Splinting: Difference between revisions
No edit summary |
Amanda Ager (talk | contribs) No edit summary |
||
| (41 intermediate revisions by 6 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> '''Original Editor '''- [[User:Shwe Shwe U Marma|Shwe Shwe U Marma]] | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}}</div> | |||
== Introduction == | |||
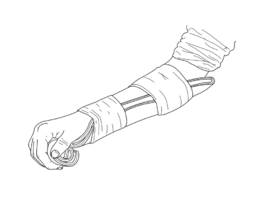
<div class="editorbox"> | [[Image:Arm splint.png|alt=|thumb|Arm Splint|265x265px]]A [[splint]] is a rigid support made from metal, plaster, or plastic. It's used to protect <ref>VanBlarcom CW, editor. [https://www.thejpd.org/article/S0022-3913(99)70234-9/fulltext The glossary of prosthodontic terms]. Mosby; 1999.</ref>, support, or immobilize an injured or inflamed part of the body.<ref name=":1">Althoff AD, Reeves RA. [https://www.ncbi.nlm.nih.gov/books/NBK557673/ Splinting]. StatPearls [Internet]. 2020 May 24.</ref> | ||
'''Original Editor '''- [[User:Shwe Shwe U Marma|Shwe Shwe U Marma]] | |||
''' | == '''Purpose''' == | ||
Splints have various purposes. Including: | |||
* Immobilization | |||
* Support to Promote Healing | |||
* Pain | * Positioning or supporting during function | ||
*[[Pain-Modulation|Pain Relief]] <ref name=":0">Boyd AS, Benjamin HJ, Asplund CA. [https://www.researchgate.net/publication/26784832_Splints_and_Casts_Indications_and_Methods Splints and casts: indications and methods]. American family physician. 2009 Sep 1;80(5):491-9.</ref> | |||
* Substitute for Weak Muscles | |||
* Prevention | * Prevention and Correction of Contracture & Deformity <ref>Singh KA, Shah H, Joseph B. [https://online.boneandjoint.org.uk/doi/abs/10.1302/0301-620X.102B10.BJJ-2020-0181.R4 Comparison of plaster-of-Paris casts and Woodcast splints for immobilization of the limb during serial manipulation and casting for idiopathic clubfoot in infants: a prospective randomized trial]. The Bone & Joint Journal. 2020 Oct 3;102(10):1399-404.</ref> | ||
* Restoration or Maintenance of [[Range of Motion]] <ref>Rezaei B, Mahdavinejad R. [https://japer.in/storage/models/article/PuhlW9qhFMTWZ0y8u4MRHzXx4GSaVQRsF5R7Y7JeXDZtYo4GMUcPDkPvWRyt/massage-therapy-and-splint-in-males-with-carpal-tunnel-syndrome.pdf Massage therapy and Splint in males with Carpal Tunnel syndrome]. Journal of Advanced Pharmacy Education & Research| Jan-Mar. 2020;10(S1).</ref> | |||
* Maintenance | *[[Oedema Assessment|Edema Control]] <ref>Giang TA, Ong AW, Krishnamurthy K, Fong KN. [https://journals.sagepub.com/doi/full/10.1016/j.hkjot.2016.03.002 Rehabilitation interventions for poststroke hand oedema: a systematic review]. Hong Kong Journal of Occupational Therapy. 2016 Jun 1;27:7-17.</ref> | ||
* | |||
== Different Types of Splints == | == Different Types of Splints == | ||
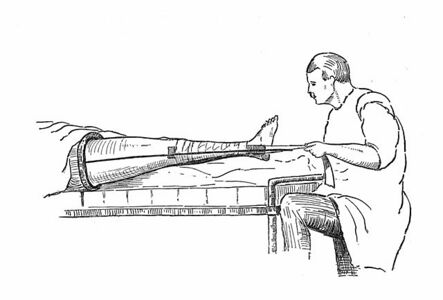
[[Image:Thomas's splint.jpg|alt=|thumb|Thomas's Splint|443x443px]]Splints are classified based on the movement permissible as | |||
{| | |||
* Static | |||
* Dynamic | |||
* Serial Static | |||
* Static Progressive | |||
== Regional Splints == | |||
==== 1. Splints for Upper Extremity ==== | |||
{| cellspacing="1" cellpadding="1" border="1" width="800" | |||
|+'''Table.1''' Splints for Lower Extremity <ref name=":0" /> | |||
|- | |- | ||
| | ! scope="col" |'''Region''' | ||
!'''Type of Splint''' | |||
|- | |- | ||
| | |Ulnar Side of Hand | ||
| | |Ulnar Gutter Splint | ||
|- | |- | ||
| | |Radial Side of Hand | ||
| | |Radial Gutter Splint | ||
|- | |- | ||
|Finger | |Thumb, First Metacarpal, and Carpal Bones | ||
|Thumb Spica Splint | |||
|- | |||
|Finger Injuries | |||
| | | | ||
* Buddy | * Buddy Taping | ||
* Aluminium U-shaped | * Aluminium U-shaped Splint | ||
* Dorsal | * Dorsal Extension-block Splint | ||
* Mallet finger splint | * Mallet Finger Splint | ||
[[File:Mallet finger splint (thermoplastic).jpg|alt=Image showing mallet finger splint applied|left|thumb|171x171px|Mallet finger splint]] | |||
|- | |- | ||
|Wrist/ | |Wrist / Hand | ||
| | | | ||
* Volar/dorsal forearm splint | * Volar/dorsal forearm splint | ||
| Line 47: | Line 56: | ||
|- | |- | ||
|Forearm | |Forearm | ||
|Single | | | ||
* Single Sugar-tong Splint | |||
|- | |- | ||
|Elbow, proximal forearm, and skeletally immature wrist injuries | |Elbow, proximal forearm, and skeletally immature wrist injuries | ||
| | | | ||
* Long | * Long Arm Posterior Splint | ||
* Long | * Long Arm Cast | ||
* Double | * Double Sugar-tong Splint | ||
|} | |} | ||
==== 2. Splints for Lower Extremity ==== | |||
{| cellspacing="1" cellpadding="1" border="1" width="800" | |||
|+'''Table.2''' Splints for Lower Extremity <ref name=":0" /> | |||
|- | |||
! scope="col" |'''Region''' | |||
!'''Type of Splint''' | |||
|- | |||
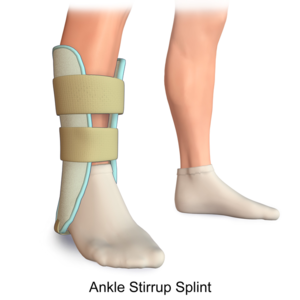
|Ankle | |||
| | |||
* Posterior Ankle Splint | |||
* Stirrup Splint | |||
[[File:Ankle splint.png|left|thumb|300x300px|Ankle Stirrup Splint|alt=]] | |||
|- | |||
|Lower Leg, Ankle and Foot | |||
|Short Leg Cast | |||
|- | |||
|Knee and Lower Leg | |||
|Posterior Knee Splint | |||
|- | |||
|Foot | |||
|Short Leg Cast with Toe Plate Extension | |||
|} | |||
== Indications of Splinting == | |||
[[File:Sprained Ankle.JPG|alt=Image showing swollen sprained left ankle|thumb|Swollen sprained ankle, an indication for splinting]] | |||
Splints are used to immobilize musculoskeletal and nerve injuries, support healing, and to prevent further damage. The indications for splinting are broad, but commonly include: | |||
* Temporary stabilization of acute fractures, sprains, strains or nerve injuries before further evaluation or definitive operative management | |||
* Immobilization of a suspected occult fracture (such as a scaphoid fracture) | |||
* Severe soft tissue injuries requiring immobilization and protection from further injury | |||
* Definitive management of specific stable fracture patterns | |||
* Peripheral neuropathy requiring extremity protection | |||
* Partial immobilization for minor soft tissue injuries | |||
* Treatment of joint instability, including dislocation <ref name=":1" /> | |||
== Contraindications of Splinting == | |||
No specific contraindications to splinting exist. However, certain injuries and patient-specific co-morbidities require special attention: | |||
* '''Injuries that Violate the Skin or Open Wounds:''' | |||
** Antibiotic administration should be considered for these patients depending on the severity of the lesion. These patients also require additional soft tissue care, which may necessitate tissue debridement and skin closure before splint application. | |||
* '''Injuries that Result in Sensory or Neurological Deficits:''' | |||
** The complications of splint placement such as [[Compartment Syndrome|compartment syndrome]], pressure injuries, or malreduction may go unnoticed if the patient has a concurrent nerve injury. These patients should undergo evaluation by a surgeon before splint application as neurologic findings may be a sign of a surgical emergency. | |||
* '''Injuries to the Vasculature:''' | |||
** This requires special attention by vascular surgeons, as these may require urgent operative intervention. Furthermore, evaluation of the vasculature is essential both before and after splint application, as the reduction of some fractures may result in acute arterial injury or obstruction if trapped between the fracture fragments. | |||
* '''Patients with Peripheral Vascular Disease or Peripheral [[Neuropathies|Neuropathy]]:''' | |||
** Special care should be taken when applying lower extremity splints in these patients since their baseline sensation may be altered. These patients have difficulty detecting pressure sores, skin irritation, and possible vascular compromise.<ref name=":1" /> | |||
== Side Effects of Splinting == | |||
* Excessive use of splints can lead to chronic pain, stiff joints or weak muscles <ref>Gravlee JR, Van Durme DJ. [https://www.aafp.org/afp/2007/0201/p342.html Braces and splints for musculoskeletal conditions]. American family physician. 2007 Feb 1;75(3):342-8.</ref> | |||
* Skin irritation <ref>Johnston JJ, Spelman L. [https://pubmed.ncbi.nlm.nih.gov/27613591/ Pressure-induced localised granuloma annulare following use of an elbow splint]. Prosthetics and orthotics international. 2017 Jun;41(3):311-3.</ref> | |||
* Discomfort <ref>So H, Chung VC, Cheng JC, Yip RM. [https://onlinelibrary.wiley.com/doi/full/10.1111/1756-185X.13162 Local steroid injection versus wrist splinting for carpal tunnel syndrome: a randomized clinical trial]. International Journal of Rheumatic Diseases. 2018 Jan;21(1):102-7.</ref> | |||
== Advantages of Splinting == | |||
Splint use offers many advantages over casting. | |||
* Splints are faster and easier to apply. | |||
* They may be static (i.e., prevent motion) or dynamic (i.e., functional; assist with controlled motion). | |||
* Splints are non-circumferential, allowing for natural swelling that occurs during the initial inflammatory phase of the injury. | |||
* A splint may be removed more easily than a cast, allowing for regular inspection of the injury site.<ref name=":2" /> | |||
== Disadvantages of Splinting == | |||
Disadvantages of Splinting include; | |||
* Poor Patient Compliance | |||
* Excessive Motion at the Injury Site | |||
* Limitations in their usage, as in unstable or potentially unstable fractures<ref name=":2" /> | |||
== Complications of Splinting == | |||
[[File:Acute Compartment Syndrome.JPG|alt=Image showing compartment syndrome in arm with blister formation|thumb|Compartment Syndrome]] | |||
* Compartment Syndrome | |||
* Ischemia | |||
* Heat Injury | |||
* Pressure Sores and Skin Breakdown | |||
* Edema | |||
* Infection | |||
* Dermatitis | |||
* Joint Stiffness | |||
* Altered Range of Motion | |||
* Decreased Strength | |||
* Altered Sensation | |||
* Neurological injury<ref name=":2">Boyd AS, Benjamin HJ, Asplund CA. [https://www.aafp.org/afp/2009/0101/p16.html Principles of casting and splinting]. American family physician. 2009 Jan 1;79(1):16-22.</ref> | |||
=== Considerations for Effective Splinting === | |||
* Creases provide for landmarks in splint fabrication | |||
* Bony prominences may cause pressure | |||
* Ensure three points of pressure | |||
* Custom made splints to fit the contours of the body rather than ready-made splints | |||
* Patient education for better compliance | |||
== References == | == References == | ||
| Line 60: | Line 154: | ||
<references /> | <references /> | ||
[[Category:Interventions]] | [[Category:Interventions]] | ||
[[Category:Injury]] | |||
[[Category:Course Pages]] | |||
Latest revision as of 18:38, 10 November 2022
Introduction[edit | edit source]
A splint is a rigid support made from metal, plaster, or plastic. It's used to protect [1], support, or immobilize an injured or inflamed part of the body.[2]
Purpose[edit | edit source]
Splints have various purposes. Including:
- Immobilization
- Support to Promote Healing
- Positioning or supporting during function
- Pain Relief [3]
- Substitute for Weak Muscles
- Prevention and Correction of Contracture & Deformity [4]
- Restoration or Maintenance of Range of Motion [5]
- Edema Control [6]
Different Types of Splints[edit | edit source]
Splints are classified based on the movement permissible as
- Static
- Dynamic
- Serial Static
- Static Progressive
Regional Splints[edit | edit source]
1. Splints for Upper Extremity[edit | edit source]
| Region | Type of Splint |
|---|---|
| Ulnar Side of Hand | Ulnar Gutter Splint |
| Radial Side of Hand | Radial Gutter Splint |
| Thumb, First Metacarpal, and Carpal Bones | Thumb Spica Splint |
| Finger Injuries |
|
| Wrist / Hand |
|
| Forearm |
|
| Elbow, proximal forearm, and skeletally immature wrist injuries |
|
2. Splints for Lower Extremity[edit | edit source]
| Region | Type of Splint |
|---|---|
| Ankle |
|
| Lower Leg, Ankle and Foot | Short Leg Cast |
| Knee and Lower Leg | Posterior Knee Splint |
| Foot | Short Leg Cast with Toe Plate Extension |
Indications of Splinting[edit | edit source]
Splints are used to immobilize musculoskeletal and nerve injuries, support healing, and to prevent further damage. The indications for splinting are broad, but commonly include:
- Temporary stabilization of acute fractures, sprains, strains or nerve injuries before further evaluation or definitive operative management
- Immobilization of a suspected occult fracture (such as a scaphoid fracture)
- Severe soft tissue injuries requiring immobilization and protection from further injury
- Definitive management of specific stable fracture patterns
- Peripheral neuropathy requiring extremity protection
- Partial immobilization for minor soft tissue injuries
- Treatment of joint instability, including dislocation [2]
Contraindications of Splinting[edit | edit source]
No specific contraindications to splinting exist. However, certain injuries and patient-specific co-morbidities require special attention:
- Injuries that Violate the Skin or Open Wounds:
- Antibiotic administration should be considered for these patients depending on the severity of the lesion. These patients also require additional soft tissue care, which may necessitate tissue debridement and skin closure before splint application.
- Injuries that Result in Sensory or Neurological Deficits:
- The complications of splint placement such as compartment syndrome, pressure injuries, or malreduction may go unnoticed if the patient has a concurrent nerve injury. These patients should undergo evaluation by a surgeon before splint application as neurologic findings may be a sign of a surgical emergency.
- Injuries to the Vasculature:
- This requires special attention by vascular surgeons, as these may require urgent operative intervention. Furthermore, evaluation of the vasculature is essential both before and after splint application, as the reduction of some fractures may result in acute arterial injury or obstruction if trapped between the fracture fragments.
- Patients with Peripheral Vascular Disease or Peripheral Neuropathy:
- Special care should be taken when applying lower extremity splints in these patients since their baseline sensation may be altered. These patients have difficulty detecting pressure sores, skin irritation, and possible vascular compromise.[2]
Side Effects of Splinting[edit | edit source]
- Excessive use of splints can lead to chronic pain, stiff joints or weak muscles [7]
- Skin irritation [8]
- Discomfort [9]
Advantages of Splinting[edit | edit source]
Splint use offers many advantages over casting.
- Splints are faster and easier to apply.
- They may be static (i.e., prevent motion) or dynamic (i.e., functional; assist with controlled motion).
- Splints are non-circumferential, allowing for natural swelling that occurs during the initial inflammatory phase of the injury.
- A splint may be removed more easily than a cast, allowing for regular inspection of the injury site.[10]
Disadvantages of Splinting[edit | edit source]
Disadvantages of Splinting include;
- Poor Patient Compliance
- Excessive Motion at the Injury Site
- Limitations in their usage, as in unstable or potentially unstable fractures[10]
Complications of Splinting[edit | edit source]
- Compartment Syndrome
- Ischemia
- Heat Injury
- Pressure Sores and Skin Breakdown
- Edema
- Infection
- Dermatitis
- Joint Stiffness
- Altered Range of Motion
- Decreased Strength
- Altered Sensation
- Neurological injury[10]
Considerations for Effective Splinting[edit | edit source]
- Creases provide for landmarks in splint fabrication
- Bony prominences may cause pressure
- Ensure three points of pressure
- Custom made splints to fit the contours of the body rather than ready-made splints
- Patient education for better compliance
References[edit | edit source]
- ↑ VanBlarcom CW, editor. The glossary of prosthodontic terms. Mosby; 1999.
- ↑ 2.0 2.1 2.2 Althoff AD, Reeves RA. Splinting. StatPearls [Internet]. 2020 May 24.
- ↑ 3.0 3.1 3.2 Boyd AS, Benjamin HJ, Asplund CA. Splints and casts: indications and methods. American family physician. 2009 Sep 1;80(5):491-9.
- ↑ Singh KA, Shah H, Joseph B. Comparison of plaster-of-Paris casts and Woodcast splints for immobilization of the limb during serial manipulation and casting for idiopathic clubfoot in infants: a prospective randomized trial. The Bone & Joint Journal. 2020 Oct 3;102(10):1399-404.
- ↑ Rezaei B, Mahdavinejad R. Massage therapy and Splint in males with Carpal Tunnel syndrome. Journal of Advanced Pharmacy Education & Research| Jan-Mar. 2020;10(S1).
- ↑ Giang TA, Ong AW, Krishnamurthy K, Fong KN. Rehabilitation interventions for poststroke hand oedema: a systematic review. Hong Kong Journal of Occupational Therapy. 2016 Jun 1;27:7-17.
- ↑ Gravlee JR, Van Durme DJ. Braces and splints for musculoskeletal conditions. American family physician. 2007 Feb 1;75(3):342-8.
- ↑ Johnston JJ, Spelman L. Pressure-induced localised granuloma annulare following use of an elbow splint. Prosthetics and orthotics international. 2017 Jun;41(3):311-3.
- ↑ So H, Chung VC, Cheng JC, Yip RM. Local steroid injection versus wrist splinting for carpal tunnel syndrome: a randomized clinical trial. International Journal of Rheumatic Diseases. 2018 Jan;21(1):102-7.
- ↑ 10.0 10.1 10.2 Boyd AS, Benjamin HJ, Asplund CA. Principles of casting and splinting. American family physician. 2009 Jan 1;79(1):16-22.