are limited. | ||
* Symptomatic hand osteoarthritis is a common disorder among this elderly Caucasian population, especially among women. Most common musculoskeletal disorder worldwide affecting the hands | |||
* The most commonly involved joints were the distal interphalangeal and proximal interphalangeal joints, followed by the base of the thumb joint. | |||
* The symptomatic hand osteoarthritis is associated with weak grip strength and limits several daily functional activities. | |||
* Age: Incidence increases after 55 in women; Rate of progression increases with age<ref name="Goodman">Goodman CC, Fuller KS. Pathology: implications for the physical therapist. Third Edition. St. Louis, MO: Saunders Elsevier; 2009.</ref> | |||
* Gender: More common and more severe in women; Observed sex differences become evident after menopause<ref name="Kalichamn">Kalichman L, Hernández-Molina G. Hand osteoarthritis: an epidemiological perspective. Seminars in Arthritis and Rheumatism. 2010; 39:465-476.</ref>; The typical locations of degeneration in patients with osteoarthritis are the distal and interphalangeal joints of the hand<ref name="Zhang">Zhang W, Doherty M, Leeb BF, et al. EULAR evidence-based recommendations for the diagnosis of hand osteoarthritis: report of a task force of ESCISIT. Annals of Rheumatic Diseases. 2009; 68:8-17.</ref> | |||
* Genetics: Women; Gene mutations that code for collagen II may increase the risk of developing early OA; Role of human leukocyte antigen (HLA) types regarding the risk of OA remains much debated | |||
* Handedness: HOA mostly occurs on the dominant hand<ref name="Feydy">Feydy A, Pluot E, Guerini H, Drape JL. Role of imaging in spine, hand, and wrist osteoarthritis. 2009; 605-649.</ref> | |||
* Continuing to increase as the majority of our population increases<br> | |||
Many people may think that symptomatic hand osteoarthritis is not a common disease, because patients with hand osteoarthritis seldom seek medical care. | |||
A 2002 study found that 13.2 percent of men and 26.2 percent of women aged 70 or more years had at least one joint with symptomatic osteoarthritis. | |||
Among subjects within the same age range in the study also reported the prevalence of symptomatic hand osteoarthritis was higher than that of symptomatic knee osteoarthritis and many subjects with symptomatic hand osteoarthritis in the elderly population do not seek medical care<ref>Zhang Y, Niu J, Kelly-Hayes M, Chaisson CE, Aliabadi P, Felson DT. [https://academic.oup.com/aje/article/156/11/1021/80530 Prevalence of symptomatic hand osteoarthritis and its impact on functional status among the elderly: The Framingham Study.] American journal of epidemiology. 2002 Dec 1;156(11):1021-7. Available from:https://academic.oup.com/aje/article/156/11/1021/80530 (last accessed 18.3.2020)</ref> | |||
[[File:Osteoarthritis of the CMC joint.png|right|frameless]] | |||
Osteoarthritis is a disorder of the entire synovial joint organ and involves more structures than articular cartilage. The tissue changes that occur in the hand and wrist are a result of imbalance between catabolic and anabolic repair activity< | === Pathological Process === | ||
Osteoarthritis is a disorder of the entire synovial joint organ and involves more structures than articular cartilage. The tissue changes that occur in the hand and wrist are a result of imbalance between catabolic and anabolic repair activity<ref name="Goodman" />. Current evidence states that the subchondral bone may be the primary etiologic agent in osteoarthritis and joint cartilage is simply the final target of the process. Periarticular bone changes occur very early in the development of OA and these changes can be segregated into distinct patterns based on the anatomic location and pathogenic mechanisms<ref name="Goldring">Goldring SR. The role of bone in osteoarthritis pathogenesis. Rheumatic Disease Clinics of North America. 2008; 34: 561–571.</ref>. There is a progressive increase in subchondral plate thickness, alterations in the architecture of subchondral trabecular bone, formation of new bone at joint margins (osteophytes), and development of sub chondral bone cysts. Once the pathology reaches the articular cartilage, the cartilage thins and the joint space narrows. This causes sclerosis of the subchondral bone due to the new mechanical load placed on the affected joint<ref name="Goodman" />.<br> | |||
== Clinical Presentation<ref name="Zhang" /> == | |||
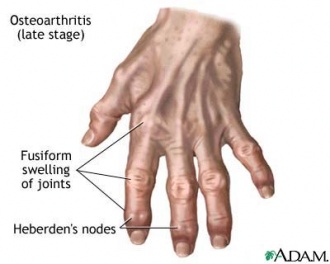
* Swelling | |||
* Stiffness, particularly in the mornings | |||
* Pain, swelling and stiffness primarily targeted to DIP, PIP, thumb base, index and middle MCP joints. | |||
* Muscle weakness | |||
* Difficulty gripping and twisting objects (doorknobs) | |||
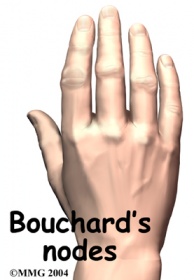
* Presence of Heberden (on distal IP joints) or Bouchard nodes (on proximal IP joints) or bony enlargements. <br> clinical hallmark* <br><br> | |||
[[Image:Heberden.jpg|330x360px|Heberden.jpg]] [[Image:Bouchard's.jpg|200x280px|Bouchard's.jpg]] | [[Image:Heberden.jpg|330x360px|Heberden.jpg]] [[Image:Bouchard's.jpg|200x280px|Bouchard's.jpg]] | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
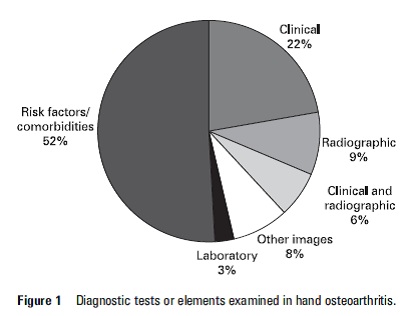
Diagnosis difficult to make due to the number of joints involved, the broad spectrum of severity and possible subsets of criteria which may exist. As well as laboratory tests there are also other factors that are used to aid the diagnosis of hand OA, such as imaging, risk factors and clinical criteria. | |||
=== Laboratory Tests === | |||
Laboratory markers such as rheumatoid factor (RF) and erythrocyte sedimentation rate (ESR) may be suggestive of rheumatoid arthritis but [[Blood Tests|blood tests]] are not required to diagnose hand OA but recommended to exclude potential coexisting diseases<ref name="Zhang" /> | |||
[[File:EULAR_risk_factors.jpg|right|frameless|404x404px]] | |||
=== Imaging === | |||
[[X-Rays|Radiographs]] (gold standard). Note joint space narrowing; osteophytes; subchondral bone: sclerosis, cysts, erosion.<ref name="Zhang" /> Kellgren-Lawrence grading allows a wide range of interpretations for each grade, reducing inter-observer reliability. Verbruggen and colleagues suggest an easy and reproducible scoring method, using numeric scores for radiographs<ref name="Feydy" /> | |||
<br> | <br>[[MRI Scans|MRI]] and Scintigraphy are often used in the early diagnosis of hand OA but their efficacy is yet to be established.<ref name="Zhang" /> | ||
< | === Risk Factors === | ||
There are many risk factors associated with hand OA and the presence of these (see list below) will help to support a diagnosis<ref name="Zhang" /> | |||
* Female gender | |||
* Increasing age over 40 | |||
* Menopausal status | |||
* Family history | |||
* Obesity | |||
* Joint laxity | |||
* Prior hand injury | |||
* Occupational and recreation-related usage | |||
=== Clinical Diagnostic Criteria === | |||
A study by Altman et al in 1990 developed clinical criteria for the diagnosis of OA of the hand based on data collected from multi-centred studies<ref name="Altman">Altman, RD. Classification of disease: osteoarthritis. Seminars in Arthritis and Rheumatism. 1991; 20(6): 40-47.</ref> | |||
* Presence of hand pain, aching, or stiffness plus | |||
* Hard tissue enlargement of at least 2 of 10 selected joints | |||
* Plus less than 3 swollen metacarpophalangeal joint | |||
* Plus either hard tissue enlargement of at least 2 distal interphalangeal | |||
* Joints or deformity of at least 1 of 10 selected joints | |||
< | == Outcome Measures<ref name="Kaufmann" /> == | ||
Outcome measures are a useful tool for determining the efficacy of physiotherapy interventions, especially the benefits of exercise and patient education.<ref name="Kaufmann" /><ref name="Valdes" /> | |||
* Score for Assessment and quantification of Chronic Rheumatic Affections of the Hands (SACRAH) | |||
* Functional Index for Osteoarthritis of the Hand (FIHOA) | |||
* [[DASH Outcome Measure|DASH]]/QuickDash<br> | |||
== Conservative Treatment == | |||
A Systematic Review of Conservative Interventions for Osteoarthritis of the Hand<ref name="Valdes">Valdes K, Marik T. A systematic review of conservative interventions for osteoarthritis of the hand. Journal of Hand Therapy. 2010; 23: 334–351.</ref><sup><br></sup>''' ''' | |||
''' Summary of Key Evidence''' | ''' Summary of Key Evidence''' | ||
| Line 76: | Line 96: | ||
| '''Level of Evidence''' | | '''Level of Evidence''' | ||
|- | |- | ||
| Hand Exercises | | [[Hand Exercises]] | ||
| | | | ||
*Increased Grip Strength | *Increased Grip Strength | ||
| Line 85: | Line 105: | ||
| Moderate | | Moderate | ||
|- | |- | ||
| Joint Protection Exercises and Provision of Adaptive Equipment | | Joint Protection Exercises and Provision of Adaptive Equipment ([https://www.kch.nhs.uk/Doc/pl%20-%20840.1%20-%20joint%20protection%20techniques%20for%20hand/finger%20arthritis.pdf Joint protection techniques for finger/ hand OA]) | ||
| | | | ||
*Increased Hand Function | *Increased Hand Function | ||
| Line 116: | Line 136: | ||
|} | |} | ||
=== Pharmacological Treatment === | |||
There is no pharmacological intervention to treatment to cure OA but instead, this intervention is indicated to improve function by providing temporary relief of symptoms | |||
== | * Intra-articular steroid injections | ||
* Analgesics | |||
* [https://physio-pedia.com/NSAID_Gastropathy?utm_source=physiopedia&utm_medium=search&utm_campaign=ongoing_internal#share Non-steroidal anti-inflammatory drugs (NSAIDs)] | |||
=== Surgery === | |||
The main indication for surgery is pain relief but it is very rarely the first option as it can result in reduced function<ref name="Talwalkar">Talwalkar SC, Hayton MJ, Stanley JK. Wrist osteoarthritis. Scandinavian Journal of Surgery. 2008; 97: 305–309.</ref>. When indicated the most common types of surgery are: | |||
* Arthrodesis of the digits and wrist, this can be either partial or full | |||
* Arthoplasty of the the knuckles or wrist<sup><br></sup> | |||
== Differential Diagnosis == | |||
There are many conditions that are similar to Hand OA and definite diagnosis is based on a combination of findings such as, clinical manifestations, risk factors, radiographic changes and laboratory tests<ref name="Zhang" />. Other conditions that have similar symptoms include: | |||
* [[Psoriatic Arthritis|Psoriatic]] arthritis (one ray or just DIP joints targeted) | |||
* [[Rheumatoid Arthritis|Rheumatoid arthritis]] (targets MCP, PIP, wrist joints) | |||
* [[gout]] (elevated serum urate levels) | |||
* [[hemochromatosis]] (targets MCP and wrist joints) | |||
* [[Reactive Arthritis|Reiter’s]] arthritis | |||
== Key Evidence == | == Key Evidence == | ||
* '''Diagnosing hand osteoarthritis: '''<br>Zhang W, Doherty M, Leeb BF, et al. EULAR evidence-based recommendations for the diagnosis of hand osteoarthritis: report of a task force of ESCISIT. Ann Rheum Dis. 2009; 68:8-17. | |||
* '''Conservative treatment for hand osteoarthritis''': <br>Valdes K, Marik T. A systematic review of conservative interventions for osteoarthritis of the hand. Journal of Hand Therapy. 2010; 23: 334–351. Walker MJ. Manual Physical Therapy Examination and Intervention of a Patient with Radial Wrist Pain: A Case Report. Journal of Orthopaedic and Sports Physical Therapy. 2004; 34 (12): 761-769. | |||
* [https://www.kch.nhs.uk/Doc/pl%20-%20840.1%20-%20joint%20protection%20techniques%20for%20hand/finger%20arthritis.pdf Joint protection techniques for finger/ hand OA] | |||
'''Conservative treatment for hand osteoarthritis''': <br> | |||
== Resources == | |||
* [http://www.arthritis.org/ Arthritis Foundation] | |||
== Resources | * [https://www.cdc.gov/arthritis/ Arthritis - Centers for Disease Control and Prevention] | ||
* [http://orthoinfo.aaos.org/ Arthritis - The American Academy of Orthopaedic Surgeons] | |||
== Case Studies == | == Case Studies == | ||
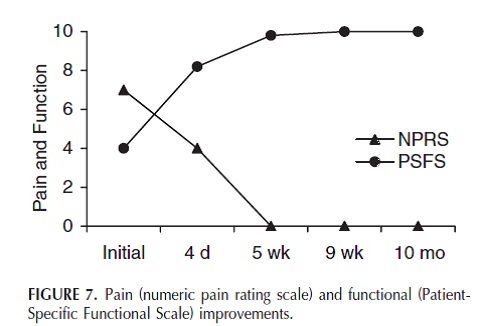
Walker et al. (2004) used an impairment based manual physical therapy approach in which the intervention included manual physical therapy in the clinic and self-mobilizations as part of a home exercise program. This impairment based approach appears to be beneficial in the treatment of CMC joint dysfunction and lead to the expeditious resolution of pain and return to full activity. Results demonstrate the clinically significant differences on the PSFS and NPRS and can be seen on the diagram below< | Walker et al. (2004) used an impairment based manual physical therapy approach in which the intervention included manual physical therapy in the clinic and self-mobilizations as part of a home exercise program. This impairment based approach appears to be beneficial in the treatment of CMC joint dysfunction and lead to the expeditious resolution of pain and return to full activity. Results demonstrate the clinically significant differences on the PSFS and NPRS and can be seen on the diagram below<ref name="Walker">Walker MJ. Manual Physical Therapy Examination and Intervention of a Patient with Radial Wrist Pain: A Case Report. Journal of Orthopaedic and Sports Physical Therapy. 2004; 34 (12): 761-769.</ref>. <br> | ||
<br> | <br> | ||
[[Image:Walker.jpg]] | [[Image:Walker.jpg]] | ||
== References == | == References == | ||
<references /><br> | |||
< | |||
<br> | |||
[[Category: | [[Category:Osteoarthritis]] | ||
[[Category:Wrist]] | |||
[[Category:Hand]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Temple_Student_Project]] | |||
[[Category:Occupational Health]] | |||
[[Category:Conditions]] | |||
[[Category:Hand - Conditions]] | |||
[[Category:Hand - Conditions]] | |||
Latest revision as of 10:15, 24 January 2022
Original Editor - Kristin Johnson and Yuliya Bugera as part of the Temple University EBP Project Top Contributors - Yuliya Bugera, Johnathan Fahrner, Lucinda hampton, Admin, Rachael Lowe, Kristin Johnson, Kim Jackson, Venugopal Pawar, Scott A Burns, WikiSysop, Anas Mohamed, Evan Thomas, Shaimaa Eldib and Amrita Patro
Introduction[edit | edit source]
Hand osteoarthritis (OA) is a common chronic condition involving one or more joints of the thumb and fingers. It is associated with pain, reduced grip strength, loss of range of motion (ROM), and joint stiffness leading to impaired hand function and difficulty with daily activities.
- Estimates of the prevalence of symptomatic hand OA range from 13% to 26% and are greater in women
Evidence suggests the following:
- Long-term use of a night splint offers significant benefits to improve pain, hand function, strength, and ROM for patients with OA
- Programs of joint protection, advice, and home exercises are effective at improving grip strength and hand function.
- Low-level laser therapy is effective at improving ROM
- No rehabilitation interventions were found to improve stiffness.[1]
Clinically Relevant Anatomy[edit | edit source]
The wrist and hand are composed of 27 bones: 8 bones of the wrist, 5 metacarpals and 14 bones of the phalanges.
In this degenerative disorder, the articular cartilage wears away, exposing the bones. Cartilage is an elastic connective tissue whose purpose is to allow for a smooth, gliding motion between joints[2].
Epidemiology[edit | edit source]
Epidemiologic studies of hand osteoarthritis, especially symptomatic hand osteoarthritis, are limited.
- Symptomatic hand osteoarthritis is a common disorder among this elderly Caucasian population, especially among women. Most common musculoskeletal disorder worldwide affecting the hands
- The most commonly involved joints were the distal interphalangeal and proximal interphalangeal joints, followed by the base of the thumb joint.
- The symptomatic hand osteoarthritis is associated with weak grip strength and limits several daily functional activities.
- Age: Incidence increases after 55 in women; Rate of progression increases with age[3]
- Gender: More common and more severe in women; Observed sex differences become evident after menopause[4]; The typical locations of degeneration in patients with osteoarthritis are the distal and interphalangeal joints of the hand[5]
- Genetics: Women; Gene mutations that code for collagen II may increase the risk of developing early OA; Role of human leukocyte antigen (HLA) types regarding the risk of OA remains much debated
- Handedness: HOA mostly occurs on the dominant hand[6]
- Continuing to increase as the majority of our population increases
Many people may think that symptomatic hand osteoarthritis is not a common disease, because patients with hand osteoarthritis seldom seek medical care.
A 2002 study found that 13.2 percent of men and 26.2 percent of women aged 70 or more years had at least one joint with symptomatic osteoarthritis.
Among subjects within the same age range in the study also reported the prevalence of symptomatic hand osteoarthritis was higher than that of symptomatic knee osteoarthritis and many subjects with symptomatic hand osteoarthritis in the elderly population do not seek medical care[7]
Pathological Process[edit | edit source]
Osteoarthritis is a disorder of the entire synovial joint organ and involves more structures than articular cartilage. The tissue changes that occur in the hand and wrist are a result of imbalance between catabolic and anabolic repair activity[3]. Current evidence states that the subchondral bone may be the primary etiologic agent in osteoarthritis and joint cartilage is simply the final target of the process. Periarticular bone changes occur very early in the development of OA and these changes can be segregated into distinct patterns based on the anatomic location and pathogenic mechanisms[8]. There is a progressive increase in subchondral plate thickness, alterations in the architecture of subchondral trabecular bone, formation of new bone at joint margins (osteophytes), and development of sub chondral bone cysts. Once the pathology reaches the articular cartilage, the cartilage thins and the joint space narrows. This causes sclerosis of the subchondral bone due to the new mechanical load placed on the affected joint[3].
Clinical Presentation[5][edit | edit source]
- Swelling
- Stiffness, particularly in the mornings
- Pain, swelling and stiffness primarily targeted to DIP, PIP, thumb base, index and middle MCP joints.
- Muscle weakness
- Difficulty gripping and twisting objects (doorknobs)
- Presence of Heberden (on distal IP joints) or Bouchard nodes (on proximal IP joints) or bony enlargements.
clinical hallmark*
Diagnostic Procedures[edit | edit source]
Diagnosis difficult to make due to the number of joints involved, the broad spectrum of severity and possible subsets of criteria which may exist. As well as laboratory tests there are also other factors that are used to aid the diagnosis of hand OA, such as imaging, risk factors and clinical criteria.
Laboratory Tests[edit | edit source]
Laboratory markers such as rheumatoid factor (RF) and erythrocyte sedimentation rate (ESR) may be suggestive of rheumatoid arthritis but blood tests are not required to diagnose hand OA but recommended to exclude potential coexisting diseases[5]
Imaging[edit | edit source]
Radiographs (gold standard). Note joint space narrowing; osteophytes; subchondral bone: sclerosis, cysts, erosion.[5] Kellgren-Lawrence grading allows a wide range of interpretations for each grade, reducing inter-observer reliability. Verbruggen and colleagues suggest an easy and reproducible scoring method, using numeric scores for radiographs[6]
MRI and Scintigraphy are often used in the early diagnosis of hand OA but their efficacy is yet to be established.[5]
Risk Factors[edit | edit source]
There are many risk factors associated with hand OA and the presence of these (see list below) will help to support a diagnosis[5]
- Female gender
- Increasing age over 40
- Menopausal status
- Family history
- Obesity
- Joint laxity
- Prior hand injury
- Occupational and recreation-related usage
Clinical Diagnostic Criteria[edit | edit source]
A study by Altman et al in 1990 developed clinical criteria for the diagnosis of OA of the hand based on data collected from multi-centred studies[9]
- Presence of hand pain, aching, or stiffness plus
- Hard tissue enlargement of at least 2 of 10 selected joints
- Plus less than 3 swollen metacarpophalangeal joint
- Plus either hard tissue enlargement of at least 2 distal interphalangeal
- Joints or deformity of at least 1 of 10 selected joints
Outcome Measures[2][edit | edit source]
Outcome measures are a useful tool for determining the efficacy of physiotherapy interventions, especially the benefits of exercise and patient education.[2][10]
- Score for Assessment and quantification of Chronic Rheumatic Affections of the Hands (SACRAH)
- Functional Index for Osteoarthritis of the Hand (FIHOA)
- DASH/QuickDash
Conservative Treatment[edit | edit source]
A Systematic Review of Conservative Interventions for Osteoarthritis of the Hand[10]
Summary of Key Evidence
| Intervention | Results | Level of Evidence |
| Hand Exercises |
|
Moderate |
| Joint Protection Exercises and Provision of Adaptive Equipment (Joint protection techniques for finger/ hand OA) |
|
Moderate |
| Paraffin |
|
Weak |
| Low-level Continuous Heat Wrap |
|
Moderate |
| CMC Orthotics (splints) |
|
Moderate |
Pharmacological Treatment[edit | edit source]
There is no pharmacological intervention to treatment to cure OA but instead, this intervention is indicated to improve function by providing temporary relief of symptoms
- Intra-articular steroid injections
- Analgesics
- Non-steroidal anti-inflammatory drugs (NSAIDs)
Surgery [edit | edit source]
The main indication for surgery is pain relief but it is very rarely the first option as it can result in reduced function[11]. When indicated the most common types of surgery are:
- Arthrodesis of the digits and wrist, this can be either partial or full
- Arthoplasty of the the knuckles or wrist
Differential Diagnosis[edit | edit source]
There are many conditions that are similar to Hand OA and definite diagnosis is based on a combination of findings such as, clinical manifestations, risk factors, radiographic changes and laboratory tests[5]. Other conditions that have similar symptoms include:
- Psoriatic arthritis (one ray or just DIP joints targeted)
- Rheumatoid arthritis (targets MCP, PIP, wrist joints)
- gout (elevated serum urate levels)
- hemochromatosis (targets MCP and wrist joints)
- Reiter’s arthritis
Key Evidence[edit | edit source]
- Diagnosing hand osteoarthritis:
Zhang W, Doherty M, Leeb BF, et al. EULAR evidence-based recommendations for the diagnosis of hand osteoarthritis: report of a task force of ESCISIT. Ann Rheum Dis. 2009; 68:8-17.
- Conservative treatment for hand osteoarthritis:
Valdes K, Marik T. A systematic review of conservative interventions for osteoarthritis of the hand. Journal of Hand Therapy. 2010; 23: 334–351. Walker MJ. Manual Physical Therapy Examination and Intervention of a Patient with Radial Wrist Pain: A Case Report. Journal of Orthopaedic and Sports Physical Therapy. 2004; 34 (12): 761-769. - Joint protection techniques for finger/ hand OA
Resources[edit | edit source]
- Arthritis Foundation
- Arthritis - Centers for Disease Control and Prevention
- Arthritis - The American Academy of Orthopaedic Surgeons
Case Studies[edit | edit source]
Walker et al. (2004) used an impairment based manual physical therapy approach in which the intervention included manual physical therapy in the clinic and self-mobilizations as part of a home exercise program. This impairment based approach appears to be beneficial in the treatment of CMC joint dysfunction and lead to the expeditious resolution of pain and return to full activity. Results demonstrate the clinically significant differences on the PSFS and NPRS and can be seen on the diagram below[12].
References[edit | edit source]
- ↑ Ye L, Kalichman L, Spittle A, Dobson F, Bennell K. Effects of rehabilitative interventions on pain, function and physical impairments in people with hand osteoarthritis: a systematic review. Arthritis research & therapy. 2011 Feb;13(1):R28.Available from:https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3241372/ (last accessed 18.3.2020)
- ↑ 2.0 2.1 2.2 Kaufmann RA, Logters TT, Verbruggen G, Windolf J, Goitz RJ. Osteoarthritis of the Distal Interphalangeal Joint. Journal of Hand Surgery. 2010; 35A: 2117-2125.
- ↑ 3.0 3.1 3.2 Goodman CC, Fuller KS. Pathology: implications for the physical therapist. Third Edition. St. Louis, MO: Saunders Elsevier; 2009.
- ↑ Kalichman L, Hernández-Molina G. Hand osteoarthritis: an epidemiological perspective. Seminars in Arthritis and Rheumatism. 2010; 39:465-476.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Zhang W, Doherty M, Leeb BF, et al. EULAR evidence-based recommendations for the diagnosis of hand osteoarthritis: report of a task force of ESCISIT. Annals of Rheumatic Diseases. 2009; 68:8-17.
- ↑ 6.0 6.1 Feydy A, Pluot E, Guerini H, Drape JL. Role of imaging in spine, hand, and wrist osteoarthritis. 2009; 605-649.
- ↑ Zhang Y, Niu J, Kelly-Hayes M, Chaisson CE, Aliabadi P, Felson DT. Prevalence of symptomatic hand osteoarthritis and its impact on functional status among the elderly: The Framingham Study. American journal of epidemiology. 2002 Dec 1;156(11):1021-7. Available from:https://academic.oup.com/aje/article/156/11/1021/80530 (last accessed 18.3.2020)
- ↑ Goldring SR. The role of bone in osteoarthritis pathogenesis. Rheumatic Disease Clinics of North America. 2008; 34: 561–571.
- ↑ Altman, RD. Classification of disease: osteoarthritis. Seminars in Arthritis and Rheumatism. 1991; 20(6): 40-47.
- ↑ 10.0 10.1 Valdes K, Marik T. A systematic review of conservative interventions for osteoarthritis of the hand. Journal of Hand Therapy. 2010; 23: 334–351.
- ↑ Talwalkar SC, Hayton MJ, Stanley JK. Wrist osteoarthritis. Scandinavian Journal of Surgery. 2008; 97: 305–309.
- ↑ Walker MJ. Manual Physical Therapy Examination and Intervention of a Patient with Radial Wrist Pain: A Case Report. Journal of Orthopaedic and Sports Physical Therapy. 2004; 34 (12): 761-769.