Spondylodiscitis: Difference between revisions
No edit summary |
No edit summary |
||
| (44 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- [[User:Lynn Leemans|Lynn Leemans]] | '''Original Editors '''- [[User:Lynn Leemans|Lynn Leemans]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== | == Introduction == | ||
Spondylodiscitis, also referred to as discitis-osteomyelitis, is characterised by infection involving the [[intervertebral disc]] (IVD) and adjacent vertebrae.<ref name=":0">Radiopedia Spondylodiscitis Available:https://radiopaedia.org/articles/spondylodiscitis (accessed 26.11.2022) </ref> The condition is difficult to treat due to the the limited blood supply to these segments, a factor that makes it also rare. Treatment consists of an extended [[Antibiotics|antibiotic]] course, with good outcomes but misdiagnosis or a delay in treatment may result in significant morbidity/mortality.<ref name=":1">Muscara JD, Blazar E. Diskitis. InStatPearls [Internet] 2022 May 13. StatPearls Publishing. Available: https://www.ncbi.nlm.nih.gov/books/NBK541047/ (accessed 26.11.2022)</ref> | |||
'''Terminology''': Discitis is discouraged as a term as isolated infection of the spinal disc rarely occurs. Normally the initial infection is the vertebral endplate with secondary involvement of the disc. The terms spondylodiscitis or vertebral [[osteomyelitis]] are preferred as they are more accurate. | |||
== Pathology == | |||
In adults, infection starts at the vertebral body endplate, extending into the IVD space and then into the adjacent vertebral body endplate. | |||
= | Paediatrics present differently with infection often starting in the intervertebral disc itself as a good direct blood supply still present).<ref name=":0" /> | ||
== Etiology == | |||
Most cases of Spondylodiscitis arise from one of three initial events: direct inoculation, hematogenous spread, or less commonly contiguous spread. Finding the causative agent is very difficult, the most commonly identified organism is being Staphylococcus aureus.<ref name=":1" /> | |||
== Epidemiology == | |||
Spondylodiscitis has a bimodal age distribution | |||
# More common in pediatric patients than in the adult population, as consequence of the greater vascular supply of the IVD. | |||
# Older population ~50 years, more often men<ref name=":0" /><ref name=":1" /> | |||
== Risk Factors == | |||
Include | |||
* remote infection (present in ~25%) | |||
* ascending infection, e.g. from urogenital tract instrumentation | |||
* spinal instrumentation or [[Spinal Cord Injury|trauma]] | |||
* intravenous drug use (IVDU) | |||
* [[Immunocompromised Client|immunosuppression]] | |||
* long-term systemic administration of [[Corticosteroid Medication|steroids]] | |||
* advanced age | |||
* [[Diabetes|diabetes mellitus]] | |||
* organ transplantation | |||
* [[malnutrition]] | |||
* cancer<ref name=":0" /> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
The symptoms are non-specific, diffuse <ref name=" | The symptoms are non-specific, diffuse <ref name="p2">F. Postacchini, 1999, Lumbar disc herniation, Springer, 481p. (Level of evidence 5)</ref> and treacherous <ref name="p8">Erhard R, Relative Effectiveness of an Extension Program and a Combined Program of Manipulation and Flexion and Extension Exercises in Patients With Acute Low Back Syndrome, Journal of The American Physical Therapy Association 1994. (level of evidence 1A)</ref>. However the usual presentation is back pain (over 90% of patients) and possibly fever (under 20% of patients). Patients are often bacteraemic , originating from eg endocarditis, intravenous drug use.<ref name=":0" />Symptoms may include: | ||
< | *Spinal tenderness <ref name="p1" /> | ||
*Loss of lumbar lordosis and lower back movement <ref name="p1" /> | |||
*Inspection on local changes and neurological status (parese, paralyse,..) | |||
*Pain on heelstrike, impactation and percussion | |||
*Relieving posture (avoid stressing the ventral sections of the spinal column | |||
*Inclination and re-erection are painful | |||
*Reduction of mobility | |||
*[[Erector Spinae|Paravertebral muscle spasm]] <ref name="p1" /> | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 42: | Line 56: | ||
Differential diagnoses include: | Differential diagnoses include: | ||
*Erosive osteochondrosis <ref name="p8"/> | |||
*[[Insufficiency Fracture|Osteoporotic and pathological fracture]] | |||
*Cancer related destruction | |||
*[[Ankylosing Spondylitis (Axial Spondyloarthritis)|Ankylosing spondylarthritis]] | |||
*[[Scheuermann's Kyphosis|Scheuermann's kyphosis]] <ref name="p1">R. Sobottke et al., Current Diagnosis and Treatment of Spondylodiscitis. Deutsches ärzteblatt International, 2008. (Level of evidence 2A)</ref><ref name="p2" /> | |||
*[[Charcot-Marie-Tooth Disease|Charcot joint]] | |||
*[[Modic Changes|Modic]] type I degenerative change | |||
*Schmorl nodes | |||
*Langerhans cell histiocytosis (LCH) <ref name="p1"/><ref name="p2"/> | |||
*[[Disc Herniation|Disc herniation]] | |||
*Metastatic seeding | |||
*Inflammatory or [[Degenerative Disc Disease|degenerative spinal disease]] <ref name="p3">M. Titlic et al., Spondylodiscitis, Journal Citation/ Science Edition, 2008; 109(8) 345-347. (Level of evidence 2A)</ref> | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
It is important to identify and treat spondylodiscitis as early as possible. | It is important to identify and treat spondylodiscitis as early as possible. The clinical presentation of spondylodiscitis are manifold. This commonly leads to a several months from initial symptoms to final diagnosis. <ref name="p9">A. Hegde, et al., Infections of the deep neck spaces, Singapore Med J. 2012 May;53(5):305-312 (level of evidence 5)</ref> A number of different tests and tools help in diagnosis including: | ||
The clinical presentation of spondylodiscitis are manifold. This commonly leads to a several months from initial symptoms to final diagnosis. <ref name=" | |||
A | |||
* [[Medical Imaging|Medical imaging:]] [[MRI Scans|Magnetic Resonance Imaging]] (MRI) : Golden standard. Detects any spread of the inflammation. <ref name="p2" /><ref name="p8" /><ref name="p5">Enrique G. et al., Surgical treatment of spondylodiscitis. An update, International Orthopaedics 2012. (level of evidence 5)</ref><ref name="p6">Kapsalaki E. et al., Spontaneous spondylodiscitis: presentation, risk factors, diagnosis, management, and outcomes, International Journal of Infectious Diseases 2009. (level of evidence 1B)</ref><ref name="p0">P. Prithvi, et al., Intervertebral Disc: Anatomy-Physiology-Pathophysiology-Treatment, Department of Anesthesiology and Pain Management, World Institute of Pain, 2008 (level of evidence 2A)</ref><ref name="p6" />; PET and PET/CT <ref name="p3" /><ref name="p4">M. Hasenbring et al., Intervertebral disk diseases, Thieme, 2008, 236p. (Level of evidence 5)</ref><ref name="p8" />: Due to its high specificity, <ref name="p2" /> F-FDG PET/CT should be considered as a first-line imaging procedure in the diagnosis of spondylodiscitis. <ref name="p3" />And others | |||
* Biopsy: Pathogens are only successfully detected in about half of the patients. To obtain a definite diagnosis: Blood Culture <ref name="p9" /><ref name="p0" /> | |||
* [[Blood Tests|Blood tests]]<br>- | |||
== Outcome Measures == | |||
Include: | |||
*[[Visual Analogue Scale]] (VAS): <ref name="p2" /><ref name="p3" /><ref name="p4" /><ref name="p5" /> to evaluate therapeutic effects, for assessment of pain. | |||
*[[Oswestry Disability Index|Oswestry disability index]] (ODI): <ref name="p2" /><ref name="p3" /><ref name="p4" /> to evaluate therapeutic effects, assessment of quality of life<br> | |||
* | |||
== Treatment == | |||
The aim of treatment is to eliminate the infection, restore and preserve structure and function of the spine, and ease the pain. Conservative management consists of antimicrobial therapy and non-pharmacological treatments, for example physiotherapy and immobilization. Immobilization is advocated when pain is significant or there is a risk of spinal instability.<ref>Gouliouris T, Aliyu SH, Brown NM. Spondylodiscitis: update on diagnosis and management. Journal of Antimicrobial Chemotherapy. 2010 Nov 1;65(suppl_3):iii11-24. Available:https://academic.oup.com/jac/article/65/suppl_3/iii11/923760 (accessed 27.11.2022)</ref> | |||
== Physical Therapy Management == | == Physical Therapy Management == | ||
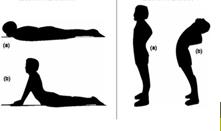
[[File:Thoracic_extension_2.jpg|alt=|thumb|Spinal extension]] | |||
Spondylodiscitis has several clinical symptoms, a severe one is low back pain. This can be treated with exercises.<ref name="p2" /> | |||
[[File:Thoracic.jpg|alt=|thumb|Thoracic extension]] | |||
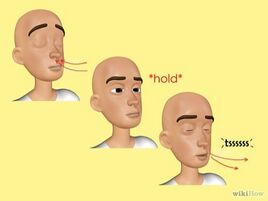
[[File:Resp.jpg|alt=|thumb|268x268px|Breathing exercises]] | |||
[[File:Hamstr.png|alt=|thumb|Flexibility exercises ]] | |||
Prognosis seems to be good with conservative treatment including [[NSAIDs|NSAID’S]], physiotherapy (exercises), and a corset. | |||
'''Immobilization''' is advocated when pain is significant or there is a risk of spinal instability. Wearing the corset for a period of 6–10 weeks is confirmed by most authors. <ref name="p8" /><ref name="p0" /><ref name="p1" /> | |||
'''Exercise''': | |||
== | * Several exercises can be done with the emphasis on extension exercises and exercises for trunk balance. This is important to maintain a good posture. <ref name="p9" /><ref name="p1" /><ref name="p2" /><ref name="p8" /><ref name="p0" /><ref name="p1" /><ref name="p0" /><ref name="p1" /> Early mobilization is important. <ref name="p8" /> | ||
* Limb exercises are considered to be good for the therapy.<ref name="p8" /> These exercises should be done daily at home. | |||
* General fitness, like swimming, should be encouraged. This therapy can lead to a decrease in pain and the ability to accomplish activities of daily living. <ref name="p0" /><ref name="p1" /> | |||
* [[Breathing Exercises|Breathing exercises.]] These exercises help the stability in the lower back. <ref name="p8" /><ref name="p7">Sans N. et al., Infections of the spinal column — Spondylodiscitis, Diagnostic and Interventional Imaging 2012. (level of evidence 5)</ref> | |||
* Low back pain is strongly related with tight and strained hamstrings. Patients should do [[flexibility]] exercises for the hamstrings, maintain a good position while sitting and move enough to help this. Keeping the hamstrings flexible is important for pain control as well as in prevention of spinal pain flare-ups. <ref name="p9" /> | |||
In general the rehabilitation program will improve the patient’s sensory and motor skills, develop the balance and proprioception and will help the patient’s to do their daily living activities. During the total program the onset and increase of pain should be evaluated. Pain intensity increases or exercises that provoke too much pain or exhaust the patient should not be in the rehabilitation program and there has to be enough rest after the exercises. It is important that when there is a resting period, this one has to be kept minimal. Immobilization lead to weakness of the trunk and lower extremity muscles and will contribute to complications. Secondary problems because of immobilization and musculoskeletal problems should be looked after and prevented. The patient also gets a home exercise program that is based on the patient’s capacity. <ref name="p1" /> | |||
== Clinical Bottom Line == | == Clinical Bottom Line == | ||
Spondylodiscitis can be defined as a primary infection of the intervertebral disc | Spondylodiscitis can be defined as a primary infection of the intervertebral disc, with secondary infections of the vertebrae (spondylitis). It can lead to osteomyelitis of the spinal column. Pyogenic spondylodiscitis is frequently caused by the staphylococcus. Tuberculous spondylodiscitis is caused by the mycobacterium tuberculosis. The symptoms are non-specific, diffuse and treacherous. Diagnosis is difficult and often delayed or missed due to the rarity of the disease. The basic diagnostic examination to establish spondylodiscitis is MRI. Surgical and conservative treatment for postoperative lumbar spondylodiscitis is effective. Prognosis seems to be good with conservative treatment including NSAID’S, physiotherapy (exercises), and a corset. | ||
== References == | == References == | ||
| Line 204: | Line 119: | ||
[[Category:Vrije_Universiteit_Brussel_Project | [[Category:Vrije_Universiteit_Brussel_Project]] [[Category:Primary Contact]] | ||
Latest revision as of 23:24, 26 November 2022
Original Editors - Lynn Leemans
Top Contributors - Ine Wittevrongel, Bo Hellinckx, Lucinda hampton, Kim Jackson, Admin, WikiSysop, 127.0.0.1 and Claire Knott
Introduction[edit | edit source]
Spondylodiscitis, also referred to as discitis-osteomyelitis, is characterised by infection involving the intervertebral disc (IVD) and adjacent vertebrae.[1] The condition is difficult to treat due to the the limited blood supply to these segments, a factor that makes it also rare. Treatment consists of an extended antibiotic course, with good outcomes but misdiagnosis or a delay in treatment may result in significant morbidity/mortality.[2]
Terminology: Discitis is discouraged as a term as isolated infection of the spinal disc rarely occurs. Normally the initial infection is the vertebral endplate with secondary involvement of the disc. The terms spondylodiscitis or vertebral osteomyelitis are preferred as they are more accurate.
Pathology[edit | edit source]
In adults, infection starts at the vertebral body endplate, extending into the IVD space and then into the adjacent vertebral body endplate.
Paediatrics present differently with infection often starting in the intervertebral disc itself as a good direct blood supply still present).[1]
Etiology[edit | edit source]
Most cases of Spondylodiscitis arise from one of three initial events: direct inoculation, hematogenous spread, or less commonly contiguous spread. Finding the causative agent is very difficult, the most commonly identified organism is being Staphylococcus aureus.[2]
Epidemiology[edit | edit source]
Spondylodiscitis has a bimodal age distribution
- More common in pediatric patients than in the adult population, as consequence of the greater vascular supply of the IVD.
- Older population ~50 years, more often men[1][2]
Risk Factors[edit | edit source]
Include
- remote infection (present in ~25%)
- ascending infection, e.g. from urogenital tract instrumentation
- spinal instrumentation or trauma
- intravenous drug use (IVDU)
- immunosuppression
- long-term systemic administration of steroids
- advanced age
- diabetes mellitus
- organ transplantation
- malnutrition
- cancer[1]
Characteristics/Clinical Presentation[edit | edit source]
The symptoms are non-specific, diffuse [3] and treacherous [4]. However the usual presentation is back pain (over 90% of patients) and possibly fever (under 20% of patients). Patients are often bacteraemic , originating from eg endocarditis, intravenous drug use.[1]Symptoms may include:
- Spinal tenderness [5]
- Loss of lumbar lordosis and lower back movement [5]
- Inspection on local changes and neurological status (parese, paralyse,..)
- Pain on heelstrike, impactation and percussion
- Relieving posture (avoid stressing the ventral sections of the spinal column
- Inclination and re-erection are painful
- Reduction of mobility
- Paravertebral muscle spasm [5]
Differential Diagnosis[edit | edit source]
Differential diagnoses include:
- Erosive osteochondrosis [4]
- Osteoporotic and pathological fracture
- Cancer related destruction
- Ankylosing spondylarthritis
- Scheuermann's kyphosis [5][3]
- Charcot joint
- Modic type I degenerative change
- Schmorl nodes
- Langerhans cell histiocytosis (LCH) [5][3]
- Disc herniation
- Metastatic seeding
- Inflammatory or degenerative spinal disease [6]
Diagnostic Procedures[edit | edit source]
It is important to identify and treat spondylodiscitis as early as possible. The clinical presentation of spondylodiscitis are manifold. This commonly leads to a several months from initial symptoms to final diagnosis. [7] A number of different tests and tools help in diagnosis including:
- Medical imaging: Magnetic Resonance Imaging (MRI) : Golden standard. Detects any spread of the inflammation. [3][4][8][9][10][9]; PET and PET/CT [6][11][4]: Due to its high specificity, [3] F-FDG PET/CT should be considered as a first-line imaging procedure in the diagnosis of spondylodiscitis. [6]And others
- Biopsy: Pathogens are only successfully detected in about half of the patients. To obtain a definite diagnosis: Blood Culture [7][10]
- Blood tests
-
Outcome Measures[edit | edit source]
Include:
- Visual Analogue Scale (VAS): [3][6][11][8] to evaluate therapeutic effects, for assessment of pain.
- Oswestry disability index (ODI): [3][6][11] to evaluate therapeutic effects, assessment of quality of life
Treatment[edit | edit source]
The aim of treatment is to eliminate the infection, restore and preserve structure and function of the spine, and ease the pain. Conservative management consists of antimicrobial therapy and non-pharmacological treatments, for example physiotherapy and immobilization. Immobilization is advocated when pain is significant or there is a risk of spinal instability.[12]
Physical Therapy Management[edit | edit source]
Spondylodiscitis has several clinical symptoms, a severe one is low back pain. This can be treated with exercises.[3]
Prognosis seems to be good with conservative treatment including NSAID’S, physiotherapy (exercises), and a corset.
Immobilization is advocated when pain is significant or there is a risk of spinal instability. Wearing the corset for a period of 6–10 weeks is confirmed by most authors. [4][10][5]
Exercise:
- Several exercises can be done with the emphasis on extension exercises and exercises for trunk balance. This is important to maintain a good posture. [7][5][3][4][10][5][10][5] Early mobilization is important. [4]
- Limb exercises are considered to be good for the therapy.[4] These exercises should be done daily at home.
- General fitness, like swimming, should be encouraged. This therapy can lead to a decrease in pain and the ability to accomplish activities of daily living. [10][5]
- Breathing exercises. These exercises help the stability in the lower back. [4][13]
- Low back pain is strongly related with tight and strained hamstrings. Patients should do flexibility exercises for the hamstrings, maintain a good position while sitting and move enough to help this. Keeping the hamstrings flexible is important for pain control as well as in prevention of spinal pain flare-ups. [7]
In general the rehabilitation program will improve the patient’s sensory and motor skills, develop the balance and proprioception and will help the patient’s to do their daily living activities. During the total program the onset and increase of pain should be evaluated. Pain intensity increases or exercises that provoke too much pain or exhaust the patient should not be in the rehabilitation program and there has to be enough rest after the exercises. It is important that when there is a resting period, this one has to be kept minimal. Immobilization lead to weakness of the trunk and lower extremity muscles and will contribute to complications. Secondary problems because of immobilization and musculoskeletal problems should be looked after and prevented. The patient also gets a home exercise program that is based on the patient’s capacity. [5]
Clinical Bottom Line[edit | edit source]
Spondylodiscitis can be defined as a primary infection of the intervertebral disc, with secondary infections of the vertebrae (spondylitis). It can lead to osteomyelitis of the spinal column. Pyogenic spondylodiscitis is frequently caused by the staphylococcus. Tuberculous spondylodiscitis is caused by the mycobacterium tuberculosis. The symptoms are non-specific, diffuse and treacherous. Diagnosis is difficult and often delayed or missed due to the rarity of the disease. The basic diagnostic examination to establish spondylodiscitis is MRI. Surgical and conservative treatment for postoperative lumbar spondylodiscitis is effective. Prognosis seems to be good with conservative treatment including NSAID’S, physiotherapy (exercises), and a corset.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Radiopedia Spondylodiscitis Available:https://radiopaedia.org/articles/spondylodiscitis (accessed 26.11.2022)
- ↑ 2.0 2.1 2.2 Muscara JD, Blazar E. Diskitis. InStatPearls [Internet] 2022 May 13. StatPearls Publishing. Available: https://www.ncbi.nlm.nih.gov/books/NBK541047/ (accessed 26.11.2022)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 F. Postacchini, 1999, Lumbar disc herniation, Springer, 481p. (Level of evidence 5)
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Erhard R, Relative Effectiveness of an Extension Program and a Combined Program of Manipulation and Flexion and Extension Exercises in Patients With Acute Low Back Syndrome, Journal of The American Physical Therapy Association 1994. (level of evidence 1A)
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 R. Sobottke et al., Current Diagnosis and Treatment of Spondylodiscitis. Deutsches ärzteblatt International, 2008. (Level of evidence 2A)
- ↑ 6.0 6.1 6.2 6.3 6.4 M. Titlic et al., Spondylodiscitis, Journal Citation/ Science Edition, 2008; 109(8) 345-347. (Level of evidence 2A)
- ↑ 7.0 7.1 7.2 7.3 A. Hegde, et al., Infections of the deep neck spaces, Singapore Med J. 2012 May;53(5):305-312 (level of evidence 5)
- ↑ 8.0 8.1 Enrique G. et al., Surgical treatment of spondylodiscitis. An update, International Orthopaedics 2012. (level of evidence 5)
- ↑ 9.0 9.1 Kapsalaki E. et al., Spontaneous spondylodiscitis: presentation, risk factors, diagnosis, management, and outcomes, International Journal of Infectious Diseases 2009. (level of evidence 1B)
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 P. Prithvi, et al., Intervertebral Disc: Anatomy-Physiology-Pathophysiology-Treatment, Department of Anesthesiology and Pain Management, World Institute of Pain, 2008 (level of evidence 2A)
- ↑ 11.0 11.1 11.2 M. Hasenbring et al., Intervertebral disk diseases, Thieme, 2008, 236p. (Level of evidence 5)
- ↑ Gouliouris T, Aliyu SH, Brown NM. Spondylodiscitis: update on diagnosis and management. Journal of Antimicrobial Chemotherapy. 2010 Nov 1;65(suppl_3):iii11-24. Available:https://academic.oup.com/jac/article/65/suppl_3/iii11/923760 (accessed 27.11.2022)
- ↑ Sans N. et al., Infections of the spinal column — Spondylodiscitis, Diagnostic and Interventional Imaging 2012. (level of evidence 5)