Vertebral Artery Test: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) (Corrected grammar) |
||
| (47 intermediate revisions by 14 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editor ''' - [[User:Rachael Lowe|Rachael Lowe]] | |||
Original Editor - | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
== Definition/Description == | |||
< | The vertebral artery test (VAT) is used in physiotherapy to test the vertebral artery blood flow to the brain, searching for symptoms of vertebral artery insufficiency and disease<ref name="p1">Jeanette Mitchell; Doppler insonation of vertebral artery blood flow changes associated with cervical spine rotation: Implications for manual therapists; Physiotherapy Theory and Practice; 2007; 23(6):303-313</ref><ref name="p2">R. Grant; Vertebral Artery Testing – the Australian Association protocol after 6 years; Manual Therapy; 1996; 1; 149-153</ref><ref name="p3">Jeanette A. Mitchell; Changes in vertebral artery flow following normal rotation of the cervical spine; Journal of Manipulative and Physiological Therapeutics; 347-351, 2002</ref>. | ||
== | The test manoeuvre causes a reduction of the lumen at the third division of the vertebral artery, resulting in decreased blood flow of the intracranial VA of the contralateral side<ref name="p2" /><ref name="p3" /><ref name="p5">Jeanette A. Mitchell; Is cervical spine rotation, as used in the standard vertebrobasilar insufficiency test, associated with a measureable change in intracranial vertebral artery blood flow?; Manual Therapy; 2004; 9 ; 220–227</ref>. It causes ischemia, due to blood loss in the pons and the medulla oblongata<ref name="p1" /><ref name="p3" /><ref name="bbb" /> of the brain. This results in dizziness, nausea, syncope, dysarthria, dysphagia, and disturbances of the hearing or vision, paresis, or paralysis of patients with Vertebrobasilar Insufficiency (VBI)<ref name="p5" />. | ||
== Clinically Relevant Anatomy == | |||
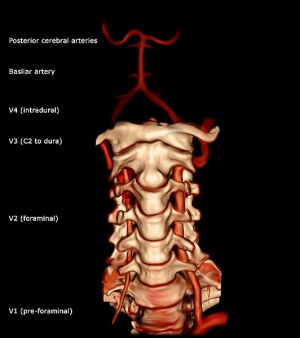
< | [[Image:532px-Vertebral artery 3D AP.jpg|thumb|right]]The [[Vertebral Artery|vertebral artery]] is a major artery in the neck<ref name="aaa">http://home.comcast.net/~wnor/lesson5.htm</ref>. It branches from the subclavian artery, where it arises from the posterosuperior portion of the subclavian artery. It ascends through the foramina of the transverse processes of the sixth cervical vertebra. Then, it winds behind the superior articular process of the atlas. It enters the cranium through the foramen magnum, where it unites with the opposite vertebral artery to form the basilar artery (at the lower border of the pons)<ref name="bbb">http://education.yahoo.com/reference/gray/subjects/subject/148</ref>. | ||
< | The vertebral artery can be divided into four divisions: The first division runs posterocranial between the longus colli and the m. scalenus anterior.<ref name="bbb" /> The first division is also called the ‘pre-foraminal division’.<ref name="aaa" /> The second division runs cranial through the foramina in the cervical transverse processes of the cervical vertebrae C2.<ref name="bbb" /> The second division is also called the foraminal division<ref name="aaa" />. The third division is defined as the part that rises from C2. It rises from the latter foramen on the medial side of the rectus capitis lateralis, and curves behind the superior articular process of the atlas. Then, it lies in the groove on the upper surface of the posterior arch of the atlas, and enters the vertebral canal by passing beneath the posterior atlantooccipital membrane<ref name="bbb" />. The fourth part pierces the dura mater and inclines medially to the front of the medulla oblongata.<ref name="bbb" /> | ||
== Purpose == | |||
== | The vertebral artery test is used to test the vertebral artery blood flow, searching for symptoms of vertebral artery insufficiency<ref name="p1" /><ref name="p2" /><ref name="p3" />. | ||
A reduction of blood flow may result in a transient ischemic attack (TIA), a critical sign of [[Stroke|impending stroke]]. It could mean that, if the disease isn’t quickly diagnosed, there is a risk of missing the opportunity to prevent permanent disability or even death<ref name="p8">Albers GW, Caplan LR, Easton JD, Fayad PB, Mohr JP, Saver JL, et al.; Transient ischemic attack—proposal for a new definition.; N Engl J Med. 2002;347:1713–6.[A2]</ref><ref name="p9">Hiroaki Naritomi, MD; Fumihiko Sakai, MD; John Stirling Meyer, MD; fckLRPathogenesis of Transient Ischemic Attacks Within the Vertebrobasilar Arterial System; Arch Neurol. 1979;36(3):121-128.[B]</ref> or if the cervical spine is placed in a compromising position, there is a risk of causing permanent disability or even death. | |||
== | According to Johnston et al<ref name="p0">Johnston CS, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA. 2000;284:2901–6.[B]</ref> the 90-day risk of stroke after a transient ischaemic attack has been estimated to approximately 10%. 50% of these strokes occur within the first two days after a TIA. Therefore, it is important to send a person with a positive test score to the hospital, where they can be examined further. TIA is often misdiagnosed as a [[Migraine Headache|migraine]], seizure, peripheral neuropathy, or anxiety<ref name="p9" />. | ||
== Technique == | |||
Active range of motion of the cervical spine is usually performed before passive assessment<ref name="p1" />. | |||
* Place patient in supine and perform a passive extension and side flexion of the head and neck<ref name="p1" /><ref name="p2" /><ref name="p3" />. | |||
* Perform passive rotation of the neck to the same side and hold for approximately 30 seconds<ref name=":0">Magee DJ. Orthopedic physical assessment. Elsevier Health Sciences; 2013 </ref>. | |||
* Repeat test with head movement to the opposite side. | |||
* Test is considered positive if there is dropping of the arms, loss of balance, or pronation of the hands; a positive result indicates decreased blood supply to the brain<ref name=":0" />. | |||
Modification: | |||
* Rotate head opposite to tested side maximally and holds position for 10 seconds | |||
* Return to neutral for 10 seconds | |||
* Extend head for 10 seconds | |||
* Return to neutral for 10 seconds | |||
* Extends and rotate head (against opposite tested side) maximally for 10 seconds | |||
* Positive symptoms include (The 5 D’s) dizziness, diplopia, dysarthria, dysphagia, drop attacks, nausea and vomiting, sensory changes, nystagmus, etc.<br> | |||
{{#ev:youtube|74l7mdVHvss|300}} <br>Below is an alternate vertebral artery test, that may be used in certain settings. For example, in the assessment of an individual with suspected BPPV. <br> {{#ev:youtube|sxXZzUomTuQ|300}} | |||
== | == Evidence == | ||
The | The test is commonly used for over the past 30 years<ref name="p2" />. The reduction of the lumen has been reported by many authors, but a lot of these studies are not sufficient because of lack of good samples of healthy people and VBI patients over a wide range of age. A study on vertebral artery testing and differential diagnosis in dizzy patients<ref name=":1">Alshahrani A, Johnson EG, Cordett TK. Vertebral artery testing and differential diagnosis in dizzy patients. Phys Ther Rehabil. 2014 Jun 5;1(1).</ref> also concluded that VAT has not been consistently validated as a clinical test for VBI. | ||
= | There are also a lot of inconsistencies in today’s literature. The review by Mitchell et al<ref name="p1" /> found that, from the twenty studies it reviewed, four studies measured the blood flow in the transverse part of the VA (first division), eleven in the second division, none in the third division, and five in the fourth division. In 7 of the 20 studies, there was no loss of blood flow in the VAI. Because of the inconsistency in the literature, there will be false positive/negative blood flow results in cervical spine rotation. Thus, the controversial findings in today’s literature cannot be used to guide evidence-based practice except to support the need for educated caution and authority in the pre-treatment screening and treatment of patients. | ||
Côté et al<ref>Cote P, Kreitz BG, Cassidy JD, Thiel H. [https://www.ncbi.nlm.nih.gov/pubmed/8728458 The validity of the extension-rotation test as a clinical screening procedure before neck manipulation: a secondary analysis.] Journal of Manipulative and Physiological Therapeutics. 1996;19(3):159-64.</ref> cite that the positive predictive value of this test (the proportion of subjects with a positive test who are correctly diagnosed) is 0%, and the negative predictive value of this test ranged from 63%-97%. The test was found not to be valid enough to detect a reduced blood flow in the VA. Therefore, the value of this test is questionable<ref name="p1" /><ref name="p3" />. | |||
== Clinical Importance == | |||
Physiotherapists should be aware of the following points in relation to the use of provocative testing for VBI<ref>Rivett D, Shirley D, Magarey M, Refshauge K. [http://www.physiotherapy.asn.au/DocumentsFolder/Resources_Guidelines_Spine_Disorders_2006.pdf Clinical guidelines for assessing vertebrobasilar insufficiency in the management of cervical spine disorders]. Australian physiotherapy association. 2006.</ref><ref name=":1" />: | |||
# The tests themselves are provocative and therefore hold some inherent risk. However, if appropriately selected and performed with care (including only to the initial point of provocation of symptoms), any potential risk to the patient will be minimised. The provocation of symptoms or signs during testing should alert the physiotherapist to the need for particular care in the selection of examination and treatment procedures. | |||
# The recommended tests are the most valid procedures for determining the presence of VBI and the adequacy of the collateral circulation identified in the literature to date. Although the tests have shown mixed results in relation to changes in vertebrobasilar arterial blood flow in experimental studies, it appears that end-range rotation is the most sensitive cervical position. Recent research has also identified blood flow changes in the simulated manipulation position. | |||
# There is no simple clinical method for testing the intrinsic state of the vertebral artery and physiotherapists should be cognisant of this when examining or treating the cervical spine. The recommended tests will not identify all patients at risk of suffering an adverse event following cervical manipulation or mobilisation. | |||
# VAT is recommended to assess the cervical positional tolerance. If the test is positive, the patient should be referred for further diagnostic tests to rule out VBI. | |||
If a patient tests positive on the Vertebral Artery Test, they may have Vertebrobasilar Insufficiency (VBI), but if they test negative on it, you '''CANNOT''' rule out Vertebrobasilar Insufficiency. | |||
== Resources == | == Resources == | ||
* [http://www.ifompt.com/site/ifompt/files/pdf/Standards%20Committee/Standards%20Committee%20Documents//IFOMPT%20Examination%20cervical%20spine%20doc%20September%202012%20definitive.pdf International Framework for Examination of the Cervical Region for potential of Cervical Arterial Dysfunction prior to Orthopaedic Manual Therapy Intervention] | |||
* [http://www.physiotherapy.asn.au/DocumentsFolder/Resources_Guidelines_Spine_Disorders_2006.pdf Clinical guidelines for assessing vertebrobasilar insufficiency in the management of cervical spine disorders]. | |||
== References == | |||
<references /> | |||
== References< | |||
[[Category:Cervical Spine - Assessment and Examination]] | |||
[[Category:Special Tests]] | |||
[[Category:Cervical Spine - Assessment and Examination]] | |||
[[Category:Arteries]] | |||
[[Category:Primary Contact]] | |||
[[Category:Cervical Spine]] | |||
[[Category:Cervical Spine - Special Tests]] | |||
Latest revision as of 16:32, 2 February 2023
Original Editor - Rachael Lowe
Top Contributors - Francky Petit, Admin, Kim Jackson, Rachael Lowe, Nick Libotton, Evan Thomas, Johnathan Fahrner, Tarina van der Stockt, Candace Goh, Naomi O'Reilly, Kai A. Sigel, WikiSysop, Claire Knott and 127.0.0.1
Definition/Description[edit | edit source]
The vertebral artery test (VAT) is used in physiotherapy to test the vertebral artery blood flow to the brain, searching for symptoms of vertebral artery insufficiency and disease[1][2][3].
The test manoeuvre causes a reduction of the lumen at the third division of the vertebral artery, resulting in decreased blood flow of the intracranial VA of the contralateral side[2][3][4]. It causes ischemia, due to blood loss in the pons and the medulla oblongata[1][3][5] of the brain. This results in dizziness, nausea, syncope, dysarthria, dysphagia, and disturbances of the hearing or vision, paresis, or paralysis of patients with Vertebrobasilar Insufficiency (VBI)[4].
Clinically Relevant Anatomy[edit | edit source]
The vertebral artery is a major artery in the neck[6]. It branches from the subclavian artery, where it arises from the posterosuperior portion of the subclavian artery. It ascends through the foramina of the transverse processes of the sixth cervical vertebra. Then, it winds behind the superior articular process of the atlas. It enters the cranium through the foramen magnum, where it unites with the opposite vertebral artery to form the basilar artery (at the lower border of the pons)[5].
The vertebral artery can be divided into four divisions: The first division runs posterocranial between the longus colli and the m. scalenus anterior.[5] The first division is also called the ‘pre-foraminal division’.[6] The second division runs cranial through the foramina in the cervical transverse processes of the cervical vertebrae C2.[5] The second division is also called the foraminal division[6]. The third division is defined as the part that rises from C2. It rises from the latter foramen on the medial side of the rectus capitis lateralis, and curves behind the superior articular process of the atlas. Then, it lies in the groove on the upper surface of the posterior arch of the atlas, and enters the vertebral canal by passing beneath the posterior atlantooccipital membrane[5]. The fourth part pierces the dura mater and inclines medially to the front of the medulla oblongata.[5]
Purpose[edit | edit source]
The vertebral artery test is used to test the vertebral artery blood flow, searching for symptoms of vertebral artery insufficiency[1][2][3].
A reduction of blood flow may result in a transient ischemic attack (TIA), a critical sign of impending stroke. It could mean that, if the disease isn’t quickly diagnosed, there is a risk of missing the opportunity to prevent permanent disability or even death[7][8] or if the cervical spine is placed in a compromising position, there is a risk of causing permanent disability or even death.
According to Johnston et al[9] the 90-day risk of stroke after a transient ischaemic attack has been estimated to approximately 10%. 50% of these strokes occur within the first two days after a TIA. Therefore, it is important to send a person with a positive test score to the hospital, where they can be examined further. TIA is often misdiagnosed as a migraine, seizure, peripheral neuropathy, or anxiety[8].
Technique[edit | edit source]
Active range of motion of the cervical spine is usually performed before passive assessment[1].
- Place patient in supine and perform a passive extension and side flexion of the head and neck[1][2][3].
- Perform passive rotation of the neck to the same side and hold for approximately 30 seconds[10].
- Repeat test with head movement to the opposite side.
- Test is considered positive if there is dropping of the arms, loss of balance, or pronation of the hands; a positive result indicates decreased blood supply to the brain[10].
Modification:
- Rotate head opposite to tested side maximally and holds position for 10 seconds
- Return to neutral for 10 seconds
- Extend head for 10 seconds
- Return to neutral for 10 seconds
- Extends and rotate head (against opposite tested side) maximally for 10 seconds
- Positive symptoms include (The 5 D’s) dizziness, diplopia, dysarthria, dysphagia, drop attacks, nausea and vomiting, sensory changes, nystagmus, etc.
Below is an alternate vertebral artery test, that may be used in certain settings. For example, in the assessment of an individual with suspected BPPV.
Evidence[edit | edit source]
The test is commonly used for over the past 30 years[2]. The reduction of the lumen has been reported by many authors, but a lot of these studies are not sufficient because of lack of good samples of healthy people and VBI patients over a wide range of age. A study on vertebral artery testing and differential diagnosis in dizzy patients[11] also concluded that VAT has not been consistently validated as a clinical test for VBI.
There are also a lot of inconsistencies in today’s literature. The review by Mitchell et al[1] found that, from the twenty studies it reviewed, four studies measured the blood flow in the transverse part of the VA (first division), eleven in the second division, none in the third division, and five in the fourth division. In 7 of the 20 studies, there was no loss of blood flow in the VAI. Because of the inconsistency in the literature, there will be false positive/negative blood flow results in cervical spine rotation. Thus, the controversial findings in today’s literature cannot be used to guide evidence-based practice except to support the need for educated caution and authority in the pre-treatment screening and treatment of patients.
Côté et al[12] cite that the positive predictive value of this test (the proportion of subjects with a positive test who are correctly diagnosed) is 0%, and the negative predictive value of this test ranged from 63%-97%. The test was found not to be valid enough to detect a reduced blood flow in the VA. Therefore, the value of this test is questionable[1][3].
Clinical Importance[edit | edit source]
Physiotherapists should be aware of the following points in relation to the use of provocative testing for VBI[13][11]:
- The tests themselves are provocative and therefore hold some inherent risk. However, if appropriately selected and performed with care (including only to the initial point of provocation of symptoms), any potential risk to the patient will be minimised. The provocation of symptoms or signs during testing should alert the physiotherapist to the need for particular care in the selection of examination and treatment procedures.
- The recommended tests are the most valid procedures for determining the presence of VBI and the adequacy of the collateral circulation identified in the literature to date. Although the tests have shown mixed results in relation to changes in vertebrobasilar arterial blood flow in experimental studies, it appears that end-range rotation is the most sensitive cervical position. Recent research has also identified blood flow changes in the simulated manipulation position.
- There is no simple clinical method for testing the intrinsic state of the vertebral artery and physiotherapists should be cognisant of this when examining or treating the cervical spine. The recommended tests will not identify all patients at risk of suffering an adverse event following cervical manipulation or mobilisation.
- VAT is recommended to assess the cervical positional tolerance. If the test is positive, the patient should be referred for further diagnostic tests to rule out VBI.
If a patient tests positive on the Vertebral Artery Test, they may have Vertebrobasilar Insufficiency (VBI), but if they test negative on it, you CANNOT rule out Vertebrobasilar Insufficiency.
Resources[edit | edit source]
- International Framework for Examination of the Cervical Region for potential of Cervical Arterial Dysfunction prior to Orthopaedic Manual Therapy Intervention
- Clinical guidelines for assessing vertebrobasilar insufficiency in the management of cervical spine disorders.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Jeanette Mitchell; Doppler insonation of vertebral artery blood flow changes associated with cervical spine rotation: Implications for manual therapists; Physiotherapy Theory and Practice; 2007; 23(6):303-313
- ↑ 2.0 2.1 2.2 2.3 2.4 R. Grant; Vertebral Artery Testing – the Australian Association protocol after 6 years; Manual Therapy; 1996; 1; 149-153
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 Jeanette A. Mitchell; Changes in vertebral artery flow following normal rotation of the cervical spine; Journal of Manipulative and Physiological Therapeutics; 347-351, 2002
- ↑ 4.0 4.1 Jeanette A. Mitchell; Is cervical spine rotation, as used in the standard vertebrobasilar insufficiency test, associated with a measureable change in intracranial vertebral artery blood flow?; Manual Therapy; 2004; 9 ; 220–227
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 http://education.yahoo.com/reference/gray/subjects/subject/148
- ↑ 6.0 6.1 6.2 http://home.comcast.net/~wnor/lesson5.htm
- ↑ Albers GW, Caplan LR, Easton JD, Fayad PB, Mohr JP, Saver JL, et al.; Transient ischemic attack—proposal for a new definition.; N Engl J Med. 2002;347:1713–6.[A2]
- ↑ 8.0 8.1 Hiroaki Naritomi, MD; Fumihiko Sakai, MD; John Stirling Meyer, MD; fckLRPathogenesis of Transient Ischemic Attacks Within the Vertebrobasilar Arterial System; Arch Neurol. 1979;36(3):121-128.[B]
- ↑ Johnston CS, Gress DR, Browner WS, Sidney S. Short-term prognosis after emergency department diagnosis of TIA. JAMA. 2000;284:2901–6.[B]
- ↑ 10.0 10.1 Magee DJ. Orthopedic physical assessment. Elsevier Health Sciences; 2013
- ↑ 11.0 11.1 Alshahrani A, Johnson EG, Cordett TK. Vertebral artery testing and differential diagnosis in dizzy patients. Phys Ther Rehabil. 2014 Jun 5;1(1).
- ↑ Cote P, Kreitz BG, Cassidy JD, Thiel H. The validity of the extension-rotation test as a clinical screening procedure before neck manipulation: a secondary analysis. Journal of Manipulative and Physiological Therapeutics. 1996;19(3):159-64.
- ↑ Rivett D, Shirley D, Magarey M, Refshauge K. Clinical guidelines for assessing vertebrobasilar insufficiency in the management of cervical spine disorders. Australian physiotherapy association. 2006.