Pelvic Floor Anatomy: Difference between revisions
No edit summary |
No edit summary |
||
| Line 90: | Line 90: | ||
<br> | <br> | ||
'''Endopelvic Fascia - Ligaments''' | '''Endopelvic Fascia - Ligaments''' | ||
Female: Pubovesical ligaments - attach bladder to pubic symphysis <br> | Female: Pubovesical ligaments - attach bladder to pubic symphysis <br> | ||
| Line 96: | Line 96: | ||
Male: Puboprostatic ligaments - attach bladder to pubic symphysis <br> | Male: Puboprostatic ligaments - attach bladder to pubic symphysis <br> | ||
Sacrogenital - these are thickenings of the fascia, not specific ligaments<br> | Sacrogenital - these are thickenings of the fascia, not specific ligaments<br> | ||
Uterosacral ligaments - attach upper vagina, upper portion of cervix and uterus to the 3rd sacral vertebra | Uterosacral ligaments - attach upper vagina, upper portion of cervix and uterus to the 3rd sacral vertebra | ||
| Line 334: | Line 334: | ||
|} | |} | ||
== References == | == Use ful Resources == | ||
<div>Anatomy TV</div><div></div> | |||
== <span> </span>References == | |||
<references /> | <references /> | ||
[[Category:Articles]] [[Category:Anatomy]] [[Category:Mens_Health]] [[Category:Womens_Health]] [[Category:Videos]] | [[Category:Articles]] [[Category:Anatomy]] [[Category:Mens_Health]] [[Category:Womens_Health]] [[Category:Videos]] | ||
Revision as of 15:25, 21 April 2014
Original Editor - Laura Ritchie
Top Contributors - Laura Ritchie, Venus Pagare, Admin, Kim Jackson, Redisha Jakibanjar, Deborah Mazzarotto, Siobhán Cullen, Uchechukwu Chukwuemeka, Evan Thomas, Scott Buxton, George Prudden, Tarina van der Stockt, Mandy Roscher and Khloud Shreif
The Pelvic Floor - Overview and Function [1][edit | edit source]
The pelvic floor is an area of muscle and connective tissue that spans the area underneath the pelvis, separating the pelvic cavity above from the perineal region below. It provides support to the pelvic viscera including the bladder, intestines and uterus (in females). It also assists with continence through control of the urinary and anal sphincters. It facilitates birth by resisting the descent of the presenting part, causing the fetus to rotate forwards to navigate through the pelvic girdle. Finally, it helps to maintain optimal intra-abdominal pressure.
Osteology, Ligaments and Fascia
[edit | edit source]
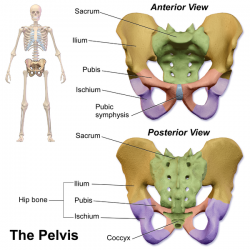
Osteology
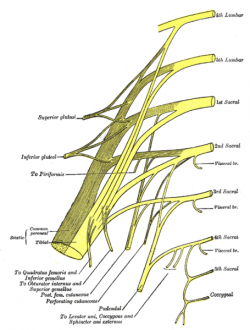
- The bony pelvis is composed of sacrum, ileum, ischium, and pubis.
- It is divided into the false (greater) and true (lesser) pelvis by the pelvic brim.
- The sacral promontory, the anterior ala of the sacrum, the arcuate line of the ilium, the pectineal line of the pubis and the pubic crest that culminates in the symphsis pubis.
- The shape of the female bony pelvis can be classified into four broad categories: gynecoid, anthropoid, android, and platypelloid.
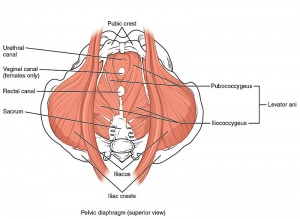
The Pelvic Diaphragms
- The pelvic diaphragm is a wide but thin muscular layer of tissue that forms the inferior border of the abdominopelvic cavity.
- Composed of a broad, funnel-shaped sling of fascia and muscle, it extends from the symphysis pubis to the coccyx and from one lateral sidewall to the other.
- The urogenital diaphragm, also called the triangular ligament, is a strong, muscular membrane that occupies the area between the symphysis pubis and ischial tuberosities and stretches across the triangular anterior portion of the pelvic outlet.
- The urogenital diaphragm is external and inferior to the pelvic diaphragm.
Ligaments and Pelvic Fascia[2]
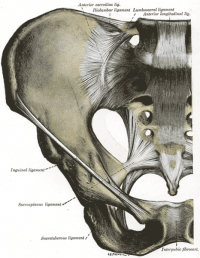
Ligaments of the Pelvis
Iliolumbar ligament - from tip of transverse process of L5 to posterior aspect of inner lip of iliac crest; strengthens the lumbo-sacral joint.
Lateral lumbosacral ligament
Sacrotuberous ligament- from sacrum to tuberosity of the ischium
Sacrospinous ligament - from ischial spine to lateral margins of the sacrum
Sacroiliac Ligaments
Ventral/Anterior sacroiliac ligament- from antero-lateral aspect of sacrum to auricular surface of the ilium
Dorsal/Posterior sacroiliac ligament
- Upper portion (short posterior sacroiliac ligament) - from 1st and 2nd transverse tubercles of sacrum to tuberosity of ilium
- Lower portion (long posterior sacroiliac ligament) - from 3rd transverse tubercle of sacrum to posterior superior iliac spine (PSIS)
Interosseous sacroiliac ligament- lies deep to posterior SI ligament and runs between the tuberosities of the sacrum and ilium
Sacrococcygeal Ligaments
Ventral/Anterio sacrococcygeal ligament -from anterior surface of sacrum to the front of the coccyx; continuation of the anterior longitudinal ligament of the spine
Dorsal sacrococcygeal ligament
- Deep portion - from inside sacral canal at the 5th sacral segment to the dorsal surface of the coccyx; continuation of the psoterior longitudinal ligament of the spine
- Superficial portion - from free margin of sacral hiatus to dorsal surface of the coccyx; corresponds with the ligamentum flavum of the spine
Lateral sacrococcygeal ligament - from inferior lateral angle of the sacrum to the transverse process of the 1st coccygeal vertebra
Pubic Symphysis Ligaments
Superior pubic ligament - runs between pubic tubercles
Inferior pubic ligament (aka arcuate public ligament) - runs between inferior pubic rami and blends with fibrocartilagnous disc of pubic symphysis
Anterior pubic ligament
Posterior pubic ligament - membranous structure which blends with periosteum
Endopelvic Fascia - Ligaments
Female: Pubovesical ligaments - attach bladder to pubic symphysis
Male: Puboprostatic ligaments - attach bladder to pubic symphysis
Sacrogenital - these are thickenings of the fascia, not specific ligaments
Uterosacral ligaments - attach upper vagina, upper portion of cervix and uterus to the 3rd sacral vertebra
Cardinal ligaments (aka Mackenrodt's) - attach upper vagina, cervix and uterus to the side walls of the pelvis
Round ligaments - attach uterus to mons pubis
Broad ligaments - attach uterus to medial aspect of the ilium
Uracus ligament - attaches bladder to umbilicus (formed from the remnants of the umbilican vein)
Penile Suspensory Ligaments
Penile Suspensory ligament - attaches to anterior aspect of interpubic disc and divides in two to sling around the penis
Fundiform ligament - extends from inferior linea alba and divides to wrap around the penis
Parietal pelvic fascia - lines the internal surface of the muscles of the pelvic floor and walls
Visceral pelvic fascia - invests each pelvic organ
The parietal and visceral fascia are continuous where organs penetrate the pelvic floor. They thicken to form the arcus tendineus, arches of fascia running adjacent to the viscera from the pubis to the sacrum.
Endopelvic fascia* - meshwork of smooth muscle, ligaments, blood vessels and connective tissue lying between the parietal and visceral fascia, sometimes condensing to form fibrous fascial septa which separate and suspend the organs.
- Anatomists use the name subserous fascia whereas surgeons refer to this layer of retroperitoneal fascia as endopelvic fascia.
- Hypogastric sheath - separates retropubic space from presacral space; conduit for vessels and nerves
- Transverse cerical (cardinal) ligaments - part of hypogastric sheath; runs from lateral pelvic wall to uterine cervix and vagina; transmits uterine artery and provides passive support for the uterus
- Vesicovaginal septum
- Rectovesical septum
- Rectovaginal septum
Pelvic Floor Myology [2][1][edit | edit source]
Layer One - Urogenital Triangle
- Bulbocavernosus (bulbospongiosus in men)
- Ischiocavernosus
- Superficial transverse perineal
- External anal sphincter
Layer Two - Urogenital Diaphragm
- Urethral sphincter (sphincter urethrae)
- Compressor urethrae
- Sphincter urethral vaginalis
- Deep transverse perineal
- Perineal membrane
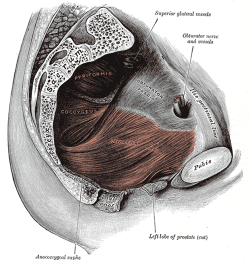
Layer Three - Pelvic Diaphragm
- Levator ani (pubococcygeus aka pubovisceral, pubovaginalis, puboanalis, puborectalis, iliococcygeus)
- Ischiococcygeus (Coccygeus)
- Piriformis
- Obturator internus
- Arcus tendinous of levator ani
- Arcus tendinous fasciae pelvis
Perineal Body - a fibromuscular structure located between the vagina/testicles and the anus, attaching to the sides of the ischiopubis rami by the deep transverse perineal muscle. It is know as the central tendon of the pelvis because many pelvic floor structures intersect with the perineum at this structure.
Other muscles related to pelvic dysfunction
Psoas
Rectus abdominus
Transversus abdominus
| [3] | [4] |
| Muscle | Origin | Insertion | Action | Innervation |
| Bulbospongiosus |
Male: median raphe, ventral surface of bulb of penis Female: perineal body then divides to wrap around vagina |
Male: Corpora spongiosum and cavernosa, fascia of bulb of penis Female: fascia of corpus cavernosa |
Male: Empties urethra, acts as sphincter to compress bulb of penis, assists erection, propels semen down urethra Female: empties urethra, acts as a sphincter to reduce lumen of vagina and assists erection of clitoris |
Deep branch of perineal nerve (branch of pudendal nerve) |
| Ischiocavernosus | Ischial ramus and tuberosity | Crus of penis or clitoris | Maintains erection of penis or clitoris by compression of outflow veins | Deep branch of perineal nerve (branch of pudendal nerve) |
| Superficial transverse perineal | Ischial tuberosity | Perineal body | Reinforces action of deep transverse perineal muscle to stabilize perineal body | Deep branch of perineal nerve (branch of pudendal nerve) |
| External anal sphincter | Perineal body and encircles anal canal |
Coccyx | Part of voluntary sphincter of anal canal | Inferior rectal (anal) nerve |
| Sphincter urethrae | Inferior aspect of pubic ramus and ischial tuberosity | Surrounds urethra; in females, some fibres also enclose the vagina | Controls flow of urine through urethra; also compresses vagina in females | Deep branch of perineal nerve (branch of pudendal nerve) |
|
Compressor urethrae (only in females) |
Ischiopubic ramus |
Vaginal wall |
Compresses ventral wall of the urethra |
|
|
Sphincter urethral vaginalis (only in females) |
Vaginal walls |
Ventral surface of urethra |
Compresses ventral wall of the urethra |
|
| Deep transverse perineal | Inner aspect of ischiopubic ramus | Median raphe (male), perineal body and external anal sphincter | Fixes perineal body, supports the function of levator ani and sphincter urethra |
Deep branch of perineal nerve (branch of pudendal nerve) |
| Perineal membrane (fascial thickening, not a muscle) | Fasical attachments at pubic symphysis | Fascial attachments at ischial spine | Suspensory ligament that provides extra support to prevent descent of perineal body |
|
| Levator Ani (Pubococcygeus) | Dorsal surface of pubis and fascia of obturator internus |
Anococcygeal body between tip of coccyx and the anal canal |
Voluntary spincter of the anal canal |
Nerve to levator ani (branches of S4), inferior rectal nerve (from pudendal nerve - S3, S4), coccygeal plexus |
| Levator Ani (Puborectalis) | Dorsal surface of pubis and fascia of obturator internus | Unites with its partner to make a U-shaped sling around the rectum | Controls defecation by pulling anorectal junction forward | Nerve to levator ani (branches of S4), branch of pudendal nerve (S2-4) |
| Levator Ani (Pubovaginalis) | Nerve to levator ani (branches of S4), branch of pudendal nerve (S2-4) | |||
| Levator Ani (Iliococcygeus) | Posterior aspect of arcus tendineus levator ani and the ischial spine | Anococcygeal body and the coccyx | Helps to support pelvic viscera and lateral coccyx | Nerve to levator ani (branches of S4), inferior rectal nerve (from pudendal nerve - S3, S4), coccygeal plexus |
|
Ischiococcygeus* (Coccygeus) *some consider this more of a ligament than a muscle |
Ischial Spine | Lower two sacral and upper two coccygeal spinal segments, blends with sacrospinous ligament on its external surface | Supports pelvic viscera, flexion of coccyx, stabilizes sacro-iliac joint | Anterior rami of S4 and S5 |
| Piriformis | Pelvic surface of sacrum, passes through greater sciatic foramen |
Superior border of the greater trochanter of the femur |
Hip external rotation, assist with hip abduction if hip is flexed |
Anterior rami of S1 & S2 |
| Obturator Internus | Internal or pelvic surface of the obturator foramen |
Medial surface of the greater trochanter of the femur |
Hip external rotation, assists with hip abduction if hip is flexed |
Nerve to obturator internus (L5, S1, S2) |
| Arcus tendinous levator ani (fascial thickening, not a muscle) | Fasical attachments at pubic symphysis | Fascial attachments at ischial spine | Suspensory ligament that provides extra support to prevent descent of perineal body | |
| Arcus tendinous fasciae pelvis (fascial thickening, not a muscle) | Fasical attachments at pubic symphysis | Fascial attachments at ischial spine | Suspensory ligament that provides extra support to prevent descent of perineal body |
Use ful Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 Wikipedia. Pelvic floor. http://en.wikipedia.org/wiki/Pelvic_floor. (accessed 6 April 2014).
- ↑ 2.0 2.1 Netter Anatomy. Pelvis and perineum: pelvic floor and contents. http://www.netteranatomy.com/anatomylab/subregions.cfm?subregionID=R53. (accessed 6 April 2014).
- ↑ Anatomy Zone. Pelvic Floor Part 1 - The Pelvic Diaphragm - 3D Anatomy Tutorial. Available from: http://www.youtube.com/watch?v=P3BBAMWm2Eo [last accessed 11/04/14]
- ↑ Anatomy Zone. Pelvic Floor Part 2 - Perineal Membrane and Deep Perineal Pouch - 3D Anatomy Tutorial. Available from: http://www.youtube.com/watch?v=q0Ax3rLFc6M[last accessed 11/04/14]