Proprioception: Difference between revisions
(intro) |
Amanda Ager (talk | contribs) No edit summary |
||
| (15 intermediate revisions by 4 users not shown) | |||
| Line 2: | Line 2: | ||
'''Original Editor '''- The [[Open Physio]] project. | '''Original Editor '''- The [[Open Physio]] project. | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} <br> | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
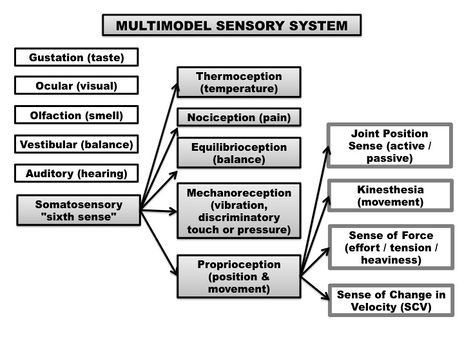
'''Proprioception''' is | '''Proprioception (sense of body positioning in space)''' is an important bodily neuromuscular sense. It falls under our "sixth sense", more commonly known as somatosensation. The term somatosensation (or somatosensory senses) is an all encompassing term which includes the sub-categories of mechanoreception (vibration, pressure, discriminatory touch), thermoreception (temperature), nociception (pain), equilibrioception (balance) and proprioception (sense of positioning and movement).<ref>Ager, A.L., Borms, D., Deschepper, L., Dhooghe, R., Dijkhuis, J., Roy, J.S., & Cools, A.Proprioception and shoulder pain: A Systematic Review. ''J Hand Ther''. 2019 Aug 31. pii: S0894-1130(19)30094-8. doi: 10.1016/j.jht.2019.06.002. </ref> The feedback from all these different sensory components arise from our peripheral nervous system (PNS), and feed information to our central nervous system (CNS), both at the level of the spinal cord (reflexive) and sent to the cerebral cortex for higher processing.<ref>''Guyton AC. Textbook of Medical Physiology. 8th ed. Philadelphia, PA WB Saunders; 1992.''</ref> | ||
Proprioception itself can be understood as including various sub-modalities: | |||
'''<u>Joint Position Sense:</u>''' Proprioception is our sense of joint / limb positioning. It is often measured through joint position sense - active joint position sense (AJPS) and passive joint position sense (PJPS). Joint position sense determines the ability of a person to perceive a presented joint angle and then, after the limb has been moved, to actively or passively reproduces the same joint angle<ref name=":1">Riemann, B. L., & Lephart, S.M. (2002). The sensorimotor system, part 1: the physiological basis of functional joint stability. ''Journal of Athletic Training, 37''(1),71-79.</ref> (Clinically measured as a joint matching task). | |||
'''<u>Kinaesthesia:</u>''' Kinaesthesia (kinaesthesis) is the awareness of motion of the human body (motion sense).<ref>Sherrington CS. On the proprio-ceptive system, especially in its reflex aspect. Brain. 1907;29:467–482.</ref> Sense of movement refers to the ability to appreciate joint movement, including the duration, direction, amplitude, speed, acceleration and timing of movements.<ref name=":1" /> | |||
'''<u>Sense of Force:</u>''' Sense of Force (SoF) is also known as sense of effort / heaviness / tension or the force matching sense. It is the ability to reproduce (or match) a desired level of force one or more times. Sense of force is thought to stem from the afferent feedback of the Golgi Tendon Organs (GTOs) embedded within our tendons, the muscle spindles within our muscles and proprioceptions within our skin.<ref>Hung, Y. J. (2015). Neuromuscular control and rehabilitation of the unstable ankle. ''World Journal of Orthopedics'', ''6''(5), page 434.</ref> | |||
'''<u>Sense of Change in Velocity (SoV):</u>''' SoV is our ability to detect vibration, derived from oscillating objects placed against the skin.<ref>Gilman, S., ''Joint position sense and vibration sense: anatomical organisation and assessment.''Journal of neurology, neurosurgery, and psychiatry, 2002. '''73'''(5): p. 473-7.</ref> It is believed to travel through the same type of large afferent nerve fibers (Aαβ) as proprioception.<ref>Shakoor, N., A. Agrawal, and J.A. Block, ''Reduced lower extremity vibratory perception in osteoarthritis of the knee.''Arthritis and rheumatism, 2008. '''59'''(1): p. 117-21.</ref> | |||
[[File:Somatosensation.jpg|thumb|464x464px|Somatosensation. Retrieved from: Ager, A.L., Borms, D., Deschepper, L., Dhooghe, R., Dijkhuis, J., Roy, J.S., & Cools, A.Proprioception and shoulder pain: A Systematic Review. ''J Hand Ther''. 2019 Aug 31. pii: S0894-1130(19)30094-8. doi: 10.1016/j.jht.2019.06.002. ]] | |||
Globally, all sub-modalities of proprioception arise from the sum of neural inputs from the joint capsules, ligaments, muscles, tendons, and skin, in a multifaceted system, which influences behavior regulation and motor control of the body.<ref>Blanche, E.I., Bodison, S., Chang, M.C., & Reinoso, G. (2012). Development of the Comprehensive Observations of Proprioception (COP): Validity, Reliability, and Factor Analysis. Am J Occup Ther. 66(6): 691–698. doi:10.5014/ajot.2012.003608.</ref> | |||
Proprioception is critical for meaningful interactions with our surrounding environment. Proprioception helps with the planing of movements, sport performance, playing a musical instrument and ultimately helping us avoid an injury. | |||
The neurological basis of proprioception comes primarily from sensory receptors (mechanoreceptors and proprioceptors) located in your skin, joints, and muscles (muscle spindles with a smaller component from tendon organ afferents, cutaneous receptors and minimal input from joint receptors). These muscle afferents receptors allow for the identification of limb position and movement via neural signalling of a change in muscle, skin or joint stretch<ref>Suetterlin KJ, Sayer AA. [https://academic.oup.com/ageing/article/43/3/313/16765 Proprioception: where are we now? A commentary on clinical assessment, changes across the life course, functional implications and future interventions.] Age and ageing. 2013 Nov 14;43(3):313-8. Available from: https://academic.oup.com/ageing/article/43/3/313/16765 (last accessed 31.10.19)</ref>. Hence, proprioception is basically a continuous loop of feedforward and feedback inputs between sensory receptors throughout your body and your nervous system. | |||
A mechanoreceptor is a sensory receptor in your body that responds to mechanical changes of tissues. Different types of mechanoreceptors include | |||
A | * Pacinian Corpuscles | ||
* Meissner's Corpuscles | |||
* Merkel's Discs | |||
* Ruffini Corpuscles | |||
* Golgi Tendon Organs (GTO) | |||
* Free nerve endings | |||
There are also mechanoreceptors within the hair and skin. | |||
''' | There are four types of mechanoreceptors found within ligamentous tissues. As all the types of mechanoreceptors are myelinated and rapidly transmit sensory information to the CNS.<ref name=":2">Michelson JD, Hutchins C. (1995). Mechanoreceptors in human ankle ligaments. ''The Journal of Bone and Joint Surgery. British Volume''. '''77''' (2): 219–24. PMID [https://www.ncbi.nlm.nih.gov/pubmed/7706334 7706334].</ref> | ||
* | * '''Type I''': (small) Low threshold, slow adapting in both static and dynamic settings; | ||
* | * '''Type II''': (medium) Low threshold, rapidly adapting in dynamic settings; | ||
* | * '''Type III''': (large) High threshold, slowly adapting in dynamic settings; | ||
''' | * '''Type IV''': (very small) High threshold pain receptors that communicate injury. | ||
Type II and Type III mechanoreceptors in particular are believed to be linked to one's sense of proprioception.<ref name=":2" /> | |||
* | |||
The short video below gives a good insight into the complexities of proprioception. | |||
{{#ev:youtube|https://www.youtube.com/watch?v=Dzlkz8j-8rg|width}}<ref>W Deloriea Proprioceptors Available from: https://www.youtube.com/watch?v=Dzlkz8j-8rg ( last accessed 30.10.2019)</ref> | |||
== Proprioception | === Causes of Proprioception Impairment === | ||
Poor proprioception at a joint may result in the increased likelihood of an injury.<ref>Anderson, V. B., & Wee, E. (2011). Impaired joint proprioception at higher shoulder elevations in chronic rotator cuff pathology. ''Arch Phys Med Rehabil, 92''(7), 1146-1151. doi:10.1016/j.apmr.2011.02.004</ref> The reason for proprioception impairments are not clear at this time. A decreased sense of proprioception can be caused by localized tissue damage, the presence of edema (swelling) or competitive nociceptive inputs (presence off pain). | |||
Proprioception can be affected by the following factors: | |||
* Temporary impairment from a compromised state (for example the consumption of [[Alcoholism|alcohol]]). | |||
* Age-related changes also affect proprioception. The risk of proprioception loss increases as we age due to a combination of natural age-related changes to the nerves, joints, and muscles. | |||
* Injuries or medical conditions that affect the neuromuscular system (muscles, nerves, and the [[cerebellum]], CNS) which can cause long-term or permanent proprioception impairment. | |||
Proprioception impairments have been noted among the following neurological conditions: | |||
* Brain injuries; multiple sclerosis ([[Multiple Sclerosis (MS)|MS]]); stroke; [[Parkinson's|Parkinson’s]] disease; [[Huntington Disease|Huntington’s]] disease; [[Amyotrophic Lateral Sclerosis |ALS]] (amyotrophic lateral sclerosis) | |||
* Also health conditions: herniated [[Disc Herniation|disc]]; [[Osteoarthritis|arthritis]]; autism spectrum disorder (ASD); [[diabetes]]; [[Neuropathies|peripheral neuropathy]]. | |||
* Post-surgery: joint replacement surgery, such as [[Total Hip Replacement|hip replacement]] or [[Total Knee Arthroplasty|knee replacement]] | |||
* MSK conditions: ankle sprains, ACL injuries, shoulder dislocations and tendinopathies, whiplash associated disorders (among others). | |||
== Assessing Proprioception == | |||
The measurement of proprioception is presently not well developed. Proprioception can only be confidently measured in a laboratory setting, using complex computer-interfaced equipment. There is presently a lack of valid, reliable and responsive tools and outcome measures to quantify proprioception deficits, in a clinical setting.<ref>Ager, A.L.,Roy, J.S., Roos, M., Belley, A.F., Cools, A., & Hebert, L.J. (2017). Shoulder proprioception: How is it measured and is it reliable? A systematic review. ''J Hand Ther.,''30(2), 221-231. doi: 10.1016/j.jht.2017.05.003.</ref> | |||
If you suspect a proprioception deficit, focus on the following clinical aspects. | |||
'''Subjective assessment''' should include questions regarding the following: | |||
* Balance issues, such as having trouble standing on one foot or frequent falls while walking or sitting; | |||
* Uncoordinated movement ([[ataxia]]), such as not being able to walk in a straight line, or difficulty reaching for an object; | |||
* The avoidance of certain activities, such as climbing stairs or walking on uneven surfaces because of a fear of falling. | |||
'''Objective assessment''' should include observation of the above and the points below: | |||
* Overal coordination (Reaching tests, Star Excurtion Balance Test, Upper extremity coordination tests); | |||
* Clumsiness, such as dropping or bumping into things; | |||
* Poor postural control, such as slouching or having to place extra weight on a table for balance while sitting; | |||
* Trouble recognizing the appropriate level of muscular strength for a task (for example: pressing on a pen too hard when writing or not being able to gauge the force needed to pick up an object). | |||
There are a few clinical tests Physiotherapists can use to assess proprioception, depending on the body part being assessed. The include: | |||
* [[Romberg Test|Romberg test]]; | |||
* '''Heel-shin.''' The patient is asked to touch the heel of one foot to the opposite knee and then to drag their heel in a straight line all the way down the front of their shin and back up again. In order to eliminate the effect of gravity in moving the heel down the shin, this test should always be done in the supine position. | |||
* '''Ataxia'''. Best revealed if the examiner's finger is held at the extreme of the patient's reach, and if the examiner's finger is occasionally moved suddenly to a different location. | |||
*'''Finger—nose—finger test.''' The patient is asked to alternately touch their nose and the examiner's finger as quickly as possible | |||
*'''Distal proprioception test.''' The tester will move the joints of the hip, knee ankle and big toe up and down while you watch. You then ask the client to repeat the same movement with your eyes closed. | |||
*'''A contralateral joint matching task.''' Asking the patient to match a demonstrated joint angle, and measuring the difference between the actual joint angle, and the reproduced joint angle (the difference representing the proprioception error). | |||
=== Learning New Skills === | |||
An intact sense of proprioception is crucial to learning a new skill. During the learning of any new skill, (sport performance or an artistic activity, for example) it is usually necessary to become familiar with some proprioceptive tasks specific to that activity. Without the appropriate integration of proprioceptive input, an artist would not be able to brush paint onto a canvas without looking at the hand as it moved the brush over the canvas; it would be impossible to drive an automobile because a motorist would not be able to steer or use the foot pedals while looking at the road ahead. A person could not touch-type (typing without looking at the keys) or perform a ballet dance. The bottom line remains that our sense of proprioception is important to train and develop, as it allows us to interact with our environments without the dependence on visual feedback (for example, reaching for a cup on the top shelve, without looking at the cup). | |||
== Physiotherapy - Training Proprioception == | == Physiotherapy - Training Proprioception == | ||
No matter the underlying cause | No matter the underlying cause of a proprioceptive deficit, clinicians can rehabilitate patients with tasks and activities to improve motor skills, strength, balance and coordination. They can also help patients learn how to manage daily tasks (ADLs) while living with a proprioception dysfunction. | ||
There is converging evidence that proprioceptive training can yield meaningful improvements in somatosensory and sensorimotor function.<ref>Aman JE, Elangovan N, Yeh I, Konczak J. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4309156/ The effectiveness of proprioceptive training for improving motor function: a systematic review]. Frontiers in human neuroscience. 2015 Jan 28;8:1075. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4309156/ (last accessed 31.10.2019)</ref> Retraining of a somatosensory function includes any interventions that addresses the remediation of the somatosensory modalities. Intervention methods include: | |||
* '''Education;''' | |||
* '''Repetitive practice and feedback in detecting, localising, discriminating, or recognising different sensory stimuli, pressure, or objects; PRACTICE, PRACTICE, PRACTICE!''' | |||
* '''Proprioceptive training;''' | |||
* '''Balance training (unstable surfaces, unpredictable situations with an external stimuli);''' | |||
* '''Dual task training (in the absence of visual feedback for example)''' | |||
* '''Somatosensory stimulation,<ref name=":0">Chia FS, Kuys S, [https://journals.sagepub.com/doi/full/10.1177/0269215519836461 Low Choy N. Sensory retraining of the leg after stroke: systematic review and meta-analysis.] Clinical rehabilitation. 2019 Jun;33(6):964-79. Available from: https://journals.sagepub.com/doi/full/10.1177/0269215519836461 (last accessed 31.10,2019)</ref>''' | |||
A 2019 review on sensory retraining of the leg following a stroke, concluded that interventions used for retraining leg somatosensory impairment significantly improved somatosensory function and balance, but not gait suggesting a specificity of training effect.<ref name=":0" /> | |||
* | A 2005 systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed anterior cruciate ligaments, reported that proprioceptive and balance exercise improves outcomes in individuals with ACL-deficient knees.<ref>Cooper RL, Taylor NF, Feller JA. [https://www.tandfonline.com/doi/full/10.1080/15438620590956197 A systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed anterior cruciate ligament.] Research in sports medicine. 2005 Apr 1;13(2):163-78. Available from: https://www.tandfonline.com/doi/full/10.1080/15438620590956197 (last accessed 31.10.2019)</ref> Similarly a 2015 review on ankle sprains amongst a sporting population, concluded that proprioceptive training programmes are effective at reducing the rate of re-injury, particularly amongst those with a history of ankle sprain.<ref>Schiftan GS, Ross LA, Hahne AJ. [https://www.jsams.org/article/S1440-2440(14)00074-7/fulltext The effectiveness of proprioceptive training in preventing ankle sprains in sporting populations: a systematic review and meta-analysis]. Journal of Science and Medicine in Sport. 2015 May 1;18(3):238-44. Available from: https://www.jsams.org/article/S1440-2440(14)00074-7/fulltext (last accessed 31.10.2019)</ref> | ||
The effectiveness of physiotherapy treatment on balance dysfunction and postural instability in persons with Parkinson’s disease: a systematic review and meta-analysis in 2016 reported that physiotherapy interventions like balance training combined with muscle strengthening, range of movement and walking training exercise is effective in improving balance in patients with Parkinson’s disease. As proprioception can also be improved with balance training, this could possibly advocate for proprioceptive retraining as well, amongst this population.<ref>Yitayeh A, Teshome A. [https://bmcsportsscimedrehabil.biomedcentral.com/articles/10.1186/s13102-016-0042-0 The effectiveness of physiotherapy treatment on balance dysfunction and postural instability in persons with Parkinson’s disease: a systematic review and meta-analysis]. BMC sports science, medicine and rehabilitation. 2016 Dec;8(1):17. Available from: https://bmcsportsscimedrehabil.biomedcentral.com/articles/10.1186/s13102-016-0042-0 (last accessed 31.10.2019)</ref> | |||
==== Proprioception rehabilitation often include: ==== | |||
*[[File:SLS balance on bosu.jpg|right|frameless|300x300px]]'''1. Balance exercises.''' Standing on a Balance board is often used to retrain or increase proprioception abilities, particularly as physical therapy for ankle or knee injuries. You can also perform weight bearing exercises on an unstable surface (such as a Bosu Ball or stability disc) for the upper extremities (such as push ups, or simply weight bearing on elbows or an outstretched arm position). [[File:Taoist Tai Chi class.jpg|right|frameless|214x214px]]'''2. [[Tai Chi and the Older Person|Tai Chi]],''' which improves lower limb proprioception and Yoga, which improves balance and muscle strength. The slow, focused movements of Tai Chi practice provide an environment whereby the proprioceptive information being fed back to the brain stimulates an intense, dynamic "listening environment" to further enhance mind / body integration. | |||
'''3. somatosensory stimulation training''', such as vibration therapy, different textures (cotton ball vs. velcro); | |||
'''4. Joint repositioning training''' (joint matching tasks). | |||
For complimentary topics, please read the following pages: | |||
[[Neuromuscular Exercise Program]] | [[Neuromuscular Exercise Program]] | ||
| Line 87: | Line 115: | ||
[[Developmental Coordination Disorder and Physical Activity]] | [[Developmental Coordination Disorder and Physical Activity]] | ||
[[Sensorimotor Impairment in Neck Pain]] | [[Sensorimotor Impairment in Neck Pain]] | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Open_Physio]] | [[Category:Open_Physio]] | ||
[[Category:Falls]] | [[Category:Falls]] | ||
Latest revision as of 14:00, 18 August 2023
Original Editor - The Open Physio project.
Top Contributors - Lucinda hampton, Admin, Amanda Ager, Kim Jackson, Vanessa Rhule, Paule Morbois, Scott Buxton, Naomi O'Reilly, WikiSysop, Tarina van der Stockt, Claire Knott, Amrita Patro, Wanda van Niekerk, Rishika Babburu and Rachael Lowe
Introduction[edit | edit source]
Proprioception (sense of body positioning in space) is an important bodily neuromuscular sense. It falls under our "sixth sense", more commonly known as somatosensation. The term somatosensation (or somatosensory senses) is an all encompassing term which includes the sub-categories of mechanoreception (vibration, pressure, discriminatory touch), thermoreception (temperature), nociception (pain), equilibrioception (balance) and proprioception (sense of positioning and movement).[1] The feedback from all these different sensory components arise from our peripheral nervous system (PNS), and feed information to our central nervous system (CNS), both at the level of the spinal cord (reflexive) and sent to the cerebral cortex for higher processing.[2]
Proprioception itself can be understood as including various sub-modalities:
Joint Position Sense: Proprioception is our sense of joint / limb positioning. It is often measured through joint position sense - active joint position sense (AJPS) and passive joint position sense (PJPS). Joint position sense determines the ability of a person to perceive a presented joint angle and then, after the limb has been moved, to actively or passively reproduces the same joint angle[3] (Clinically measured as a joint matching task).
Kinaesthesia: Kinaesthesia (kinaesthesis) is the awareness of motion of the human body (motion sense).[4] Sense of movement refers to the ability to appreciate joint movement, including the duration, direction, amplitude, speed, acceleration and timing of movements.[3]
Sense of Force: Sense of Force (SoF) is also known as sense of effort / heaviness / tension or the force matching sense. It is the ability to reproduce (or match) a desired level of force one or more times. Sense of force is thought to stem from the afferent feedback of the Golgi Tendon Organs (GTOs) embedded within our tendons, the muscle spindles within our muscles and proprioceptions within our skin.[5]
Sense of Change in Velocity (SoV): SoV is our ability to detect vibration, derived from oscillating objects placed against the skin.[6] It is believed to travel through the same type of large afferent nerve fibers (Aαβ) as proprioception.[7]
Globally, all sub-modalities of proprioception arise from the sum of neural inputs from the joint capsules, ligaments, muscles, tendons, and skin, in a multifaceted system, which influences behavior regulation and motor control of the body.[8]
Proprioception is critical for meaningful interactions with our surrounding environment. Proprioception helps with the planing of movements, sport performance, playing a musical instrument and ultimately helping us avoid an injury.
The neurological basis of proprioception comes primarily from sensory receptors (mechanoreceptors and proprioceptors) located in your skin, joints, and muscles (muscle spindles with a smaller component from tendon organ afferents, cutaneous receptors and minimal input from joint receptors). These muscle afferents receptors allow for the identification of limb position and movement via neural signalling of a change in muscle, skin or joint stretch[9]. Hence, proprioception is basically a continuous loop of feedforward and feedback inputs between sensory receptors throughout your body and your nervous system.
A mechanoreceptor is a sensory receptor in your body that responds to mechanical changes of tissues. Different types of mechanoreceptors include
- Pacinian Corpuscles
- Meissner's Corpuscles
- Merkel's Discs
- Ruffini Corpuscles
- Golgi Tendon Organs (GTO)
- Free nerve endings
There are also mechanoreceptors within the hair and skin.
There are four types of mechanoreceptors found within ligamentous tissues. As all the types of mechanoreceptors are myelinated and rapidly transmit sensory information to the CNS.[10]
- Type I: (small) Low threshold, slow adapting in both static and dynamic settings;
- Type II: (medium) Low threshold, rapidly adapting in dynamic settings;
- Type III: (large) High threshold, slowly adapting in dynamic settings;
- Type IV: (very small) High threshold pain receptors that communicate injury.
Type II and Type III mechanoreceptors in particular are believed to be linked to one's sense of proprioception.[10]
The short video below gives a good insight into the complexities of proprioception.
Causes of Proprioception Impairment[edit | edit source]
Poor proprioception at a joint may result in the increased likelihood of an injury.[12] The reason for proprioception impairments are not clear at this time. A decreased sense of proprioception can be caused by localized tissue damage, the presence of edema (swelling) or competitive nociceptive inputs (presence off pain).
Proprioception can be affected by the following factors:
- Temporary impairment from a compromised state (for example the consumption of alcohol).
- Age-related changes also affect proprioception. The risk of proprioception loss increases as we age due to a combination of natural age-related changes to the nerves, joints, and muscles.
- Injuries or medical conditions that affect the neuromuscular system (muscles, nerves, and the cerebellum, CNS) which can cause long-term or permanent proprioception impairment.
Proprioception impairments have been noted among the following neurological conditions:
- Brain injuries; multiple sclerosis (MS); stroke; Parkinson’s disease; Huntington’s disease; ALS (amyotrophic lateral sclerosis)
- Also health conditions: herniated disc; arthritis; autism spectrum disorder (ASD); diabetes; peripheral neuropathy.
- Post-surgery: joint replacement surgery, such as hip replacement or knee replacement
- MSK conditions: ankle sprains, ACL injuries, shoulder dislocations and tendinopathies, whiplash associated disorders (among others).
Assessing Proprioception[edit | edit source]
The measurement of proprioception is presently not well developed. Proprioception can only be confidently measured in a laboratory setting, using complex computer-interfaced equipment. There is presently a lack of valid, reliable and responsive tools and outcome measures to quantify proprioception deficits, in a clinical setting.[13]
If you suspect a proprioception deficit, focus on the following clinical aspects.
Subjective assessment should include questions regarding the following:
- Balance issues, such as having trouble standing on one foot or frequent falls while walking or sitting;
- Uncoordinated movement (ataxia), such as not being able to walk in a straight line, or difficulty reaching for an object;
- The avoidance of certain activities, such as climbing stairs or walking on uneven surfaces because of a fear of falling.
Objective assessment should include observation of the above and the points below:
- Overal coordination (Reaching tests, Star Excurtion Balance Test, Upper extremity coordination tests);
- Clumsiness, such as dropping or bumping into things;
- Poor postural control, such as slouching or having to place extra weight on a table for balance while sitting;
- Trouble recognizing the appropriate level of muscular strength for a task (for example: pressing on a pen too hard when writing or not being able to gauge the force needed to pick up an object).
There are a few clinical tests Physiotherapists can use to assess proprioception, depending on the body part being assessed. The include:
- Romberg test;
- Heel-shin. The patient is asked to touch the heel of one foot to the opposite knee and then to drag their heel in a straight line all the way down the front of their shin and back up again. In order to eliminate the effect of gravity in moving the heel down the shin, this test should always be done in the supine position.
- Ataxia. Best revealed if the examiner's finger is held at the extreme of the patient's reach, and if the examiner's finger is occasionally moved suddenly to a different location.
- Finger—nose—finger test. The patient is asked to alternately touch their nose and the examiner's finger as quickly as possible
- Distal proprioception test. The tester will move the joints of the hip, knee ankle and big toe up and down while you watch. You then ask the client to repeat the same movement with your eyes closed.
- A contralateral joint matching task. Asking the patient to match a demonstrated joint angle, and measuring the difference between the actual joint angle, and the reproduced joint angle (the difference representing the proprioception error).
Learning New Skills[edit | edit source]
An intact sense of proprioception is crucial to learning a new skill. During the learning of any new skill, (sport performance or an artistic activity, for example) it is usually necessary to become familiar with some proprioceptive tasks specific to that activity. Without the appropriate integration of proprioceptive input, an artist would not be able to brush paint onto a canvas without looking at the hand as it moved the brush over the canvas; it would be impossible to drive an automobile because a motorist would not be able to steer or use the foot pedals while looking at the road ahead. A person could not touch-type (typing without looking at the keys) or perform a ballet dance. The bottom line remains that our sense of proprioception is important to train and develop, as it allows us to interact with our environments without the dependence on visual feedback (for example, reaching for a cup on the top shelve, without looking at the cup).
Physiotherapy - Training Proprioception[edit | edit source]
No matter the underlying cause of a proprioceptive deficit, clinicians can rehabilitate patients with tasks and activities to improve motor skills, strength, balance and coordination. They can also help patients learn how to manage daily tasks (ADLs) while living with a proprioception dysfunction.
There is converging evidence that proprioceptive training can yield meaningful improvements in somatosensory and sensorimotor function.[14] Retraining of a somatosensory function includes any interventions that addresses the remediation of the somatosensory modalities. Intervention methods include:
- Education;
- Repetitive practice and feedback in detecting, localising, discriminating, or recognising different sensory stimuli, pressure, or objects; PRACTICE, PRACTICE, PRACTICE!
- Proprioceptive training;
- Balance training (unstable surfaces, unpredictable situations with an external stimuli);
- Dual task training (in the absence of visual feedback for example)
- Somatosensory stimulation,[15]
A 2019 review on sensory retraining of the leg following a stroke, concluded that interventions used for retraining leg somatosensory impairment significantly improved somatosensory function and balance, but not gait suggesting a specificity of training effect.[15]
A 2005 systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed anterior cruciate ligaments, reported that proprioceptive and balance exercise improves outcomes in individuals with ACL-deficient knees.[16] Similarly a 2015 review on ankle sprains amongst a sporting population, concluded that proprioceptive training programmes are effective at reducing the rate of re-injury, particularly amongst those with a history of ankle sprain.[17]
The effectiveness of physiotherapy treatment on balance dysfunction and postural instability in persons with Parkinson’s disease: a systematic review and meta-analysis in 2016 reported that physiotherapy interventions like balance training combined with muscle strengthening, range of movement and walking training exercise is effective in improving balance in patients with Parkinson’s disease. As proprioception can also be improved with balance training, this could possibly advocate for proprioceptive retraining as well, amongst this population.[18]
Proprioception rehabilitation often include:[edit | edit source]
- 1. Balance exercises. Standing on a Balance board is often used to retrain or increase proprioception abilities, particularly as physical therapy for ankle or knee injuries. You can also perform weight bearing exercises on an unstable surface (such as a Bosu Ball or stability disc) for the upper extremities (such as push ups, or simply weight bearing on elbows or an outstretched arm position). 2. Tai Chi, which improves lower limb proprioception and Yoga, which improves balance and muscle strength. The slow, focused movements of Tai Chi practice provide an environment whereby the proprioceptive information being fed back to the brain stimulates an intense, dynamic "listening environment" to further enhance mind / body integration.
3. somatosensory stimulation training, such as vibration therapy, different textures (cotton ball vs. velcro);
4. Joint repositioning training (joint matching tasks).
For complimentary topics, please read the following pages:
Neuromuscular Exercise Program
Developmental Coordination Disorder and Physical Activity
Sensorimotor Impairment in Neck Pain
References[edit | edit source]
- ↑ Ager, A.L., Borms, D., Deschepper, L., Dhooghe, R., Dijkhuis, J., Roy, J.S., & Cools, A.Proprioception and shoulder pain: A Systematic Review. J Hand Ther. 2019 Aug 31. pii: S0894-1130(19)30094-8. doi: 10.1016/j.jht.2019.06.002.
- ↑ Guyton AC. Textbook of Medical Physiology. 8th ed. Philadelphia, PA WB Saunders; 1992.
- ↑ 3.0 3.1 Riemann, B. L., & Lephart, S.M. (2002). The sensorimotor system, part 1: the physiological basis of functional joint stability. Journal of Athletic Training, 37(1),71-79.
- ↑ Sherrington CS. On the proprio-ceptive system, especially in its reflex aspect. Brain. 1907;29:467–482.
- ↑ Hung, Y. J. (2015). Neuromuscular control and rehabilitation of the unstable ankle. World Journal of Orthopedics, 6(5), page 434.
- ↑ Gilman, S., Joint position sense and vibration sense: anatomical organisation and assessment.Journal of neurology, neurosurgery, and psychiatry, 2002. 73(5): p. 473-7.
- ↑ Shakoor, N., A. Agrawal, and J.A. Block, Reduced lower extremity vibratory perception in osteoarthritis of the knee.Arthritis and rheumatism, 2008. 59(1): p. 117-21.
- ↑ Blanche, E.I., Bodison, S., Chang, M.C., & Reinoso, G. (2012). Development of the Comprehensive Observations of Proprioception (COP): Validity, Reliability, and Factor Analysis. Am J Occup Ther. 66(6): 691–698. doi:10.5014/ajot.2012.003608.
- ↑ Suetterlin KJ, Sayer AA. Proprioception: where are we now? A commentary on clinical assessment, changes across the life course, functional implications and future interventions. Age and ageing. 2013 Nov 14;43(3):313-8. Available from: https://academic.oup.com/ageing/article/43/3/313/16765 (last accessed 31.10.19)
- ↑ 10.0 10.1 Michelson JD, Hutchins C. (1995). Mechanoreceptors in human ankle ligaments. The Journal of Bone and Joint Surgery. British Volume. 77 (2): 219–24. PMID 7706334.
- ↑ W Deloriea Proprioceptors Available from: https://www.youtube.com/watch?v=Dzlkz8j-8rg ( last accessed 30.10.2019)
- ↑ Anderson, V. B., & Wee, E. (2011). Impaired joint proprioception at higher shoulder elevations in chronic rotator cuff pathology. Arch Phys Med Rehabil, 92(7), 1146-1151. doi:10.1016/j.apmr.2011.02.004
- ↑ Ager, A.L.,Roy, J.S., Roos, M., Belley, A.F., Cools, A., & Hebert, L.J. (2017). Shoulder proprioception: How is it measured and is it reliable? A systematic review. J Hand Ther.,30(2), 221-231. doi: 10.1016/j.jht.2017.05.003.
- ↑ Aman JE, Elangovan N, Yeh I, Konczak J. The effectiveness of proprioceptive training for improving motor function: a systematic review. Frontiers in human neuroscience. 2015 Jan 28;8:1075. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4309156/ (last accessed 31.10.2019)
- ↑ 15.0 15.1 Chia FS, Kuys S, Low Choy N. Sensory retraining of the leg after stroke: systematic review and meta-analysis. Clinical rehabilitation. 2019 Jun;33(6):964-79. Available from: https://journals.sagepub.com/doi/full/10.1177/0269215519836461 (last accessed 31.10,2019)
- ↑ Cooper RL, Taylor NF, Feller JA. A systematic review of the effect of proprioceptive and balance exercises on people with an injured or reconstructed anterior cruciate ligament. Research in sports medicine. 2005 Apr 1;13(2):163-78. Available from: https://www.tandfonline.com/doi/full/10.1080/15438620590956197 (last accessed 31.10.2019)
- ↑ Schiftan GS, Ross LA, Hahne AJ. The effectiveness of proprioceptive training in preventing ankle sprains in sporting populations: a systematic review and meta-analysis. Journal of Science and Medicine in Sport. 2015 May 1;18(3):238-44. Available from: https://www.jsams.org/article/S1440-2440(14)00074-7/fulltext (last accessed 31.10.2019)
- ↑ Yitayeh A, Teshome A. The effectiveness of physiotherapy treatment on balance dysfunction and postural instability in persons with Parkinson’s disease: a systematic review and meta-analysis. BMC sports science, medicine and rehabilitation. 2016 Dec;8(1):17. Available from: https://bmcsportsscimedrehabil.biomedcentral.com/articles/10.1186/s13102-016-0042-0 (last accessed 31.10.2019)