Respiratory Failure: Difference between revisions
No edit summary |
No edit summary |
||
| Line 9: | Line 9: | ||
Respiratory failure is a clinical condition that happens when the respiratory system fails to maintain its main function, which is gas exchange, in which PaO2 is lower than 60 mmHg and/or PaCO2 higher than 50 mmHg. | Respiratory failure is a clinical condition that happens when the respiratory system fails to maintain its main function, which is gas exchange, in which PaO2 is lower than 60 mmHg and/or PaCO2 higher than 50 mmHg. | ||
Respiratory failure is classified according to blood gases abnormalities into type 1 and type 2. Type | Respiratory failure is classified according to blood gases abnormalities into type 1 and type 2. | ||
Type 1 - ([[Hypoxaemia|hypoxemic]]) respiratory failure has a PaO2 < 60 mmHg with normal or subnormal PaCO2. In this type, the gas exchange is impaired at the level of aveolo-capillary membrane. Examples of type I respiratory failures are [[Oncology|carcinogenic]] or non-cardiogenic [[Pulmonary Oedema|pulmonary edema]] and severe [[pneumonia]]. | |||
Type 2 - ([[Hypercapnia|hypercapnic]]) respiratory failure has a PaCO2 > 50 mmHg. Hypoxemia is common, and it is due to respiratory pump failure. | |||
* Respiratory failure is classified also according to its onset, course, and duration into acute, chronic, and acute on top of chronic respiratory failure<ref name=":2">Shebl E, Burns B. Respiratory failure..Available from:https://www.ncbi.nlm.nih.gov/books/NBK526127/?report=printable (last accessed 28.9.2020)</ref>. | * Respiratory failure is classified also according to its onset, course, and duration into acute, chronic, and acute on top of chronic respiratory failure<ref name=":2">Shebl E, Burns B. Respiratory failure..Available from:https://www.ncbi.nlm.nih.gov/books/NBK526127/?report=printable (last accessed 28.9.2020)</ref>. | ||
* It's a major cause of mortality and morbidity and mortality rates increase with age and presence of co-morbidities. | * It's a major cause of mortality and morbidity and mortality rates increase with age and presence of co-morbidities. | ||
Revision as of 06:52, 29 September 2020
Original Editor - Simisola Ajeyalemi
Top Contributors - Lucinda hampton, Simisola Ajeyalemi, Kim Jackson, Rachael Lowe, Uchechukwu Chukwuemeka, Admin, Laura Ritchie, Evan Thomas, Karen Wilson, Vidya Acharya, Abbey Wright and Rania Nasr
Introduction[edit | edit source]
Respiratory failure is a clinical condition that happens when the respiratory system fails to maintain its main function, which is gas exchange, in which PaO2 is lower than 60 mmHg and/or PaCO2 higher than 50 mmHg.
Respiratory failure is classified according to blood gases abnormalities into type 1 and type 2.
Type 1 - (hypoxemic) respiratory failure has a PaO2 < 60 mmHg with normal or subnormal PaCO2. In this type, the gas exchange is impaired at the level of aveolo-capillary membrane. Examples of type I respiratory failures are carcinogenic or non-cardiogenic pulmonary edema and severe pneumonia.
Type 2 - (hypercapnic) respiratory failure has a PaCO2 > 50 mmHg. Hypoxemia is common, and it is due to respiratory pump failure.
- Respiratory failure is classified also according to its onset, course, and duration into acute, chronic, and acute on top of chronic respiratory failure[1].
- It's a major cause of mortality and morbidity and mortality rates increase with age and presence of co-morbidities.
Respiratory Physiology[edit | edit source]
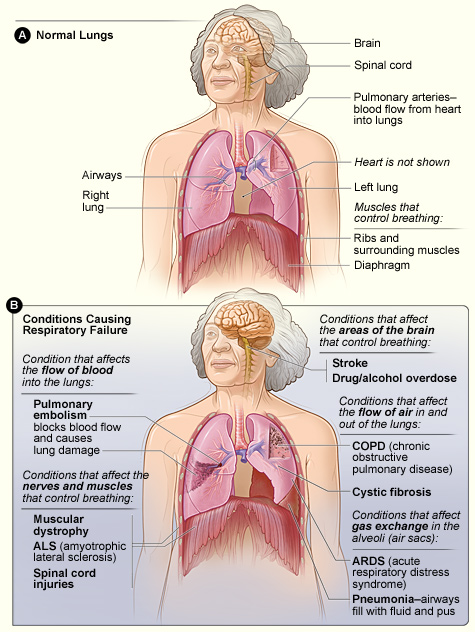
The respiratory system can be said to consist of two parts:
- Lung- gas exchanging organ
- Respiratory pump- ventilates the lungs. The respiratory pumps consists of the chest wall- respiratory muscles, the respiratory controllers in the CNS and the pathways that connect the central controllers with the respiratory muscles i.e the spinal and peripheral nerves.
The act of respiration engages three processes:
- Transfer of oxygen across the alveolus,
- Transfer of oxygen to the tissues
- Removal of carbon dioxide from the blood into the alveolus and then the environment.
The alveolar capillary unit of the lungs are primarily where respiration takes place with exchange of oxygen and carbon dioxide between alveolar gas and blood. Oxygen reversibly binds with hemoglobin after diffusing into the blood.
Pathophysiology[edit | edit source]
The main path physiologic mechanisms of respiratory failure are:
- Hypoventilation: in which PaCO2 and PaO2 and alveolar-arterial PO2 gradient are normal. Depression of CNS from drugs is an example of this condition.
- V/P mismatch: this is the most common cause of hypoxemia. Administration of 100% O2 eliminates hypoxemia.
- Shunt: in which there is persistent hypoxemia despite 100% O2 inhalation. In cases of a shunt, the deoxygenated blood (mixed venous blood) bypasses the alveoli without being oxygenated and mixes with oxygenated blood that has flowed through the ventilated alveoli, and this leads to hypoxemia as in cases of pulmonary edema (cardiogenic or noncardiogenic), pneumonia and atelectasis[1]
Generally, failure of the lung caused by a variety of lung disease leads failure of gas exchange manifested by hypoxemia whilst failure of the pump results in ventilatory failure manifested as hypercapnia. Lung diseases may result in muscle fatigue and ventilatory failure through an imbalance between demands and supplies. Likewise, patients with diseases that involve the ventilatory pump and present with hypercapnia are typically characterized by inability to cough and possibly atelectasis. This aggravates V/Q mismatch resulting in hypoxaemia.
Type I Respiratory Failure
Four pathophysiological mechanisms accounts for hypoxaemia in a variety of diseases and this includes: ventilation/perfusion(V/Q) mismatch, increased shunt, diffusion impairment and alveolar hypoventilation.[2]
- V/Q mismatch(low V/Q), which is the most common mechanism develops when there are lung regions with a greater reduction in ventilation than in perfusion.
- In shunt, there is a bypass of ventilated alveoli by intrapulmonary or intracardiac deoxygenated mixed venous blood resulting in venous admixture.
- Diffusion pathway for oxygen from the alveolar space to the pulmonary capillaries can be increased by diseases which in turn decreases capillary surface area prevents complete equilibrium of alveolar oxygen with pulmonary capillary blood.
- In underlying pulmonary disease, there is broadening of the alveolar/arterial gradient- either due to V/Q mismatch or shunt or diffusion impairment results in severe hypoxemia while for hypoxaemia accompanying hypoventilation(without underlying pulmonary disease) the alveolar/arterial gradient is normal
Type II Respiratory Failure
Pump failure leading to hypercapnia is caused by three major factors which includes: inadequate output of the respiratory centers controlling the muscles, mechanical defect in the chest wall, excessive inspiratory load
- Inadequate output of the respiratory centers controlling the muscles results in an insufficient respiratory drive for the demand or the respiratory centers my reflexively modify their output to prevent respiratory muscle injury and avoid fatigue. Insufficient activation from the CNS either temporarily- from anesthesia, drug overdose or permanently- diseases of the medulla results in inadequate respiratory efforts and hypoventilation ensues.
- Mechanical defects in the chest wall as in flail chest, diseases of the nerves (Guillain-Barre syndrome) and anterior horn cells(poliomyelitis) or diseases of the respiratory muscles(myopathies)
- Excessive inspiratory load fatigues the inspiratory muscles- they are unable to generate an adequate pleural pressure even though there is an adequate respiratory drive and an intact chest wall. Factors that increase inspiratory muscle energy demand and/or decrease energy supplies predisposes respiratory muscles to fatigue.
Epidemiology[edit | edit source]
Overall frequency of respiratory failure is not well known as respiratory failure is a syndrome not a single disease process[1].
Etiology[edit | edit source]
Respiratory failure may be due to pulmonary or extra-pulmonary causes which include:
- CNS causes due to depression of the neural drive to breath as in cases of overdose of a narcotic and sedative.
- Disorders of the peripheral nervous system: Respiratory muscle and chest wall weakness as in cases of Guillian-Barre syndrome and myasthenia gravis.
- Upper and lower airways obstruction: due to various causes as in cases of exacerbation of chronic obstructive pulmonary diseases and acute severe bronchial asthma
- Abnormities of the alveoli that result in type 1 (hypoxemic) respiratory failure as in cases of pulmonary edema and severe pneumonia[1]
Clinical Presentation[edit | edit source]
Presentation of respiratory failure is dependent on the underlying cause and associated hypoxemia or hypercapnia. Common presentations include:
- Dyspnoea
- Tachypnoea
- Restlessness
- Confusion
- Anxiety
- Cyanosis- central
- Tachycardia
- Pulmonary hypertension
- Loss of consciousness
Signs and symptoms of RF Type I (Hypoxemia) include[3]:
- Dyspnea, irritability
- Confusion, fits, somnolence
- Tachycardia, arrhythmia
- Tachypnea
- Cyanosis
Signs and symptoms of RF Type II (Hypercapnia) include[3]:
- Change of behavior
- headache
- Coma
- Warm extremities
- Astrexis
- Papilloedema
Symptoms and signs of the underlying disease[3]:eg
- Fever, cough, sputum production, chest pain in cases of pneumonia.
- History of sepsis, polytrauma, burn, or blood transfusions before the onset of acute respiratory failure may point to acute respiratory distress syndrome
Physical Findings[edit | edit source]
These are signs that suggest a possible underlying cause of respiratory failure include:
- Hypotension usually with signs of poor perfusion suggest severe sepsis or pulmonary embolus
- Hypertension usually with signs of poor perfusion suggests cardiogenic pulmonary edema
- Wheeze & stridor suggest airway obstruction
- Tachycardia and arrhythmias may be the cause of cardiogenic pulmonary edema
- Elevated jugular venous pressure suggests right ventricular dysfunction
- Respiratory rate < 12b/m in spontaneously breathing patient with hypoxia or hypercarbia and acidemia suggest nervous system dysfunction
- Paradoxical respiratory motion suggest muscular dysfunction
Evaluation[edit | edit source]
- Arterial blood gases- measures oxygen and carbon dioxide levels in the blood
- Full blood count- may indicate anemia which can contribute to tissue hypoxia; polycythaemia may indicate chronic hypoxaemic respiratory failure; thrombocytopenia may suggest sepsis
- Renal function tests and liver function tests- may indicate the etiology of respiratory failure or identify complications associated with it.
- Pulmonary function test- identifies obstruction, restriction, and gas diffusion abnormalities. Normal values for forced expiratory volume in 1 second(FEV1) and forced vital capacity(FVC) suggest a disturbance in respiratory control. Decrease in FEV1 to FVC ratio indicates airflow obstruction. A decrease in FEV1 and FVC and maintenance of FEV1 to FVC ratio suggest restrictive lung disease.
- Electrocardiography(ECG)- determines if respiratory failure is from a cardiovascular cause, may detect dysrhythmias from hypoxaemia or acidosis
- Echocardiography- needed when a cardiac cause of acute respiratory failure is suspected. Findings such as left ventricular dilatation, regional/global wall motion abnormalities or severe mitral regurgitation verify the diagnosis of cardiogenic pulmonary edema. Normal heart size and normal systolic and diastolic function in a patient with pulmonary edema suggests acute respiratory distress syndrome
- Chest radiography- reveals the cause of respiratory failure
- Serum creatinine kinase with fractionation and troponin I- excludes recent myocardial infarction in a patient with RF. Elevated levels of creatinine kinase with normal troponin I levels may indicate myositis- causes respiratory failure occasionally
- Thyroid function tests- hypothyroidism may cause chronic hypercapnic respiratory failure
Complications[edit | edit source]
Multiple organ-system complications involving the cardiovascular, pulmonary, gastrointestinal system may occur subsequent to respiratory failure
- Pulmonary: pulmonary embolism, pulmonary fibrosis, complications secondary to the use of mechanical ventilator
- Cardiovascular: hypotension, reduced cardiac output, cor pulmonale, arrhythmias, pericarditis and acute myocardial infarction
- Gastrointestinal: haemorrhage, gastric distention, ileus, diarrhoea, pneumoperitoneum and duodenal ulceration- caused by stress is common in patients with acute respiratory failure
- Infectious: noscomial- pneumonia, urinary tract infection and catheter-related sepsis. Usually occurs with use of mechanical devices.
- Renal: acute renal failure, abnormalities of electrolytes and acid-base balance.
- Nutritional: malnutrition and complications relating to parenteral or enteral nutrition and complications associated with NG tube- abdominal distention and diarrhea
Management[edit | edit source]
This includes supportive measures and treatment of the underlying cause.
Supportive measures which depend on depending on airways management to maintain adequate ventilation and correction of the blood gases abnormalities
- Correction of Hypoxemia
- The goal is to maintain adequate tissue oxygenation, generally achieved with an arterial oxygen tension (PaO2) of 60 mm Hg or arterial oxygen saturation (SaO2), about 90%.
- Un-controlled oxygen supplementation can result in oxygen toxicity and CO2 (carbon dioxide) narcosis. Inspired oxygen concentration should be adjusted at the lowest level, which is sufficient for tissue oxygenation.
- Oxygen can be delivered by several routes depending on the clinical situations in which we may use a nasal cannula, simple face mask nonrebreathing mask, or high flow nasal cannula.
- Extracorporeal membrane oxygenation may be needed in refractory cases
2. Correction of hypercapnia and respiratory acidosis
- This may be achieved by treating the underlying cause or providing ventilatory support.
3. Ventilatory support for the patient with respiratory failure
The goals of ventilatory support in respiratory failure are:
- Correct hypoxemia
- Correct acute respiratory acidosis
- Resting of ventilatory muscles[1]
Non-invasive respiratory support: is ventilatory support without tracheal intubation/ via upper airway. Considered in patients with mild to moderate respiratory failure. Patients should be conscious, have an intact airway and airway protective reflexes. Noninvasive positive pressure ventilation(NIPPV) has been shown to reduce complications, duration of ICU stay and mortality(). It has been suggested that NIPPV is more effective in preventing endotracheal intubation in acute respiratory failure due to COPD than other causes. The etiology of respiratory failure is an important predictor of NIPPV failure.[4]
Invasive respiratory support: indicated in persistent hypoxemia despite receiving maximum oxygen therapy, hypercapnia with impairment of conscious level. Intubation is associated with complications such as aspiration of gastric content, trauma to the teeth, barotraumas, trauma to the trachea etc
- Permissive hypercapnia[5] - A ventilatory strategy that allows arterial carbon dioxide(PaCO2) to rise by accepting a lower alveolar minute ventilation to avoid the risk of ventilator-associated lung injury in patients with ALI and minimize intrinsic positive end-expiratory pressure (auto PEEP) in patients with COPD thereby protecting the lungs from barotrauma. Permissive hypercapnia could increase survival in immunocompromised children with severe ARDS[6]
Physiotherapy Management[edit | edit source]
In mechanically ventilated patients, early physiotherapy has been shown to improve quality of life and to prevent ICU-associated complications like de-conditioning, ventilator dependency and respiratory conditions. Main indications for physiotherapy are excessive pulmonary secretions and atelectasis. Timely physical therapy interventions may improve gas exchange and reverse pathological progression thereby avoiding ventilation. Ultimately, physio-therapeutic interventions aim to maximize function in motor, ventilatory and improve quality of life. Interventions include:
- Positioning: the use of specific body position aimed at improving ventilation/perfusion(V/Q) matching, promoting mucociliary clearance, improving aeration via increased lung volumes and reducing the work of breathing.[7] These include:
- Prone: helps to improve V/Q matching, redistribute edema and increase functional residual capacity(FRC) in patients with acute respiratory distress syndrome. It has been shown to result in oxygenation for 52-92% of patients with severe acute respiratory failure.[8][9]
- Side-lying: with affected lungs uppermost to improve aeration through increased lung volumes in patients with unilateral lung disease.
- Semi-recumbent: 450 head-up position serves to prevent the risk of gastroesophageal reflux and aspiration.
- Upright: helps to improve lung volumes and decrease work of breathing in patients that are being weaned from mechanical ventilator.
- Postural drainage: uses gravitational effects to facilitate mucociliary clearance
- Suction: used for clearing secretions when the patient cannot do so independently. Guglielminotti et al recommended a saw-tooth pattern seen on ventilator’s flow-volume loop and/or respiratory sounds over the trachea as good indicators for tracheal suction in a ventilated patient[10]
- Manual Hyperinflation: aims to re-inflate atelectatic areas of the lung as such improving pulmonary compliance[11] and facilitate the clearance of pulmonary secretions when used with other techniques.
- Active cycle of breathing technique[12] and manual techniques such as shaking and vibration to facilitate mucus clearance
- Limb exercises: passive, active-assisted, active exercises may optimize oxygen transport and reduce the effects of immobility.[7]
- Inspiratory muscle training: aims to improve inspiratory muscle strength and it facilitates weaning from mechanical ventilation. It has be shown to improve whole body exercise performance, particularly in less fit subjects.[13] The study by Hoffman L et showed positive outcomes with inspiratory muscle training in patients with advanced lung disease.[14]
Differential Diagnosis[edit | edit source]
- Acute Respiratory Distress Syndrome
- Angina Pectoris
- Aspiration Pneumonitis
- Asthma
- Atelectasis
- Cardiogenic shock
- Obstructive sleep apnea
- Myocardial infarction
- Pulmonary embolism
Prognosis[edit | edit source]
Respiratory failure is associated with poor prognosis but advances in mechanical ventilation and airway management have improved prognosis. It is dependent on the underlying cause of respiratory failure. Mortality rates of approximately 40-45% which has remained constant over the years occur with acute respiratory distress syndrome(ARDS)[18][19] with younger patients(< 60 years) having better survival rates. About two-thirds of the patients who survive an episode of ARDS show some impairment of pulmonary function one or more years of post-recovery. For COPD and acute respiratory failure. overall mortality has reportedly declined from 26% to 10%. Also, significant mortality occurs in patients with hypercapnic respiratory failure due to associated co-morbidities and poor nutritional status. Noveanu et al's study show a strong association between preadmission use of beta-blockers and in-hospital and 1-year mortality among patients with acute respiratory failure.[20]
Resources[edit | edit source]
European Respiratory Society/American Thoracic Society Clinical guideline for non-invasive ventilation in acute respiratory failure.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 Shebl E, Burns B. Respiratory failure..Available from:https://www.ncbi.nlm.nih.gov/books/NBK526127/?report=printable (last accessed 28.9.2020)
- ↑ Hall JB, Schmidt GA, Wood LD. Acute hypoxemic respiratory failure In: Murray, JF, Nadel, JA. editors. Textbook of Respiratory Medicine. Philadephia, PA:Saunders, 2000. p2413-2442.
- ↑ 3.0 3.1 3.2 Shebl, Eman, and Bracken Burns. "Respiratory Failure." (2018).
- ↑ Agarwal R, Gupta R, Aggarwal AN, Gupta D. Noninvasive positive pressure ventilation in acute respiratory failure due to COPD vs other causes: effectiveness and predictors of failure in a respiratory ICU in North India. Int J Chron Obstrut Pulmon Dis. 2008;3(4):737-43.
- ↑ Mackenzie I, editor. Core Topics in Mechanical Ventilation. Cambridge: Cambridge University Press, 2008. p153.
- ↑ Fuchs H, Rossmann N, Schmid MB, Hoenig M, Thome U, Mayer B, et al. Permissive hypercapnia for severe acute respiratory distress syndrome in immunocompromised children: A single center experience. PLoS One. 2017;12(6):e0179974.
- ↑ 7.0 7.1 Dean E. Oxygen transport: a physiologically-based conceptual framework for the practice of cardiopulmonary Physiotherapy. Physiotherapy. 1994; 80(6): 347-354
- ↑ Jolliet P, Bulpa P, Chevrolet JC. Effects of the prone position on gas exchange and hemodynamics in severe acute respiratory distress syndrome. Crit Care Med. 1998; 26(12):1977-1985
- ↑ Mure M, Martling CR, Lindahl SG. Dramatic effect on oxygenation in patients with severe acute lung insufficiency treated in prone position.Crit Care Med. 1997; 25(9):1539-1544
- ↑ Guglielminotti J, Alzieu M, Maury E, Guidet B, Offenstadt G. Bedside detection of retained tracheobronchial secretions in patients receiving mechanical ventilation: is it time for tracheal suctioning?Chest. 2000;118(4):1095-9.
- ↑ Clarke RCN, Kelly BE. Ventilatory characteristics in mechanically ventilated patients during manual hyperinflation for chest physiotherapy. Anaesthesia. 1999; 54: 936-940
- ↑ Inal-Ince D, Savci S, Topeli A, Arikan H. Active cycle of breathing techniques in non-invasive ventilation for acute hypercapnic respiratory failure. Aust J Physiother. 2004;50(2):67-73.
- ↑ Illi SK, Held U,Frank I, Spengler CM. Effect of respiratory muscle training on exercise performance in healthy individuals: a systematic review and meta-analysis. Sport Med. 2012;42(8):707-24.
- ↑ Hoffman M, Augusto VM, Eduardo DS, Silveira BM, Lemos MD, Parreira VF. Inspiratory muscle training reduces dyspnea during activities of daily living and improves inspiratory muscle function and quality of life in patients with advanced lung disease. Physiotherapy theory and practice. 2019 Aug 21:1-1.
- ↑ Hodgson CL, Bailey M, Bellomo R, Berney S, Buhr H, Denehy L, et al. A binational multicenter pilot feasibility randomized controlled trial of early goal-directed mobilization in the ICU. Crit Care Med. 2016; 44(6):1145-1152
- ↑ Schaller SJ, Anstey M, Blobner M, Edrich T, Grabitz SD, Gradwohl-Matis I, et al. Early, goal-directed mobilisation in the surgical intensive care unit: a randomised controlled trial. Lancet. 2016;388(10052):1377-1388
- ↑ Kayambu G, Boots R, Paratz J. Early physical rehabilitation in intensive care patients with sepsis syndromes: a pilot randomised controlled trial. Intensive Care Med. 2015; 41(15):865-874
- ↑ Phua J, Badia JR, Adhikari NK. Has mortality from acute respiratory distress syndrome decreased over time? A systematic review. Am J Respir Crit Care Med. 2009; 179(3): 220-227.
- ↑ Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, et al. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and acute respiratory distress syndrome. N Engl J Med. 2000; 342(18):1301-8.
- ↑ Noveanu M, Breidthardt T, Reichlin H, Gayat E, Potocki M, Pragger H, et al. Effect of oral beta-blocker on short term and long term mortality in patients with acute respiratory failure: results from the BASEL-II-ICU study. Crit Care. 2010; 14(6): R198.doi: 10.1186/cc9317.