Trigger Points: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Dry needling" to "[[Dry Needling") |
||
| (17 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div><div class="editorbox"> | <div><div class="editorbox"> | ||
'''Original Editors -[[User:Sean Wauters|Sean Wauters]]' | '''Original Editors''' -[[User:Sean Wauters|Sean Wauters]]as part of the [[Vrije Universiteit Brussel Evidence-based Practice Project|Vrije Universiteit Brussel's Evidence-based Practice project]]. | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
< | == Definition/Description == | ||
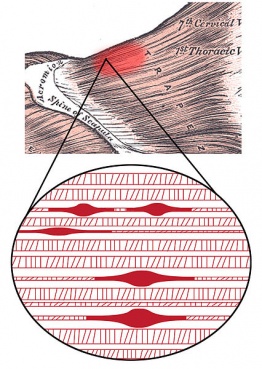
[[File:Trigger points.jpeg|thumb|369x369px|Trigger point in trapezius muscle[https://commons.wikimedia.org/wiki/File:Trigger_Point_Complex.jpg#globalusage]]]A Trigger Point (TrP) is a hyperirritable spot, a palpable nodule in the taut bands of the skeletal muscles' fascia. Direct compression or muscle contraction can elicit jump sign, local tenderness, local twitch response and referred pain which usually responds with a pain pattern distant from the spot<ref name=":0">Simons DG, Travell JG, Simons LS. [https://books.google.com/books?hl=en&lr=&id=sU0XupX7DGsC&oi=fnd&pg=PA1&dq=Simons+DG,+Travell+JG,+Simons+LS.+Travell+%26+Simons%27+myofascial+pain+and+dysfunction:+upper+half+of+body.+Lippincott+Williams+%26+Wilkins%3B+1999.%5B1%5D%5B2%5D&ots=28QDWjFNiI&sig=0r2uwOXxKjT_Q_SWmqVfCq7EoUc Travell & Simons' myofascial pain and dysfunction: upper half of body]. Lippincott williams & wilkins; 1999.</ref><ref name="David 2002">Alvarez DJ, Rockwell PG. [https://www.aafp.org/afp/2002/0215/p653.html?userguid=unk-1632566170543&condition=other&clientId=&entityId=203&clientSiteId=default&groupId=&tp=WEB_PORTAL Trigger points: diagnosis and management]. American family physician. 2002 Feb 15;65(4):653.</ref><ref name="Davidoff 1998">Davidoff RA. [https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1468-2982.1998.1807436.x Trigger points and myofascial pain: toward understanding how they affect headaches]. Cephalalgia. 1998 Sep;18(7):436-48.</ref><ref name="Eduardo 2009">Vázquez Delgado E, Cascos-Romero J, Gay Escoda C. [http://diposit.ub.edu/dspace/handle/2445/49849 Myofascial pain syndrome associated with trigger points: a literature review.(I): Epidemiology, clinical treatment and etiopathogeny]. Medicina Oral, Patología Oral y Cirugia Bucal, 2009, vol. 14, num. 10, p. 494-498. 2009 Oct 1.</ref>. | |||
'''Jump sign''' is the characteristic behavioural response to pressure on a TrP. Individuals are frequently startled by the intense pain. They wince or cry out with a response seemingly out of proportion to the amount of pressure exerted by the examining fingers. They move involuntarily, jerking the shoulder, head, or some other part of the body not being palpated. A jump sign thus reflects the extreme tenderness of a TrP. This sign has been considered pathognomonic for the presence of TrPs. | |||
'''Local twitch response''' - defined as a transient visible or palpable contraction of the muscle and skin as the tense muscle fibres contract when pressure is applied through needle penetration or by transverse snapping palpation. A local twitch response on stimulating active TrPs is a widely accepted diagnostic sign<ref>Yap EC. [https://annals.edu.sg/pdf/36VolNo1Jan2007/V36N1p43.pdf Myofascial pain-an overview.] Annals-Academy of Medicine Singapore. 2007 Jan 1;36(1):43.</ref>. | |||
''' | '''Referred pain''', also called reflective pain, is pain perceived at a location other than the site of the painful stimulus. Pain is reproducible and does not follow dermatomes, myotomes, or nerve roots. There is no specific joint swelling or neurological deficits. Pain from a myofascial TrP is a distinct, discrete and constant pattern or map of pain with no gender or racial differences able to reproduce symptoms - '''referred pain map'''<ref name=":1" />. | ||
(Radiating pain is slightly different from referred pain; for example, the pain related to a myocardial infarction could either be referred or radiating pain from the chest. Referred pain is when the pain is located away from or adjacent to the organ involved; for instance, when a person has pain only in their jaw or left arm, but not in the chest)<ref name=":0" /><ref>Ray BS, Wolff HG. [https://jamanetwork.com/journals/jamasurgery/article-abstract/544771 Experimental studies on headache: pain-sensitive structures of the head and their significance in headache]. Archives of surgery. 1940 Oct 1;41(4):813-56.</ref>. | |||
== Anatomy and Etiology == | |||
== | Trigger points develop in the [[Myofascial Release|myofascia]], mainly in the centre of a muscle belly where the motor endplate enters (primary or central TrPs)<ref name=":1">Niel-Asher S. The concise book of trigger points: A professional and self-help manual. North Atlantic Books; 2014 Sep 16.</ref>. Those are palpable nodules within the tight muscle at the size of 2-10 mm and can be demonstrated at different places in any skeletal muscles of the body. We all have TrPs in the body. Can be present even in babies and children, but their presence does not necessarily result in the formation of pain syndrome. When it happens, TrPs are directly associated with myofascial pain syndrome*, somatic dysfunction, psychological disturbance and restricted daily functioning<ref>Simons DG, Travell JG, Simons LS. [https://books.google.com/books?hl=en&lr=&id=sU0XupX7DGsC&oi=fnd&pg=PA1&dq=Simons+DG,+Travell+JG,+Simons+LS.+Travell+%26+Simons%27+myofascial+pain+and+dysfunction:+upper+half+of+body.+Lippincott+Williams+%26+Wilkins%3B+1999.%5B1%5D&ots=28QDWjFSfJ&sig=BdwAZUBTQoJRsl1cJBfp6RirMSM Travell & Simons' myofascial pain and dysfunction: upper half of body]. Lippincott williams & wilkins; 1999.</ref>. | ||
'''*[[Myofascial pain|Myofascial Pain Syndrome]]''' refers to regional pain of soft tissue origin and is associated with muscle tenderness that arises from TrPs, focal points of tenderness, a few millimetres in diameter, found at multiple sites in a muscle and the fascia of muscle tissue<ref>Jantos M. [https://www.researchgate.net/profile/Marek-Jantos/publication/228376053_Understanding_chronic_pelvic_pain/links/55f29b2a08aef559dc493b60/Understanding-chronic-pelvic-pain.pdf Understanding chronic pelvic pain]. Pelviperineology. 2007 Jun 1;26(2):66.</ref>. | |||
'''Causes -''' Usually, TrPs | '''Causes -''' Usually, TrPs happen due to: | ||
* | * Ageing, | ||
* | * Injury sustained by a fall, by stress or birth trauma. | ||
* | * Lack of exercise - commonly in sedentary persons between 27,5-55 years, of which 45% are men<ref name="Eduardo 2010">Vázquez Delgado E, Cascos-Romero J, Gay Escoda C. [http://diposit.ub.edu/dspace/handle/2445/49851 Myofascial pain associated to trigger points: a literature review. Part 2: differential diagnosis and treatment]. Medicina Oral, Patología Oral y Cirugia Bucal, 2010, vol. 15, num. 4, p. 639-643. 2010 Jul 1.</ref>, | ||
* | * Bad posture - upper and lower crossed pattern, swayback posture, telephone posture, cross-legged sitting, | ||
* | * Muscle overuse and respective micro-trauma - weightlifting, | ||
* | * Chronic stress condition - anxiety, depression, psychological stress trauma, | ||
* | * Vitamin deficiencies - vitamin C, D, B; folic acid; iron; | ||
* | * Sleep disturbance, | ||
* | * Joint problems and hypermobility. | ||
</div> | </div> | ||
| Line 37: | Line 36: | ||
== Classification of TrPs == | == Classification of TrPs == | ||
<div> | <div> | ||
TrPts can be divided | TrPts can be divided into several groups<ref name=":1" /> | ||
</div> | </div> | ||
=== Primary / Central and Secondary / Satellite Trigger Points === | |||
<div> | <div> | ||
* Primary or Central TrPs are those that cause severe pain locally at the pressure with irradiation according to referred pain map. Usually are based around center of a muscle belly. | * Primary or Central TrPs are those that cause severe [[Pain-Modulation|pain]] locally at the pressure with irradiation according to the referred pain map. Usually are based around the center of a muscle belly. | ||
* Secondary or Satellite TrPs arise in response to existing central trigger points in surrounding muscles. They usually spontaneously withdraw when the central TrP is healed. Can be present in form of a cluster. | * Secondary or Satellite TrPs arise in response to existing central trigger points in surrounding muscles. They usually spontaneously withdraw when the central TrP is healed. Can be present in the form of a cluster. | ||
</div> | </div> | ||
=== Active and Inactive /Latent Trigger Points === | |||
<div> | <div> | ||
* Active TrP is any point that causes tenderness and | * Active TrP is any point that causes tenderness and referred pain on palpation. Palpation may also cause autonomic symptoms such as skin redness, sweating, and dizziness<ref>Pringle K. [https://www.jmptonline.org/article/S0161-4754(99)70079-5/abstract Myofascial Pain and Dysfunction: The Trigger Point Manual]. Journal of Manipulative & Physiological Therapeutics. 1999 Jun 1;22(5):A1.</ref>. | ||
* | * Latent TrP does not evoke pain spontaneously, and local or referred pain occurs only with strong digital pressure<ref name=":2">Fernández-de-Las-Peñas C, Dommerholt J. [https://academic.oup.com/painmedicine/article-abstract/19/1/142/4091339 International consensus on diagnostic criteria and clinical considerations of myofascial trigger points: a Delphi study]. Pain Medicine. 2018 Jan 1;19(1):142-50.</ref>. They may change muscle activation patterns or cause muscle weakness in pain-free patients<ref>Ge HY, Monterde S, Graven-Nielsen T, Arendt-Nielsen L. Latent Myofascial Trigger Points Are Associated With an Increased Intramuscular Electromyographic Activity During Synergistic Muscle Activation. The journal of pain. [https://www-sciencedirect-com.ezproxy.library.uq.edu.au/science/article/pii/S1526590013013187 2014;15(2):181–7.]</ref><ref>Celik D, Yeldan İ. [https://content.iospress.com/articles/journal-of-back-and-musculoskeletal-rehabilitation/bmr00302 The relationship between latent trigger point and muscle strength in healthy subjects: a double-blind study]. Journal of Back and Musculoskeletal Rehabilitation. 2011 Jan 1;24(4):251-6.</ref>. | ||
* Reproduction of painful symptoms is the diagnostic criterion differentiating between the two<ref name=":2" />. | |||
</div> | </div> | ||
=== Diffuse Trigger Points === | |||
<div> | <div> | ||
* Commonly | * Commonly happens in case of severe postural deformity where initially primary TrPs are multiple, so secondary multiple TrPs are only a response of a mechanism, called diffuse. | ||
</div> | </div> | ||
=== Attachment Trigger Points === | |||
<div> | <div> | ||
* Arise in tendo- | * Arise in tendo-osseous junctions which become very tender. If not treated, degenerative processes of an adjacent joint can spring up. | ||
</div> | </div> | ||
=== Ligamentous Trigger Points === | |||
<div> | <div> | ||
* Even ligaments can develop trigger points. | * Even ligaments can develop trigger points. The presence of TrPs in the anterior longitudinal ligament of the spine can result in neck instability. Some knee pain syndromes are successfully healed when treated ligamentum patellae and fibular collateral ligament. | ||
</div> | </div> | ||
== Pathogenesis and Theories == | == Pathogenesis and Theories == | ||
<div> | <div> | ||
Little is known about the formation of TrPs. There are some theories written in literature | Little is known about the formation of TrPs. There are some theories written in literature that try to explain the formation, sensitization, and manifestation of TrPs, but few of them have strong evidence<ref name="Davidoff 1998" /><ref>Delgado EV, Romero JC, Gay-Escoda C. [https://dialnet.unirioja.es/servlet/articulo?codigo=5994615 Myofascial pain syndrome associated with trigger points: A literature review.(I): Epidemiology, clinical treatment and etiopathogeny]. Medicina oral, patología oral y cirugía bucal. Ed. inglesa. 2009;14(10):1.</ref><ref name="Elizabeth 2009">Tough EA, White AR, Cummings TM, Richards SH, Campbell JL. [https://www.sciencedirect.com/science/article/pii/S1090380108000554 Acupuncture and dry needling in the management of myofascial trigger point pain: a systematic review and meta-analysis of randomised controlled trials]. European Journal of Pain. 2009 Jan 1;13(1):3-10.</ref>. | ||
Under normal conditions, pain from TrPs is mediated by thin myelinated (Ad) fibres and unmyelinated (C) fibres. Various noxious and innocuous events, such as mechanical stimuli or chemical mediators, may excite and sensitize Ad fibres and C fibres and thereby play a role in the development of TrPs | Under normal conditions, pain from TrPs is mediated by thin myelinated (Ad) fibres and unmyelinated (C) fibres. Various noxious and innocuous events, such as mechanical stimuli or chemical mediators, may excite and sensitize Ad fibres and C fibres and thereby play a role in the development of TrPs. | ||
'''Integrated Trigger Point Hypothesis (ITPH)''' is the present working hypothesis. | '''Integrated Trigger Point Hypothesis (ITPH)''' is the present working hypothesis. When [[Sarcomere|sarcomeres]] and motor endplate become overactive for a number of different reasons, pathological changes start at cellular levels. This turns on permanently sarcomeres leading to a local inflammatory response, loss of oxygen supply, loss of nutrient supply, endogenous (involuntary) shortening of muscle fibres, and increased metabolic demand on local tissues. Electrophysiological investigations of TrPs reveal phenomena which indicate that the electrical activity arises from dysfunctional extrafusal motor endplates rather than from muscle spindles<ref>Simons DG. [https://www.tandfonline.com/doi/abs/10.1300/J094v04n01_07 Clinical and etiological update of myofascial pain from trigger points]. Journal of musculoskeletal pain. 1996 Jan 1;4(1-2):93-122.</ref>. | ||
'''Polymodal theory''' explains the existence of polymodal receptors (PMRs) throughout the body which under certain constant, pathological stimuli turn into trigger points<ref>Kawakita K, Itoh K, Okada K. The polymodal receptor hypothesis of acupuncture and moxibustion, and its rational explanation of acupuncture points. InInternational Congress Series 2002 Aug 1 (Vol. 1238, pp. 63-68). Elsevier. | '''Polymodal theory''' explains the existence of polymodal receptors (PMRs) throughout the body which under certain constant, pathological stimuli turn into trigger points<ref>Kawakita K, Itoh K, Okada K. [https://www.sciencedirect.com/science/article/pii/S0531513102004119 The polymodal receptor hypothesis of acupuncture and moxibustion, and its rational explanation of acupuncture points]. InInternational Congress Series 2002 Aug 1 (Vol. 1238, pp. 63-68). Elsevier.</ref>. | ||
'''Radiculopathic theory''' explains direct relationship between problems on nerve roots which lead to local and distant neurovascular signals and trigger points creation<ref>Gunn CC, Wall PD. The Gunn approach to the treatment of chronic pain: intramuscular stimulation for myofascial pain of radiculopathic origin. Churchill Livingstone; 1996. | '''Radiculopathic theory''' explains the direct relationship between problems on nerve roots which lead to local and distant neurovascular signals and trigger points creation<ref>Gunn CC, Wall PD. The Gunn approach to the treatment of chronic pain: intramuscular stimulation for myofascial pain of radiculopathic origin. Churchill Livingstone; 1996.</ref>. | ||
'''Peripheral and Central Sensitization''' - Central sensitization is a phenomenon, together with peripheral sensitization, which helps understanding chronic or amplified pain. There is central sensitization after intense or repetitive stimulus of the nociceptor present in the periphery, leading to reversible increase of excitability and of synaptic efficacy of central nociceptive pathway neurons. Manifested as hypersensitivity to pain (called tactile allodynia and hyperalgesia secondary to puncture or pressure). These CNS changes may be detected by electrophysiological or imaging techniques<ref>Fernández-de-las-Peñas C, Cuadrado ML, Arendt-Nielsen L, Simons DG, Pareja JA. Myofascial trigger points and sensitization: an updated pain model for tension-type headache. Cephalalgia. 2007 May;27(5):383-93.</ref><ref>Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. | '''Peripheral and Central Sensitization''' - Central sensitization is a phenomenon, together with peripheral sensitization, which helps in understanding chronic or amplified pain. There is central sensitization after an intense or repetitive stimulus of the nociceptor present in the periphery, leading to a reversible increase of excitability and of the synaptic efficacy of central nociceptive pathway neurons. Manifested as hypersensitivity to pain (called tactile allodynia and hyperalgesia secondary to puncture or pressure). These CNS changes may be detected by electrophysiological or imaging techniques<ref>Fernández-de-las-Peñas C, Cuadrado ML, Arendt-Nielsen L, Simons DG, Pareja JA. [https://journals.sagepub.com/doi/pdf/10.1111/j.1468-2982.2007.01295.x Myofascial trigger points and sensitization: an updated pain model for tension-type headache]. Cephalalgia. 2007 May;27(5):383-93.</ref><ref>Woolf CJ. [https://www.sciencedirect.com/science/article/pii/S0304395910005841 Central sensitization: implications for the diagnosis and treatment of pain]. pain. 2011 Mar 1;152(3):S2-15.</ref>. | ||
== Differential Diagnosis == | == Differential Diagnosis == | ||
* | * [[Fibromyalgia]] - characterized by diffused fatigue and aches all over the body. More often in women, does not involve joints but does involve all other tissues (muscle, bone, tendon, ligaments, and fat) and can develop tender points. Tender points are discrete areas of tenderness over soft tissues that cause local pain and are tender to palpation but patients do not present jump signs when pressed nor referred pain maps. These two pain syndromes may overlap in symptoms and are difficult to differentiate without a thorough exam by a skilled physician. Although they may be concomitant and may interact with one another<ref name="David 2002" /><ref name="Eduardo 2010" />. | ||
Other conditions which include muscle pain and trigger points: | Other conditions which include muscle pain and trigger points: | ||
* | * Musculoskeletal Diseases | ||
# Occupational myalgias | # Occupational myalgias | ||
# Post-traumatic hyperirritability syndrome | # Post-traumatic hyperirritability syndrome | ||
# Joint dysfunction (osteoarthritis) | # Joint dysfunction ([[osteoarthritis]]) | ||
# Tendonitis and bursitis | # [[Tendinopathy|Tendonitis]] and [[bursitis]] | ||
* | * Neurological Disorders | ||
# Trigeminal neuralgia | # [[Trigeminal Neuralgia|Trigeminal neuralgia]] | ||
# Glossopharyngeal neuralgia | # Glossopharyngeal neuralgia | ||
# Sphenopalatine neuralgia | # Sphenopalatine neuralgia | ||
* | * Systemic Diseases | ||
# | # [[Systemic Lupus Erythematosus|Systemic lupus erythematosus (SLE)]] | ||
# Rheumatoid arthritis | # [[Rheumatoid Arthritis|Rheumatoid arthritis]] | ||
# Gout | # [[Gout]] | ||
# Psoriatic arthritis | # [[Psoriatic Arthritis|Psoriatic arthritis]] | ||
# Infections (viral, bacterial, protozoan, parasitic and Candida albicans infection) | # Infections (viral, bacterial, protozoan, parasitic and Candida albicans infection) | ||
# Lyme | # [[Lyme Disease]] | ||
# Hypoglycemia and Hypothyroidism | # Hypoglycemia and Hypothyroidism | ||
* | * Heterotopic Pain of Central Origin | ||
* | * Axis II-Type Disorders | ||
# Psychogenic pain | # Psychogenic pain | ||
# Painful | ## Painful behaviours | ||
</div> | </div> | ||
== Symptoms | == Symptoms and Clinical Findings == | ||
<div> | <div> | ||
* | * A patient usually asks for help due to a chronic pain state (e.g.: headaches, aches everywhere, morning stiffness, TMJ syndrome, tinnitus...), which, in reality, is often physically away from the active trigger point. | ||
* | * Muscle weakness or imbalance, altered motor recruitment, in either the affected muscle or in functionally related muscles. | ||
* | *Changes in Range of Motion (ROM). | ||
* | *Painful movement and/or movement that sometimes can exacerbate symptoms. | ||
* | *Tension headaches, migraines, tinnitus, temporomandibular joint problems... as accompanying symptoms. | ||
* | *Postural abnormalities and compensations. | ||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
=== Palpation === | |||
Palpation remains the current standard for diagnosis and assessment of TrPs and is the standard against which new diagnostic methods are assessed<ref name=":3">Mazza DF, Boutin RD, Chaudhari AJ. [https://journals.lww.com/ajpmr/Fulltext/2021/10000/Assessment_of_Myofascial_Trigger_Points_via.12.aspx Assessment of myofascial trigger points via imaging: a systematic review]. American Journal of Physical Medicine & Rehabilitation. 2021 Oct 1;100(10):1003-14.</ref>. However, interrater reliability estimates for palpation vary widely, suggesting palpation is unreliable<ref>Rathbone AT, Grosman-Rimon L, Kumbhare DA. [https://www.ingentaconnect.com/content/wk/cjpn/2017/00000033/00000008/art00007 Interrater agreement of manual palpation for identification of myofascial trigger points]. The Clinical journal of pain. 2017 Aug 1;33(8):715-29.</ref>. | |||
==== Imaging ==== | |||
Imaging modalities have recently shown potential to identify TrPs: | |||
Sonoelastography was able to detect differences between clinically relevant groups and identify TrPs. It is hypothesized that vibration sonoelastography and shear wave elastography have more reliable results due to their use of mechanically-induced stimuli<ref name=":3" />. | |||
<br> | |||
</div> | </div> | ||
=== Anamnesis === | |||
<div> | <div> | ||
Anamnesis (a patient's account of their own clinical history) should be specific. The patient must be asked about fibromyalgia, as well as the presence of it in the family history of diseases. Also, the patient should be asked about his physical and daily activities in the | Anamnesis (a patient's account of their own clinical history) should be specific. The patient must be asked about fibromyalgia, as well as the presence of it in the family history of diseases. Also, the patient should be asked about his physical and daily activities in the present and in the past as a lack of exercise and sedentary life may be a pathogenic factor. Furthermore, chronic muscle overuse, daily stress, medications (and their overuse), and sleep disturbances have to be asked about and examined in detail. | ||
</div> | </div> | ||
=== Examination === | |||
<div> | <div> | ||
In 2018, an international Delphi panel revised the TrP diagnostic approach and proposed that at least two of the following criteria must be present: a taut band, a hypersensitive spot, and [[Referred Pain|referred pain]]. | |||
Palpation should be performed by moving the fingertips forward and backwards, perpendicular to the muscle fibres. Alternatively, some muscles can be palpated using a pincer grip. Once the taut band has been identified, the hypersensitive spot should be located by gently compressing spots along the taut band. Alongside palpation, clinicians should ask the following: ‘Which of the following spots is the most painful?’, ‘Is this pain part of your usual complaints?’, ‘Does the pain refer anywhere from the spot that I am compressing?’. An affirmative reply to the first question confirms the hypersensitive spot criteria. An affirmative reply to the second question confirms the pain recognition criteria; and finally, the third question confirms the presence of referred pain<ref>Barbero M, Schneebeli A, Koetsier E, Maino P. [https://journals.lww.com/co-supportiveandpalliativecare/FullText/2019/09000/Myofascial_pain_syndrome_and_trigger_points_.20.aspx Myofascial pain syndrome and trigger points: evaluation and treatment in patients with musculoskeletal pain]. Current opinion in supportive and palliative care. 2019 Sep 1;13(3):270-6.</ref>. | |||
== Outcome Measures == | == Outcome Measures == | ||
Fischer has proposed the use of a pressure threshold meter (algometer), as a means of quantitative documentation of TrPs, and for quantifying the effects of the physical therapy treatment. Pressure pain threshold and visual analogue scale (VAS) scores were the outcome measures | Fischer has proposed the use of a pressure threshold meter (algometer), as a means of quantitative documentation of TrPs, and for quantifying the effects of the physical therapy treatment. Pressure pain threshold and [[Visual Analogue Scale|visual analogue scale]] (VAS) scores were the outcome measures used in the analyzed trials. ROM also may be an outcome measurement for evaluating therapy<ref name="Fernandez 2005">de las Peñas CF, Campo MS, Carnero JF, Page JC. [https://www.sciencedirect.com/science/article/pii/S1360859203001062 Manual therapies in myofascial trigger point treatment: a systematic review]. Journal of bodywork and movement therapies. 2005 Jan 1;9(1):27-34.</ref>. | ||
== Medical Management == | == Medical Management == | ||
</div> | |||
=== Medications === | |||
<div> | |||
Milder forms of pain may be relieved by over-the-counter medications such as Tylenol (acetaminophen) or nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen. Both acetaminophen and NSAIDs relieve pain caused by muscle aches and stiffness, and additionally, NSAIDs reduce inflammation (swelling and irritation). If over-the-counter drugs do not provide relief, a doctor may prescribe muscle relaxants, anti-anxiety drugs (Valium), antidepressants (Cymbalta), NSAIDs such as Celebrex, or a short course of stronger painkillers (codeine), hydrocodone and acetaminophen (Vicodin)<ref>Persons O. [http://acclaimhealth.ca/wp-content/uploads/2019/01/Pain-Management-for-Older-Persons.pdf Pharmacological management of persistent pain in older persons]. J Am Geriatr Soc. 2009;57(8):1331-46.</ref>. | |||
</div> | |||
=== Trigger Point Injection (TPI) === | |||
<div> | |||
This is a procedure of inserting a small needle into the patient's active TrP. The injection contains a local anaesthetic or saline and may include a corticosteroid. With the injection, the TrP is made inactive and the pain is alleviated. Often, a brief course of treatment will result in sustained relief. Injections are performed by a physician and usually take a few minutes. Several sites may be injected in one visit. If a patient has an allergy to a certain drug, a dry-needle technique (involving no medications) can be used<ref>Simons DG. Myofascial pain syndrome due to trigger points. Ohio; 1983.</ref>. | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
* If possible, everyday-life factors that arouse the emergence of | * If possible, everyday-life factors that arouse the emergence of TrPs must be eliminated or reduced, | ||
* Posture training and education about postures and lifestyle | * Posture training and education about postures and lifestyle, | ||
* Passive stretching and / or Foam Roller stretching, few times a day | * Passive stretching and/or Foam Roller stretching, a few times a day, | ||
* Self-massage, few times a day, and especially Deep Stroking Massage | * Self-massage, a few times a day, and especially Deep Stroking Massage done rhythmically and in only one direction, | ||
* Strengthening: initially only isometric and then isotonic exercises, | * Strengthening: initially only isometric and then isotonic exercises, | ||
* Ischemic Compression Technique | * Ischemic Compression Technique - the term has been used to describe treatment in which ischemia is induced in the TrPt zone by applying sustained pressure. However, this principle is questionable, since the nucleus of the TrP intrinsically presents important hypoxia. Simons described a similar treatment modality, though without the need to induce additional ischemia in the TrP zone (TrP Pressure Release). The aim of this technique is to free the contracted sarcomeres within the TrP. The amount of pressure applied should suffice to produce gradual relaxation of the tension within the TrP zone, without causing pain. Yet both techniques show imitate significant improvement of the ROM after treatment<ref name="Grieve 2011">Grieve R, Clark J, Pearson E, Bullock S, Boyer C, Jarrett A. [https://www.sciencedirect.com/science/article/pii/S136085921000015X The immediate effect of soleus trigger point pressure release on restricted ankle joint dorsiflexion: A pilot randomised controlled trial]. Journal of bodywork and movement therapies. 2011 Jan 1;15(1):42-9.</ref><ref name="montanez 2010">Montañez-Aguilera FJ, Valtueña-Gimeno N, Pecos-Martín D, Arnau-Masanet R, Barrios-Pitarque C, Bosch-Morell F. [https://content.iospress.com/articles/journal-of-back-and-musculoskeletal-rehabilitation/bmr00255 Changes in a patient with neck pain after application of ischemic compression as a trigger point therapy]. Journal of back and musculoskeletal rehabilitation. 2010 Jan 1;23(2):101-4.</ref>. | ||
* Taping Technique, | * Taping Technique, | ||
* Spray and Stretch Technique by using ethyl chloride spray, | * Spray and Stretch Technique by using ethyl chloride spray, | ||
| Line 150: | Line 169: | ||
* Other proprioceptive neuromuscular techniques: Reciprocal Inhibition (RI), Post-Isometric Relaxation (PIR), Contract-Relax/Hold-Relax (CRHR), Contract-Relax/Antagonist Contract (CRAC), | * Other proprioceptive neuromuscular techniques: Reciprocal Inhibition (RI), Post-Isometric Relaxation (PIR), Contract-Relax/Hold-Relax (CRHR), Contract-Relax/Antagonist Contract (CRAC), | ||
* Some specific techniques like Neuromuscular Technique(NMT), Muscle Energy Technique (MET) and Myotherapy (MT), | * Some specific techniques like Neuromuscular Technique(NMT), Muscle Energy Technique (MET) and Myotherapy (MT), | ||
* | * Ultrasonography, Hot and Cold packs, Diathermy- Tecar therapy, Laser, Ionophoresis<ref name="Eduardo 2010" /><br> | ||
{| width="100%" cellspacing="1" cellpadding="1" | |||
|- | |||
|{{#ev:youtube|SQ5b2rqEZKg|300}} | |||
|{{#ev:youtube|woFDni1Eguw|300}} | |||
|} | |||
== Other | == Other Interventions == | ||
These are other possible therapies written in literature. Note: | These are other possible therapies written in the literature. Note: Not all of the themes have strong scientific evidence. A lot of the research are not placebo-controlled and immediate effects after treatment may occur due to placebo-effects<ref name="Fernandez 2005" />: | ||
* Dry Needling, | * [[Dry Needling|Dry Needling]], | ||
* Acupuncture, | * [[Acupuncture]], | ||
* Laser therapy, | * Laser therapy, | ||
* Prolotherapy (injecting solutions in region of TrPs: lidocaine, glycerine, phenol...)<br> | * Prolotherapy (injecting solutions in the region of TrPs: lidocaine, glycerine, phenol...).<br> | ||
== References == | == References == | ||
<references /></div> | <references /></div> | ||
[[Category:Vrije_Universiteit_Brussel_Project]] [[Category:Musculoskeletal/Orthopaedics|orthopaedics]] [[Category:Pain]] [[Category: | [[Category:Vrije_Universiteit_Brussel_Project]] | ||
[[Category:Musculoskeletal/Orthopaedics|orthopaedics]] | |||
[[Category:Pain]] | |||
[[Category:Interventions]] | |||
Latest revision as of 13:53, 29 January 2024
Original Editors -Sean Wautersas part of the Vrije Universiteit Brussel's Evidence-based Practice project.
Top Contributors - Sean Wauters, Milijana Delevic, Mathilde De Dobbeleer, Admin, Kim Jackson, WikiSysop, Uchechukwu Chukwuemeka, Aminat Abolade, Jonathan Wong, Lizzie Cotton, George Prudden, Benjamin Desmedt, Lucinda hampton and 127.0.0.1
Definition/Description[edit | edit source]
Jump sign is the characteristic behavioural response to pressure on a TrP. Individuals are frequently startled by the intense pain. They wince or cry out with a response seemingly out of proportion to the amount of pressure exerted by the examining fingers. They move involuntarily, jerking the shoulder, head, or some other part of the body not being palpated. A jump sign thus reflects the extreme tenderness of a TrP. This sign has been considered pathognomonic for the presence of TrPs.
Local twitch response - defined as a transient visible or palpable contraction of the muscle and skin as the tense muscle fibres contract when pressure is applied through needle penetration or by transverse snapping palpation. A local twitch response on stimulating active TrPs is a widely accepted diagnostic sign[5].
Referred pain, also called reflective pain, is pain perceived at a location other than the site of the painful stimulus. Pain is reproducible and does not follow dermatomes, myotomes, or nerve roots. There is no specific joint swelling or neurological deficits. Pain from a myofascial TrP is a distinct, discrete and constant pattern or map of pain with no gender or racial differences able to reproduce symptoms - referred pain map[6].
(Radiating pain is slightly different from referred pain; for example, the pain related to a myocardial infarction could either be referred or radiating pain from the chest. Referred pain is when the pain is located away from or adjacent to the organ involved; for instance, when a person has pain only in their jaw or left arm, but not in the chest)[1][7].
Anatomy and Etiology[edit | edit source]
Trigger points develop in the myofascia, mainly in the centre of a muscle belly where the motor endplate enters (primary or central TrPs)[6]. Those are palpable nodules within the tight muscle at the size of 2-10 mm and can be demonstrated at different places in any skeletal muscles of the body. We all have TrPs in the body. Can be present even in babies and children, but their presence does not necessarily result in the formation of pain syndrome. When it happens, TrPs are directly associated with myofascial pain syndrome*, somatic dysfunction, psychological disturbance and restricted daily functioning[8].
*Myofascial Pain Syndrome refers to regional pain of soft tissue origin and is associated with muscle tenderness that arises from TrPs, focal points of tenderness, a few millimetres in diameter, found at multiple sites in a muscle and the fascia of muscle tissue[9].
Causes - Usually, TrPs happen due to:
- Ageing,
- Injury sustained by a fall, by stress or birth trauma.
- Lack of exercise - commonly in sedentary persons between 27,5-55 years, of which 45% are men[10],
- Bad posture - upper and lower crossed pattern, swayback posture, telephone posture, cross-legged sitting,
- Muscle overuse and respective micro-trauma - weightlifting,
- Chronic stress condition - anxiety, depression, psychological stress trauma,
- Vitamin deficiencies - vitamin C, D, B; folic acid; iron;
- Sleep disturbance,
- Joint problems and hypermobility.
Classification of TrPs[edit | edit source]
TrPts can be divided into several groups[6]
Primary / Central and Secondary / Satellite Trigger Points[edit | edit source]
- Primary or Central TrPs are those that cause severe pain locally at the pressure with irradiation according to the referred pain map. Usually are based around the center of a muscle belly.
- Secondary or Satellite TrPs arise in response to existing central trigger points in surrounding muscles. They usually spontaneously withdraw when the central TrP is healed. Can be present in the form of a cluster.
Active and Inactive /Latent Trigger Points[edit | edit source]
- Active TrP is any point that causes tenderness and referred pain on palpation. Palpation may also cause autonomic symptoms such as skin redness, sweating, and dizziness[11].
- Latent TrP does not evoke pain spontaneously, and local or referred pain occurs only with strong digital pressure[12]. They may change muscle activation patterns or cause muscle weakness in pain-free patients[13][14].
- Reproduction of painful symptoms is the diagnostic criterion differentiating between the two[12].
Diffuse Trigger Points[edit | edit source]
- Commonly happens in case of severe postural deformity where initially primary TrPs are multiple, so secondary multiple TrPs are only a response of a mechanism, called diffuse.
Attachment Trigger Points[edit | edit source]
- Arise in tendo-osseous junctions which become very tender. If not treated, degenerative processes of an adjacent joint can spring up.
Ligamentous Trigger Points[edit | edit source]
- Even ligaments can develop trigger points. The presence of TrPs in the anterior longitudinal ligament of the spine can result in neck instability. Some knee pain syndromes are successfully healed when treated ligamentum patellae and fibular collateral ligament.
Pathogenesis and Theories[edit | edit source]
Little is known about the formation of TrPs. There are some theories written in literature that try to explain the formation, sensitization, and manifestation of TrPs, but few of them have strong evidence[3][15][16].
Under normal conditions, pain from TrPs is mediated by thin myelinated (Ad) fibres and unmyelinated (C) fibres. Various noxious and innocuous events, such as mechanical stimuli or chemical mediators, may excite and sensitize Ad fibres and C fibres and thereby play a role in the development of TrPs.
Integrated Trigger Point Hypothesis (ITPH) is the present working hypothesis. When sarcomeres and motor endplate become overactive for a number of different reasons, pathological changes start at cellular levels. This turns on permanently sarcomeres leading to a local inflammatory response, loss of oxygen supply, loss of nutrient supply, endogenous (involuntary) shortening of muscle fibres, and increased metabolic demand on local tissues. Electrophysiological investigations of TrPs reveal phenomena which indicate that the electrical activity arises from dysfunctional extrafusal motor endplates rather than from muscle spindles[17].
Polymodal theory explains the existence of polymodal receptors (PMRs) throughout the body which under certain constant, pathological stimuli turn into trigger points[18].
Radiculopathic theory explains the direct relationship between problems on nerve roots which lead to local and distant neurovascular signals and trigger points creation[19].
Peripheral and Central Sensitization - Central sensitization is a phenomenon, together with peripheral sensitization, which helps in understanding chronic or amplified pain. There is central sensitization after an intense or repetitive stimulus of the nociceptor present in the periphery, leading to a reversible increase of excitability and of the synaptic efficacy of central nociceptive pathway neurons. Manifested as hypersensitivity to pain (called tactile allodynia and hyperalgesia secondary to puncture or pressure). These CNS changes may be detected by electrophysiological or imaging techniques[20][21].
Differential Diagnosis[edit | edit source]
- Fibromyalgia - characterized by diffused fatigue and aches all over the body. More often in women, does not involve joints but does involve all other tissues (muscle, bone, tendon, ligaments, and fat) and can develop tender points. Tender points are discrete areas of tenderness over soft tissues that cause local pain and are tender to palpation but patients do not present jump signs when pressed nor referred pain maps. These two pain syndromes may overlap in symptoms and are difficult to differentiate without a thorough exam by a skilled physician. Although they may be concomitant and may interact with one another[2][10].
Other conditions which include muscle pain and trigger points:
- Musculoskeletal Diseases
- Occupational myalgias
- Post-traumatic hyperirritability syndrome
- Joint dysfunction (osteoarthritis)
- Tendonitis and bursitis
- Neurological Disorders
- Trigeminal neuralgia
- Glossopharyngeal neuralgia
- Sphenopalatine neuralgia
- Systemic Diseases
- Systemic lupus erythematosus (SLE)
- Rheumatoid arthritis
- Gout
- Psoriatic arthritis
- Infections (viral, bacterial, protozoan, parasitic and Candida albicans infection)
- Lyme Disease
- Hypoglycemia and Hypothyroidism
- Heterotopic Pain of Central Origin
- Axis II-Type Disorders
- Psychogenic pain
- Painful behaviours
Symptoms and Clinical Findings[edit | edit source]
- A patient usually asks for help due to a chronic pain state (e.g.: headaches, aches everywhere, morning stiffness, TMJ syndrome, tinnitus...), which, in reality, is often physically away from the active trigger point.
- Muscle weakness or imbalance, altered motor recruitment, in either the affected muscle or in functionally related muscles.
- Changes in Range of Motion (ROM).
- Painful movement and/or movement that sometimes can exacerbate symptoms.
- Tension headaches, migraines, tinnitus, temporomandibular joint problems... as accompanying symptoms.
- Postural abnormalities and compensations.
Diagnostic Procedures[edit | edit source]
Palpation[edit | edit source]
Palpation remains the current standard for diagnosis and assessment of TrPs and is the standard against which new diagnostic methods are assessed[22]. However, interrater reliability estimates for palpation vary widely, suggesting palpation is unreliable[23].
Imaging[edit | edit source]
Imaging modalities have recently shown potential to identify TrPs:
Sonoelastography was able to detect differences between clinically relevant groups and identify TrPs. It is hypothesized that vibration sonoelastography and shear wave elastography have more reliable results due to their use of mechanically-induced stimuli[22].
Anamnesis[edit | edit source]
Anamnesis (a patient's account of their own clinical history) should be specific. The patient must be asked about fibromyalgia, as well as the presence of it in the family history of diseases. Also, the patient should be asked about his physical and daily activities in the present and in the past as a lack of exercise and sedentary life may be a pathogenic factor. Furthermore, chronic muscle overuse, daily stress, medications (and their overuse), and sleep disturbances have to be asked about and examined in detail.
Examination[edit | edit source]
In 2018, an international Delphi panel revised the TrP diagnostic approach and proposed that at least two of the following criteria must be present: a taut band, a hypersensitive spot, and referred pain.
Palpation should be performed by moving the fingertips forward and backwards, perpendicular to the muscle fibres. Alternatively, some muscles can be palpated using a pincer grip. Once the taut band has been identified, the hypersensitive spot should be located by gently compressing spots along the taut band. Alongside palpation, clinicians should ask the following: ‘Which of the following spots is the most painful?’, ‘Is this pain part of your usual complaints?’, ‘Does the pain refer anywhere from the spot that I am compressing?’. An affirmative reply to the first question confirms the hypersensitive spot criteria. An affirmative reply to the second question confirms the pain recognition criteria; and finally, the third question confirms the presence of referred pain[24].
Outcome Measures[edit | edit source]
Fischer has proposed the use of a pressure threshold meter (algometer), as a means of quantitative documentation of TrPs, and for quantifying the effects of the physical therapy treatment. Pressure pain threshold and visual analogue scale (VAS) scores were the outcome measures used in the analyzed trials. ROM also may be an outcome measurement for evaluating therapy[25].
Medical Management[edit | edit source]
Medications[edit | edit source]
Milder forms of pain may be relieved by over-the-counter medications such as Tylenol (acetaminophen) or nonsteroidal anti-inflammatory drugs (NSAIDs) such as aspirin, ibuprofen, and naproxen. Both acetaminophen and NSAIDs relieve pain caused by muscle aches and stiffness, and additionally, NSAIDs reduce inflammation (swelling and irritation). If over-the-counter drugs do not provide relief, a doctor may prescribe muscle relaxants, anti-anxiety drugs (Valium), antidepressants (Cymbalta), NSAIDs such as Celebrex, or a short course of stronger painkillers (codeine), hydrocodone and acetaminophen (Vicodin)[26].
Trigger Point Injection (TPI)[edit | edit source]
This is a procedure of inserting a small needle into the patient's active TrP. The injection contains a local anaesthetic or saline and may include a corticosteroid. With the injection, the TrP is made inactive and the pain is alleviated. Often, a brief course of treatment will result in sustained relief. Injections are performed by a physician and usually take a few minutes. Several sites may be injected in one visit. If a patient has an allergy to a certain drug, a dry-needle technique (involving no medications) can be used[27].
Physical Therapy Management[edit | edit source]
- If possible, everyday-life factors that arouse the emergence of TrPs must be eliminated or reduced,
- Posture training and education about postures and lifestyle,
- Passive stretching and/or Foam Roller stretching, a few times a day,
- Self-massage, a few times a day, and especially Deep Stroking Massage done rhythmically and in only one direction,
- Strengthening: initially only isometric and then isotonic exercises,
- Ischemic Compression Technique - the term has been used to describe treatment in which ischemia is induced in the TrPt zone by applying sustained pressure. However, this principle is questionable, since the nucleus of the TrP intrinsically presents important hypoxia. Simons described a similar treatment modality, though without the need to induce additional ischemia in the TrP zone (TrP Pressure Release). The aim of this technique is to free the contracted sarcomeres within the TrP. The amount of pressure applied should suffice to produce gradual relaxation of the tension within the TrP zone, without causing pain. Yet both techniques show imitate significant improvement of the ROM after treatment[28][29].
- Taping Technique,
- Spray and Stretch Technique by using ethyl chloride spray,
- Manual Lymphatic Drainage (MLD), since the presence of TrPs obstacle lymphatic flow,
- Other proprioceptive neuromuscular techniques: Reciprocal Inhibition (RI), Post-Isometric Relaxation (PIR), Contract-Relax/Hold-Relax (CRHR), Contract-Relax/Antagonist Contract (CRAC),
- Some specific techniques like Neuromuscular Technique(NMT), Muscle Energy Technique (MET) and Myotherapy (MT),
- Ultrasonography, Hot and Cold packs, Diathermy- Tecar therapy, Laser, Ionophoresis[10]
Other Interventions[edit | edit source]
These are other possible therapies written in the literature. Note: Not all of the themes have strong scientific evidence. A lot of the research are not placebo-controlled and immediate effects after treatment may occur due to placebo-effects[25]:
- Dry Needling,
- Acupuncture,
- Laser therapy,
- Prolotherapy (injecting solutions in the region of TrPs: lidocaine, glycerine, phenol...).
References[edit | edit source]
- ↑ 1.0 1.1 Simons DG, Travell JG, Simons LS. Travell & Simons' myofascial pain and dysfunction: upper half of body. Lippincott williams & wilkins; 1999.
- ↑ 2.0 2.1 Alvarez DJ, Rockwell PG. Trigger points: diagnosis and management. American family physician. 2002 Feb 15;65(4):653.
- ↑ 3.0 3.1 Davidoff RA. Trigger points and myofascial pain: toward understanding how they affect headaches. Cephalalgia. 1998 Sep;18(7):436-48.
- ↑ Vázquez Delgado E, Cascos-Romero J, Gay Escoda C. Myofascial pain syndrome associated with trigger points: a literature review.(I): Epidemiology, clinical treatment and etiopathogeny. Medicina Oral, Patología Oral y Cirugia Bucal, 2009, vol. 14, num. 10, p. 494-498. 2009 Oct 1.
- ↑ Yap EC. Myofascial pain-an overview. Annals-Academy of Medicine Singapore. 2007 Jan 1;36(1):43.
- ↑ 6.0 6.1 6.2 Niel-Asher S. The concise book of trigger points: A professional and self-help manual. North Atlantic Books; 2014 Sep 16.
- ↑ Ray BS, Wolff HG. Experimental studies on headache: pain-sensitive structures of the head and their significance in headache. Archives of surgery. 1940 Oct 1;41(4):813-56.
- ↑ Simons DG, Travell JG, Simons LS. Travell & Simons' myofascial pain and dysfunction: upper half of body. Lippincott williams & wilkins; 1999.
- ↑ Jantos M. Understanding chronic pelvic pain. Pelviperineology. 2007 Jun 1;26(2):66.
- ↑ 10.0 10.1 10.2 Vázquez Delgado E, Cascos-Romero J, Gay Escoda C. Myofascial pain associated to trigger points: a literature review. Part 2: differential diagnosis and treatment. Medicina Oral, Patología Oral y Cirugia Bucal, 2010, vol. 15, num. 4, p. 639-643. 2010 Jul 1.
- ↑ Pringle K. Myofascial Pain and Dysfunction: The Trigger Point Manual. Journal of Manipulative & Physiological Therapeutics. 1999 Jun 1;22(5):A1.
- ↑ 12.0 12.1 Fernández-de-Las-Peñas C, Dommerholt J. International consensus on diagnostic criteria and clinical considerations of myofascial trigger points: a Delphi study. Pain Medicine. 2018 Jan 1;19(1):142-50.
- ↑ Ge HY, Monterde S, Graven-Nielsen T, Arendt-Nielsen L. Latent Myofascial Trigger Points Are Associated With an Increased Intramuscular Electromyographic Activity During Synergistic Muscle Activation. The journal of pain. 2014;15(2):181–7.
- ↑ Celik D, Yeldan İ. The relationship between latent trigger point and muscle strength in healthy subjects: a double-blind study. Journal of Back and Musculoskeletal Rehabilitation. 2011 Jan 1;24(4):251-6.
- ↑ Delgado EV, Romero JC, Gay-Escoda C. Myofascial pain syndrome associated with trigger points: A literature review.(I): Epidemiology, clinical treatment and etiopathogeny. Medicina oral, patología oral y cirugía bucal. Ed. inglesa. 2009;14(10):1.
- ↑ Tough EA, White AR, Cummings TM, Richards SH, Campbell JL. Acupuncture and dry needling in the management of myofascial trigger point pain: a systematic review and meta-analysis of randomised controlled trials. European Journal of Pain. 2009 Jan 1;13(1):3-10.
- ↑ Simons DG. Clinical and etiological update of myofascial pain from trigger points. Journal of musculoskeletal pain. 1996 Jan 1;4(1-2):93-122.
- ↑ Kawakita K, Itoh K, Okada K. The polymodal receptor hypothesis of acupuncture and moxibustion, and its rational explanation of acupuncture points. InInternational Congress Series 2002 Aug 1 (Vol. 1238, pp. 63-68). Elsevier.
- ↑ Gunn CC, Wall PD. The Gunn approach to the treatment of chronic pain: intramuscular stimulation for myofascial pain of radiculopathic origin. Churchill Livingstone; 1996.
- ↑ Fernández-de-las-Peñas C, Cuadrado ML, Arendt-Nielsen L, Simons DG, Pareja JA. Myofascial trigger points and sensitization: an updated pain model for tension-type headache. Cephalalgia. 2007 May;27(5):383-93.
- ↑ Woolf CJ. Central sensitization: implications for the diagnosis and treatment of pain. pain. 2011 Mar 1;152(3):S2-15.
- ↑ 22.0 22.1 Mazza DF, Boutin RD, Chaudhari AJ. Assessment of myofascial trigger points via imaging: a systematic review. American Journal of Physical Medicine & Rehabilitation. 2021 Oct 1;100(10):1003-14.
- ↑ Rathbone AT, Grosman-Rimon L, Kumbhare DA. Interrater agreement of manual palpation for identification of myofascial trigger points. The Clinical journal of pain. 2017 Aug 1;33(8):715-29.
- ↑ Barbero M, Schneebeli A, Koetsier E, Maino P. Myofascial pain syndrome and trigger points: evaluation and treatment in patients with musculoskeletal pain. Current opinion in supportive and palliative care. 2019 Sep 1;13(3):270-6.
- ↑ 25.0 25.1 de las Peñas CF, Campo MS, Carnero JF, Page JC. Manual therapies in myofascial trigger point treatment: a systematic review. Journal of bodywork and movement therapies. 2005 Jan 1;9(1):27-34.
- ↑ Persons O. Pharmacological management of persistent pain in older persons. J Am Geriatr Soc. 2009;57(8):1331-46.
- ↑ Simons DG. Myofascial pain syndrome due to trigger points. Ohio; 1983.
- ↑ Grieve R, Clark J, Pearson E, Bullock S, Boyer C, Jarrett A. The immediate effect of soleus trigger point pressure release on restricted ankle joint dorsiflexion: A pilot randomised controlled trial. Journal of bodywork and movement therapies. 2011 Jan 1;15(1):42-9.
- ↑ Montañez-Aguilera FJ, Valtueña-Gimeno N, Pecos-Martín D, Arnau-Masanet R, Barrios-Pitarque C, Bosch-Morell F. Changes in a patient with neck pain after application of ischemic compression as a trigger point therapy. Journal of back and musculoskeletal rehabilitation. 2010 Jan 1;23(2):101-4.






