Traditional Physiotherapy Interventions for Pain Conditions: Difference between revisions
mNo edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (20 intermediate revisions by 9 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editor '''- [[User:Kudzanayi Ronald Muzenda|Kudzanayi Ronald Muzenda]] and [[User:Jo Etherton|Jo Etherton]] | '''Original Editor '''- [[User:Kudzanayi Ronald Muzenda|Kudzanayi Ronald Muzenda]] and [[User:Jo Etherton|Jo Etherton]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
= Traditional Physiotherapy Modalities = | == Traditional Physiotherapy Modalities == | ||
== Electrotherapy == | === Electrotherapy === | ||
The term electrotherapy and electrophyical agents have been used interchangeably to describe the modalities used in physiotherapy. Some suggest that the term electrotherapy implies modalities that use electric current only in treatment. | The term electrotherapy and electrophyical agents have been used interchangeably to describe the modalities used in physiotherapy. Some suggest that the term electrotherapy implies modalities that use electric current only in treatment. | ||
| Line 27: | Line 18: | ||
=== Electrical Stimulation === | === Electrical Stimulation === | ||
==== Transcutaneous Electrical Stimulation ==== | |||
The exact mechanism of electrical stimulation’s beneficial effect remains controversial. Electrical stimulation is said directly block pain signals from reaching the brain so that the patient never experiences them. In addition, electrical stimulation has been shown to promote the release of endorphins which are natural painkillers produced by the body.Pain reduction occurs because the applied electrical fields act to close the body's "pain gate mechanism"TENS ( Transcutaneous Electrical Nerve Stimulation) is the widely used electrical modality for chronic pain.<br> | |||
The exact mechanism of electrical stimulation’s beneficial effect remains controversial. Electrical stimulation is said directly block pain signals from reaching the brain so that the patient never experiences them. In addition, electrical stimulation has been shown to promote the release of endorphins which are natural painkillers produced by the body.Pain reduction occurs because the applied electrical fields act to close the body's "pain gate mechanism"TENS ( Transcutaneous Electrical Nerve Stimulation) is the widely used | |||
The video shows how TENS work: | The video shows how TENS work: | ||
| Line 35: | Line 25: | ||
{{#ev:youtube|eYquxPVE_MI|300}} | {{#ev:youtube|eYquxPVE_MI|300}} | ||
In a Cochrane systematic Review by Johnson et al 2015<ref name="John">Johnson MI, Paley CA, Howe TE, Sluka KA. Transcutaneous electrical nerve stimulation for acute pain. Cochrane Database of Systematic Reviews 2015, Issue 6. Art. No.: CD006142. DOI: 10.1002/14651858.CD006142.pub3</ref> based on the six of the 19 trials TENS was found to be better than placebo TENS (delivering no electrical current) at reducing the intensity of acute pain but the reduction in pain was not consistent across all trials. There was an insufficient number patients to make a firm conclusion.More is research is needed to solidfy the evidence.For more information about TENS follow this link:[[Transcutaneous Electrical Nerve Stimulation (TENS)]] | In a Cochrane systematic Review by Johnson et al 2015<ref name="John">Johnson MI, Paley CA, Howe TE, Sluka KA. Transcutaneous electrical nerve stimulation for acute pain. Cochrane Database of Systematic Reviews 2015, Issue 6. Art. No.: CD006142. DOI: 10.1002/14651858.CD006142.pub3</ref> based on the six of the 19 trials TENS was found to be better than placebo TENS (delivering no electrical current) at reducing the intensity of acute pain but the reduction in pain was not consistent across all trials. There was an insufficient number patients to make a firm conclusion.More is research is needed to solidfy the evidence.For more information about TENS follow this link:[[Transcutaneous Electrical Nerve Stimulation (TENS)]]<br> | ||
<br | |||
==== Interferential Therapy ==== | |||
Interferential therapy is a more deeper form of electical stimulation and is more comfortable to the patient.The following link provides more information on how it works:{{pdf|IFT.pdf|Interferential Therapy}} | Interferential therapy is a more deeper form of electical stimulation and is more comfortable to the patient.The following link provides more information on how it works:{{pdf|IFT.pdf|Interferential Therapy}} | ||
| Line 49: | Line 36: | ||
=== Thermal Agents === | === Thermal Agents === | ||
When applied in successive fashion, heat and cold are believed to exert a physiological effect on your body's pain gate mechanism, which temporarily alters pain signals traveling to and from your brain. This temporary reduction in pain is a welcome relief for those suffering long-standing complaints of the nervous and musculoskeletal systems. | When applied in successive fashion, heat and cold are believed to exert a physiological effect on your body's pain gate mechanism, which temporarily alters pain signals traveling to and from your brain. This temporary reduction in pain is a welcome relief for those suffering long-standing complaints of the nervous and musculoskeletal systems. Cryotherapy (Cold therapy) works for pain by eliciting the body’s “fight or flight” response which stimulates the production of endorphins, thus decreasing the body’s perception of symptomatic pain | ||
Thermal agents can be divided into two i.e | Thermal agents can be divided into two i.e | ||
| Line 64: | Line 51: | ||
{{#ev:youtube|snXBG-gIXe8|300}}<ref name="you1">https://www.youtube.com/watch?v=snXBG-gIXe8 Accessed 30/04/2016</ref> | {{#ev:youtube|snXBG-gIXe8|300}}<ref name="you1">https://www.youtube.com/watch?v=snXBG-gIXe8 Accessed 30/04/2016</ref> | ||
There is moderate evidence<ref name="heat">French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ. Superficial heat or cold for low back pain. Cochrane Database of Systematic Reviews 2006, Issue 1. Art. No.: CD004750. DOI: 10.1002/14651858.CD004750.pub2</ref> that heat therapy reduces pain and disability for patients with back pain that lasts for less than three months. The relief has only been shown to occur for a short time and the effect is relatively small. The addition of exercise to heat wrap therapy appears to provide additional benefit. There is still not enough evidence about the effect of the application of cold for low-back pain of any duration, or for heat for back pain that lasts longer than three months. | |||
There is moderate evidence<ref name="heat">French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ. Superficial heat or cold for low back pain. Cochrane Database of Systematic Reviews 2006, Issue 1. Art. No.: CD004750. DOI: 10.1002/14651858.CD004750.pub2</ref> that heat therapy reduces pain and disability for patients with back pain that lasts for less than three months. The relief has only been shown to occur for a short time and the effect is relatively small. The addition of exercise to heat wrap therapy appears to provide additional benefit. There is still not enough evidence about the effect of the application of cold for low-back pain of any duration, or for heat for back pain that lasts longer than three months. | |||
=== Non-Thermal Agents === | === Non-Thermal Agents === | ||
| Line 74: | Line 57: | ||
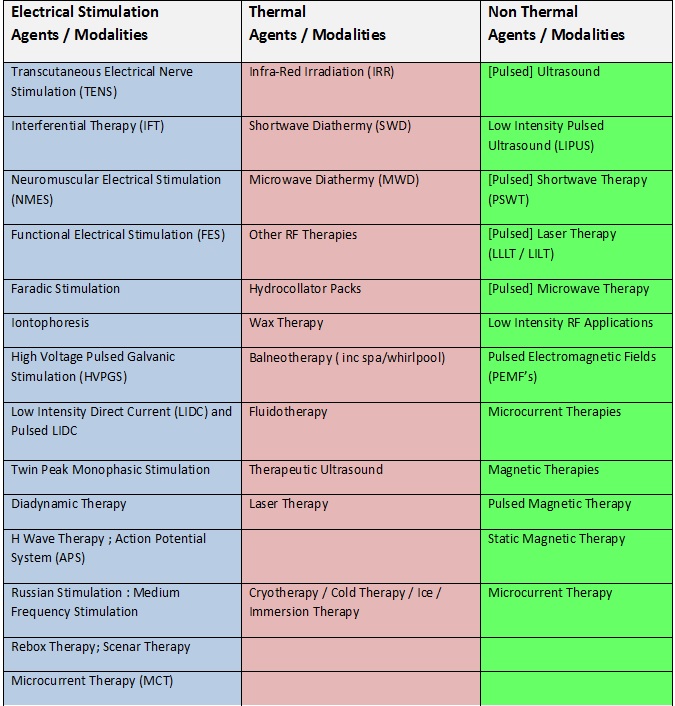
Non Thermal agents do not make use of heat/cold to exert a therapeutic effect.Examples of these are shown in the table above.The following links give information about the physiological effect,mechanism of action and evidence in pain a management to the most common non thermal agents : | Non Thermal agents do not make use of heat/cold to exert a therapeutic effect.Examples of these are shown in the table above.The following links give information about the physiological effect,mechanism of action and evidence in pain a management to the most common non thermal agents : | ||
[[Ultrasound | [[Therapeutic Ultrasound]] | ||
[http://www.electrotherapy.org/modality/laser-therapy Low Level Laser Therapy (LLLT)] | [http://www.electrotherapy.org/modality/laser-therapy Low Level Laser Therapy (LLLT)] | ||
| Line 80: | Line 63: | ||
[http://www.electrotherapy.org/modality/magnetic-therapy#Pain%20Relief Magnetic Therapy] | [http://www.electrotherapy.org/modality/magnetic-therapy#Pain%20Relief Magnetic Therapy] | ||
In a systematic review by Yousefi-Nooraie (2008)<ref name="you">Yousefi‐Nooraie R, Schonstein E, Heidari K, Rashidian A, Pennick V, Akbari‐Kamrani M, Irani S, Shakiba B, Mortaz Hejri S, Jonaidi AR, Mortaz‐Hedjri S. Low level laser therapy for nonspecific low‐back pain. The Cochrane Library.</ref> which comprised of seven studies with a total of 384 people with non-specific LBP of varying durations. “Three of the studies (168 people) separately showed that Low level laser Therapy (LLLT) was more effective at reducing pain in the short-term (less than three months), and intermediate-term (six months) than sham (fake) laser. However, the strength and number of treatments were varied and the amount of the pain reduction was small. Three studies (102 people) separately reported that LLLT with exercise was not better than exercise alone or exercise plus sham in short-term pain reduction.” | |||
In a systematic review by Yousefi-Nooraie (2008)<ref name="you">Yousefi‐Nooraie R, Schonstein E, Heidari K, Rashidian A, Pennick V, Akbari‐Kamrani M, Irani S, Shakiba B, Mortaz Hejri S, Jonaidi AR, Mortaz‐Hedjri S. Low level laser therapy for nonspecific low‐back pain. The Cochrane Library.</ref> which comprised of seven studies with a total of 384 people with non-specific LBP of varying durations. “Three of the studies (168 people) separately showed that Low level laser Therapy (LLLT) was more effective at reducing pain in the short-term (less than three months), and intermediate-term (six months) than sham (fake) laser. However, the strength and number of treatments were varied and the amount of the pain reduction was small. Three studies (102 people) separately reported that LLLT with exercise was not better than exercise alone or exercise plus sham in short-term pain reduction.” | |||
== Manual Therapy == | |||
Manual therapy can be broadly defined as | Manual therapy can be broadly defined as | ||
<ref name="Led">Lederman E. The Science and Practice of Manual therapy. 2nd ed. Elsevier: London. (2005)</ref> | <ref name="Led">Lederman E. The Science and Practice of Manual therapy. 2nd ed. Elsevier: London. (2005)</ref> | ||
"...the useof hands in a curative and healing manner or a hands-on technique with therapeutic intent..." .It can be divided into two groups i.e Soft tissue techniques and Joint techniques | "...the useof hands in a curative and healing manner or a hands-on technique with therapeutic intent..." .It can be divided into two groups i.e Soft tissue techniques and Joint techniques<br> | ||
Soft tissue | === Soft Tissue Techniques === | ||
Soft tissue - This is directed at morphologically shortened muscles and/or restricted fascial mobility Techniques includes the following ( list is not exhaustive):<br> | |||
*Myofascial techniques | *Myofascial techniques | ||
| Line 108: | Line 83: | ||
*Active release therapy | *Active release therapy | ||
*Graston | *Graston | ||
*massage | |||
*MFR, | |||
*rolfing, | |||
*self massage with tennis balls or even foam rolling. This is directed at morphologically shortened muscles and/or restricted fascial mobility. | |||
=== Stretch === | |||
This includes neural mobilization, joint stretching, and/or muscular stretching. | |||
Often there is an impairment in rotation(osteokinematics) and possibly an abnormal IAR. There is a need to restore tensile length and or tolerance for tensile load (distracting forces). | |||
=== Joint Techniques === | |||
Joint techniques includes the following (list not exhaustive): | |||
*Joint Mobilisation | *Joint Mobilisation | ||
*Muscle energy techniques | *Muscle energy techniques | ||
| Line 120: | Line 100: | ||
*Traction | *Traction | ||
Manual therapy | === Manual Therapy Guidelines === | ||
* [[APA Clinical guide to safe manual therapy practice in the cervical spine 2017]] | |||
* [[Neck Pain: Clinical Practice Guidelines]] | |||
=== Mobilization === | === Mobilization === | ||
A detailed explaination of Mobilisation and its effect on pain can be read on this Physiopedia page: '''[http://www.physio-pedia.com/Maitland's_Mobilisations Maitlands Mobilisations]''' There is no convincing evidence indicating whether mobiisations or manipulation are more effective than each other<ref name="Gro">A. R. Gross*w, T. M. Kayz, C. Kennedyz}, D. Gasner}fckLR, L. Hurleyz8, K. Yardley**, L. Hendryww, L. McLaughlin: Clinical practice guideline on the use of manipulation or mobilization in the treatment of adults with mechanical neck disorders: Manual Therapy (2002) 7(4), 193–205</ref>. However regardless of this there is indication that neither of these therapies should be used in isolation, but as part of a wider treatment plan, mainly involving exercise. | A detailed explaination of Mobilisation and its effect on pain can be read on this Physiopedia page: '''[http://www.physio-pedia.com/Maitland's_Mobilisations Maitlands Mobilisations]''' There is no convincing evidence indicating whether mobiisations or manipulation are more effective than each other<ref name="Gro">A. R. Gross*w, T. M. Kayz, C. Kennedyz}, D. Gasner}fckLR, L. Hurleyz8, K. Yardley**, L. Hendryww, L. McLaughlin: Clinical practice guideline on the use of manipulation or mobilization in the treatment of adults with mechanical neck disorders: Manual Therapy (2002) 7(4), 193–205</ref>. However regardless of this there is indication that neither of these therapies should be used in isolation, but as part of a wider treatment plan, mainly involving exercise. | ||
=== Manipulation === | === Manipulation === | ||
| Line 156: | Line 129: | ||
Acupuncture is widely used by physiotherapist for the management of pain. There is much that we still need to understand about its exact mechanisms, however patients often report anecdotal evidence of its benefits. Take a look at this physiopedia page on [http://www.physio-pedia.com/Acupuncture Acupuncture]. | Acupuncture is widely used by physiotherapist for the management of pain. There is much that we still need to understand about its exact mechanisms, however patients often report anecdotal evidence of its benefits. Take a look at this physiopedia page on [http://www.physio-pedia.com/Acupuncture Acupuncture]. | ||
The introduction of the acupuncture needle produces a numb, aching sensation called "DE QI" that is thought to be esssential for the effectiveness of the treatment. It is thought that this sensation contributes to the activation of the endogenous antinociceptive system. Bowsher(98)<ref name="Bow">Bowsher(98) The Physiology ofstimulation produced analgesia. Journal of British medical Acupuncture society.IX(2) 58-62</ref> and Wang(85)<ref name="Wan">Wang AA(85) A study on the receptive fields of Acupuncture points and the relationship between characteristics of needling sensation and groups of afferent fibres. Scientific Sinica 28: 963-971</ref>theorised that De Qi is due to the activation of A delta fibres type I and III and the C-fibres releasing opioids in the dorsal horn. | The introduction of the acupuncture needle (also known as a solid filiform needle) produces a numb, aching sensation called "DE QI" that is thought to be esssential for the effectiveness of the treatment. It is thought that this sensation contributes to the activation of the endogenous antinociceptive system. Bowsher(98)<ref name="Bow">Bowsher(98) The Physiology ofstimulation produced analgesia. Journal of British medical Acupuncture society.IX(2) 58-62</ref> and Wang(85)<ref name="Wan">Wang AA(85) A study on the receptive fields of Acupuncture points and the relationship between characteristics of needling sensation and groups of afferent fibres. Scientific Sinica 28: 963-971</ref>theorised that De Qi is due to the activation of A delta fibres type I and III and the C-fibres releasing opioids in the dorsal horn. | ||
Despite acupuncture being widely used and reported as being helpful, it is disappointing that there is a lack of evidence to support this. | Despite acupuncture being widely used and reported as being helpful, it is disappointing that there is a lack of evidence to support this. | ||
| Line 164: | Line 137: | ||
There are other reports that indicate that the evidence base for acupuncture is widening however such as this report by Ernst. | There are other reports that indicate that the evidence base for acupuncture is widening however such as this report by Ernst. | ||
{{pdf|acupuncture2.pdf|Acupuncture-the evidence base is changing}} | {{pdf|acupuncture2.pdf|Acupuncture-the evidence base is changing}} | ||
=== Re-train/Re-education === | |||
Postural re-education and movement retraining are the focus here. If you bill neuromuscular re-education, this likely falls under “retraining”. Balance and gait training also fall in this category. | |||
=== Educate === | |||
This patient must change modify their current activities (they themselves may be preventing a healing response). Poor habits (lack of exercise, nutrition, vices such as smoking affecting intrinsic healing potential). They may need temporary or permanent changes to their lifestyle. This may include a cardiopulmonary exercise program (walking, biking, swimming program). This is NOT neuromuscular re-education, gait training, etc. | |||
=== Offload === | |||
Bracing & taping are primary examples. This may also include self-traction at home for primary decompression issues. This patient often has poor tolerance for tissue loading, and therefore this treatment is directly aimed at increasing tolerance. This may include positioning that optimizes blood flow(abduction pillow for RTC repair). | |||
=== Inhibition === | |||
This includes Grade I and II joint mobilization for pain dominant joints and spinal segments. The goal is generally NOT to restore joint translation (arthrokinematics) via tissue deformation of collagenous structures. This patient generally presents with excessive spasm and guarding. This may also include post-isometric relaxation which is focusing on resetting the resting tone of the muscle spindle, it may be physiologically shortened (as opposed to morphologically shortened). The patient may also need cognitive behavioral/psycho-social strategies such as relaxation to progress mobility, function, and/or pain control. | |||
=== Strengthen/Stabilize === | |||
This includes stabilization of the muscular system through exercise. The goal of this is to improve cross-sectional area and either maximum force generating capacity of that tissue and/or the endurance of that particular tissue. This tissue usually does not have a high level of intolerance and therefore the focus is on increasing the optimal loading zone and the capacity for absorbing and or creating force. | |||
Traditional Physiotherapy pain modalities can be | Addtionally, stabilization is commonly utilized during a spondylolisthesis patho-anatomic hypothesis (shear dysfunction) and may be confirmed with segmental testing and/or radiography. You may feel a large neutral zone (laxity) with facet gliding at the L4/5 segment and therefore need to stabilize this segment. | ||
== Integration with Other Pain Treatment Approaches. == | |||
Traditional Physiotherapy pain modalities can be integrated with other pain approaches i.e Pharmacological,Psychological,Exercise and Behavioural.There is little to no evidence on this subjcect more reasearch is warranted.<br> | |||
The articles below give an insight regarding pain treatment approach integration: | The articles below give an insight regarding pain treatment approach integration: | ||
| Line 183: | Line 176: | ||
controlled trial protocol}}<ref name="inte">http://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-13-129</ref> | controlled trial protocol}}<ref name="inte">http://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-13-129</ref> | ||
For more information about | For more information about other approaches follow the links below: | ||
[[Pharmacology in Pain Management]] | [[Pharmacology in Pain Management]] | ||
| Line 191: | Line 184: | ||
[[Psychological approaches to pain management]] | [[Psychological approaches to pain management]] | ||
[[Exercise and Activity in Pain Management]] | [[Exercise and Activity in Pain Management]] | ||
== Additional Resources == | == Additional Resources == | ||
{{pdf|Key Concepts in Electrotherapy March 2014.pdf|Key Concepts in Electrotherapy}}<ref>http://www.electrotherapy.org/assets/Downloads/Key%20Concepts%20in%20Electrotherapy%20March%202014.pdf accessed 2/24/2106</ref> | |||
[http://www.electrotherapy.org/ www.electrotherapy.org/] | [http://www.electrotherapy.org/ www.electrotherapy.org/] | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Pain]] [[Category:Manual_Therapy]] [[Category: | [[Category:Pain]] | ||
[[Category:Manual_Therapy]] | |||
[[Category:Interventions]] | |||
[[Category:PPA_Project]] | |||
Latest revision as of 12:53, 2 May 2024
Original Editor - Kudzanayi Ronald Muzenda and Jo Etherton
Top Contributors - Kudzanayi Ronald Muzenda, Joanne Garvey, Kim Jackson, Evan Thomas, Simisola Ajeyalemi, Lauren Lopez, Jo Etherton, WikiSysop, Lucinda hampton, Jess Bell, Yigit Unalan and Rachael Lowe
Traditional Physiotherapy Modalities[edit | edit source]
Electrotherapy[edit | edit source]
The term electrotherapy and electrophyical agents have been used interchangeably to describe the modalities used in physiotherapy. Some suggest that the term electrotherapy implies modalities that use electric current only in treatment.
The following table categorizes various modalities into three groups, i.e. electrical stimulation agents, thermal agents, and non-thermal agents[1]
Electrical stimulation agents and thermal agents are the most used in physiotherapy pain management. However, non-thermal agents, such as pulsed ultrasound, have been reported as having an analgesic effect.
Electrical Stimulation[edit | edit source]
Transcutaneous Electrical Stimulation[edit | edit source]
The exact mechanism of electrical stimulation’s beneficial effect remains controversial. Electrical stimulation is said directly block pain signals from reaching the brain so that the patient never experiences them. In addition, electrical stimulation has been shown to promote the release of endorphins which are natural painkillers produced by the body.Pain reduction occurs because the applied electrical fields act to close the body's "pain gate mechanism"TENS ( Transcutaneous Electrical Nerve Stimulation) is the widely used electrical modality for chronic pain.
The video shows how TENS work:
In a Cochrane systematic Review by Johnson et al 2015[2] based on the six of the 19 trials TENS was found to be better than placebo TENS (delivering no electrical current) at reducing the intensity of acute pain but the reduction in pain was not consistent across all trials. There was an insufficient number patients to make a firm conclusion.More is research is needed to solidfy the evidence.For more information about TENS follow this link:Transcutaneous Electrical Nerve Stimulation (TENS)
Interferential Therapy[edit | edit source]
Interferential therapy is a more deeper form of electical stimulation and is more comfortable to the patient.The following link provides more information on how it works:Interferential Therapy
In a systematic review by Jorge et al 2010 Interferential current therapy was foundto be more effective in reducing musculoskeletal pain better than a control treatment at discharge and more effective han placebo at a three month follow up
Thermal Agents[edit | edit source]
When applied in successive fashion, heat and cold are believed to exert a physiological effect on your body's pain gate mechanism, which temporarily alters pain signals traveling to and from your brain. This temporary reduction in pain is a welcome relief for those suffering long-standing complaints of the nervous and musculoskeletal systems. Cryotherapy (Cold therapy) works for pain by eliciting the body’s “fight or flight” response which stimulates the production of endorphins, thus decreasing the body’s perception of symptomatic pain
Thermal agents can be divided into two i.e
- Heat therapy(themotherapy)
- Cryotherapy(ice/cold therapy)
The description on the physiological effects,effectiveness,mechanism of action and current evidence is found on the following Physiopedia page :
There is moderate evidence[4] that heat therapy reduces pain and disability for patients with back pain that lasts for less than three months. The relief has only been shown to occur for a short time and the effect is relatively small. The addition of exercise to heat wrap therapy appears to provide additional benefit. There is still not enough evidence about the effect of the application of cold for low-back pain of any duration, or for heat for back pain that lasts longer than three months.
Non-Thermal Agents[edit | edit source]
Non Thermal agents do not make use of heat/cold to exert a therapeutic effect.Examples of these are shown in the table above.The following links give information about the physiological effect,mechanism of action and evidence in pain a management to the most common non thermal agents :
Low Level Laser Therapy (LLLT)
In a systematic review by Yousefi-Nooraie (2008)[5] which comprised of seven studies with a total of 384 people with non-specific LBP of varying durations. “Three of the studies (168 people) separately showed that Low level laser Therapy (LLLT) was more effective at reducing pain in the short-term (less than three months), and intermediate-term (six months) than sham (fake) laser. However, the strength and number of treatments were varied and the amount of the pain reduction was small. Three studies (102 people) separately reported that LLLT with exercise was not better than exercise alone or exercise plus sham in short-term pain reduction.”
Manual Therapy[edit | edit source]
Manual therapy can be broadly defined as
"...the useof hands in a curative and healing manner or a hands-on technique with therapeutic intent..." .It can be divided into two groups i.e Soft tissue techniques and Joint techniques
Soft Tissue Techniques[edit | edit source]
Soft tissue - This is directed at morphologically shortened muscles and/or restricted fascial mobility Techniques includes the following ( list is not exhaustive):
- Myofascial techniques
- Manual lymph drainage
- Soft tissue mobilisation (Massage)
- Functional mobilistation
- Strain constraint
- Craniosacral therapy
- Active release therapy
- Graston
- massage
- MFR,
- rolfing,
- self massage with tennis balls or even foam rolling. This is directed at morphologically shortened muscles and/or restricted fascial mobility.
Stretch[edit | edit source]
This includes neural mobilization, joint stretching, and/or muscular stretching.
Often there is an impairment in rotation(osteokinematics) and possibly an abnormal IAR. There is a need to restore tensile length and or tolerance for tensile load (distracting forces).
Joint Techniques[edit | edit source]
Joint techniques includes the following (list not exhaustive):
- Joint Mobilisation
- Muscle energy techniques
- Mulligan Techniques
- Traction
Manual Therapy Guidelines[edit | edit source]
- APA Clinical guide to safe manual therapy practice in the cervical spine 2017
- Neck Pain: Clinical Practice Guidelines
Mobilization[edit | edit source]
A detailed explaination of Mobilisation and its effect on pain can be read on this Physiopedia page: Maitlands Mobilisations There is no convincing evidence indicating whether mobiisations or manipulation are more effective than each other[7]. However regardless of this there is indication that neither of these therapies should be used in isolation, but as part of a wider treatment plan, mainly involving exercise.
Manipulation[edit | edit source]
A description of spinal manipulation is given on this Physiopedia page: Spinal Manipulation
There are variable results of research into the effectiveness of manipulation. There is a recent review by Rubinstein et al [8] that states:
"Spinal Manipulative Therapy (SMT) is no more effective in participants with acute low-back pain than inert interventions, sham SMT, or when added to another intervention. SMT also appears to be no better than other recommended therapies."
However, there is other work such as Bronfort et al[9] that suggests Manipulation is a useful tool in the treatment of Low back pain.
Soft Tissue Massage[edit | edit source]
Massage and soft tissue treatment, is often employed by physiotherapists to aid pain relief. Details of this can be found on this Physiopedia page: Massage
Patients often provide anectotal reports of its benefits, however recent research is not as supportive of its long-term benefits. Furlan et al[10] states that:
"We have very little confidence that massage is an effective treatment for LBP. Acute, sub-acute and chronic LBP had improvements in pain outcomes with massage only in the short-term follow-up. Functional improvement was observed in participants with sub-acute and chronic LBP when compared with inactive controls, but only for the short-term follow-up"
Acupuncture/Dry Needling[edit | edit source]
Acupuncture is widely used by physiotherapist for the management of pain. There is much that we still need to understand about its exact mechanisms, however patients often report anecdotal evidence of its benefits. Take a look at this physiopedia page on Acupuncture.
The introduction of the acupuncture needle (also known as a solid filiform needle) produces a numb, aching sensation called "DE QI" that is thought to be esssential for the effectiveness of the treatment. It is thought that this sensation contributes to the activation of the endogenous antinociceptive system. Bowsher(98)[11] and Wang(85)[12]theorised that De Qi is due to the activation of A delta fibres type I and III and the C-fibres releasing opioids in the dorsal horn.
Despite acupuncture being widely used and reported as being helpful, it is disappointing that there is a lack of evidence to support this.
Acupuncture- The need for research
There are other reports that indicate that the evidence base for acupuncture is widening however such as this report by Ernst.
Acupuncture-the evidence base is changing
Re-train/Re-education[edit | edit source]
Postural re-education and movement retraining are the focus here. If you bill neuromuscular re-education, this likely falls under “retraining”. Balance and gait training also fall in this category.
Educate[edit | edit source]
This patient must change modify their current activities (they themselves may be preventing a healing response). Poor habits (lack of exercise, nutrition, vices such as smoking affecting intrinsic healing potential). They may need temporary or permanent changes to their lifestyle. This may include a cardiopulmonary exercise program (walking, biking, swimming program). This is NOT neuromuscular re-education, gait training, etc.
Offload[edit | edit source]
Bracing & taping are primary examples. This may also include self-traction at home for primary decompression issues. This patient often has poor tolerance for tissue loading, and therefore this treatment is directly aimed at increasing tolerance. This may include positioning that optimizes blood flow(abduction pillow for RTC repair).
Inhibition[edit | edit source]
This includes Grade I and II joint mobilization for pain dominant joints and spinal segments. The goal is generally NOT to restore joint translation (arthrokinematics) via tissue deformation of collagenous structures. This patient generally presents with excessive spasm and guarding. This may also include post-isometric relaxation which is focusing on resetting the resting tone of the muscle spindle, it may be physiologically shortened (as opposed to morphologically shortened). The patient may also need cognitive behavioral/psycho-social strategies such as relaxation to progress mobility, function, and/or pain control.
Strengthen/Stabilize[edit | edit source]
This includes stabilization of the muscular system through exercise. The goal of this is to improve cross-sectional area and either maximum force generating capacity of that tissue and/or the endurance of that particular tissue. This tissue usually does not have a high level of intolerance and therefore the focus is on increasing the optimal loading zone and the capacity for absorbing and or creating force.
Addtionally, stabilization is commonly utilized during a spondylolisthesis patho-anatomic hypothesis (shear dysfunction) and may be confirmed with segmental testing and/or radiography. You may feel a large neutral zone (laxity) with facet gliding at the L4/5 segment and therefore need to stabilize this segment.
Integration with Other Pain Treatment Approaches.[edit | edit source]
Traditional Physiotherapy pain modalities can be integrated with other pain approaches i.e Pharmacological,Psychological,Exercise and Behavioural.There is little to no evidence on this subjcect more reasearch is warranted.
The articles below give an insight regarding pain treatment approach integration:
Integrating Pain Management in Clinical Practice
A physiotherapist-delivered integrated exercise and pain coping skills training intervention for individuals with knee osteoarthritis: a randomised controlled trial protocol[13]
For more information about other approaches follow the links below:
Pharmacology in Pain Management
Behavioural Approaches to Pain Management
Psychological approaches to pain management
Exercise and Activity in Pain Management
Additional Resources[edit | edit source]
Key Concepts in Electrotherapy[14]
References[edit | edit source]
- ↑ Key concepts in electrotherapy.http://www.electrotherapy.org/modality/key-concepts-in-electrotherapy.(Accessed 19 March 2016)
- ↑ Johnson MI, Paley CA, Howe TE, Sluka KA. Transcutaneous electrical nerve stimulation for acute pain. Cochrane Database of Systematic Reviews 2015, Issue 6. Art. No.: CD006142. DOI: 10.1002/14651858.CD006142.pub3
- ↑ https://www.youtube.com/watch?v=snXBG-gIXe8 Accessed 30/04/2016
- ↑ French SD, Cameron M, Walker BF, Reggars JW, Esterman AJ. Superficial heat or cold for low back pain. Cochrane Database of Systematic Reviews 2006, Issue 1. Art. No.: CD004750. DOI: 10.1002/14651858.CD004750.pub2
- ↑ Yousefi‐Nooraie R, Schonstein E, Heidari K, Rashidian A, Pennick V, Akbari‐Kamrani M, Irani S, Shakiba B, Mortaz Hejri S, Jonaidi AR, Mortaz‐Hedjri S. Low level laser therapy for nonspecific low‐back pain. The Cochrane Library.
- ↑ Lederman E. The Science and Practice of Manual therapy. 2nd ed. Elsevier: London. (2005)
- ↑ A. R. Gross*w, T. M. Kayz, C. Kennedyz}, D. Gasner}fckLR, L. Hurleyz8, K. Yardley**, L. Hendryww, L. McLaughlin: Clinical practice guideline on the use of manipulation or mobilization in the treatment of adults with mechanical neck disorders: Manual Therapy (2002) 7(4), 193–205
- ↑ Rubinstein SM1, Terwee CB, Assendelft WJ, de Boer MR, van Tulder MW.Spinal manipulative therapy for acute low-back pain.Cochrane Database Syst Rev. 2012 Sep 12;9:
- ↑ Bronfort G1, Haas M, Evans RL, Bouter LM.Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis.Spine J. 2004 May-Jun;4(3):335-56.
- ↑ Furlan AD1, Giraldo M, Baskwill A, Irvin E, Imamura M.Massage for low-back pain.Cochrane Database Syst Rev. 2015 Sep 1;9
- ↑ Bowsher(98) The Physiology ofstimulation produced analgesia. Journal of British medical Acupuncture society.IX(2) 58-62
- ↑ Wang AA(85) A study on the receptive fields of Acupuncture points and the relationship between characteristics of needling sensation and groups of afferent fibres. Scientific Sinica 28: 963-971
- ↑ http://bmcmusculoskeletdisord.biomedcentral.com/articles/10.1186/1471-2474-13-129
- ↑ http://www.electrotherapy.org/assets/Downloads/Key%20Concepts%20in%20Electrotherapy%20March%202014.pdf accessed 2/24/2106