Osteoporotic Vertebral Fractures
Top Contributors - Mathieu Vanderroost, Angeliki Chorti, Lucinda hampton, Jasper Vermeersch, Jon Room, Kim Jackson, Jelle Van Hemelryck, Khloud Shreif, Laura Ritchie, Vidya Acharya, Lauren Lopez, Kai A. Sigel, WikiSysop, Claire Knott, 127.0.0.1, Admin and Rachael Lowe
Definition / Description[edit | edit source]
Osteoporotic (fragility) fractures are fractures that result from mechanical forces that would not ordinarily result in a fracture according to National Institute for Health and Care Excellence (NICE) clinical guidelines[1].
Vertebral compression fractures (VCFs) of the spinal column:
- Occur secondary to an axial/compressive (and to a lesser extent, flexion) load with a resultant biomechanical failure of the bone resulting in a fracture.
- Compromise the anterior column of the spine, thereby resulting in compromise to the anterior half of the vertebral body (VB) and the anterior longitudinal ligament (ALL).
- Do not involve the posterior half of the VB and do not involve the posterior osseous ligamentous complex. The former distinguishes a compression fracture from a burst fracture.
- Usually considered stable and do not require surgical instrumentation.[2]
Clinically Relevant Anatomy[edit | edit source]
Due to the osteoporosis that made the bone density low and made the bone weak (higher activity of osteoclasts and lower activity of osteoblasts), the vertebra can ‘collapse’. This is called a vertebral body fracture. The fracture can lead to hyperkyphosis or hyperlordosis depending on the vertebral level. People with osteoporosis break down bone faster than it can regenerate. Trabecular bone is more active and because of this, trabecular bone is more likely to be affected. When people stand up causing pressure on the spine, the weak trabecular bone of the spine body’s can start to collapse, leading to an osteoporotic vertebral fracture. This fracture occur on the posterior part of the vertebra or the vertebral body. Because of the decrease of height of the vertebra, the anterior longitudinal ligament and posterior longitudinal ligament lose tension. This can cause vertebral instability.
Etiology[edit | edit source]
- The most common etiology of VCFs is osteoporosis, making these fractures the most common fragility fracture.
- Compression fractures demonstrate a bimodal distribution with younger patients sustaining these injuries secondary to high energy mechanisms (fall from a height, MVA, etc.).
- Compression fractures by definition only involve compromise to the anterior column alone.
- VCFs are considered "stable" fracture patterns.
Epidemiology[edit | edit source]
Population studies have shown that the annual incidence of VCFs is 10.7 per 1000 women and 5.7 per 1000 men.
- VCFs are the most common fragility fracture reported in the literature.
- Approximately 1 to 1.5million VCFs occur annually in the united states (US) alone.
- Estimated that 40% to 50% of patients over age 80 years have sustained a VCF either acutely, or recognized incidentally during clinical workup for a separate condition.
- Thoracolumbar junction (i.e., the segment from T12 to L2) location most often affected (60% to 75% of VCFs), and another 30% occur at the L2 to L5 region
In younger patients
- 50% of spine fractures are due to motor vehicle collisions , 25% due to falls.
In the elderly patients
- 30% of VCFs occurring while the patient is in bed
- As the population continues to age, the population at risk of sustaining low energy fragility fractures will continue to increase as well.
- Largely unreported and are probably more common radiographically (present up to 14% of women older than 60 years in one study)[4]
- Currently, 10 million Americans are already diagnosed with osteoporosis, and another 34 million have osteopenia.
The below short video gives a brief overview of compression fractures
Clinical Presentation[edit | edit source]
Vertebral fractures present with pain and loss of mobility.[4]
Symptoms of vertebral fracture can include
- Back pain is common in elderly patients. Decrease when lying on the back. [6][7].
- Three quarters of patients with vertebral fractures do not seek medical attention and up to 70% of vertebral fractures may not result in notably severe symptoms [8].
Loss of height and acute pain. Height loss of the osteoporotic fractured vertebra may be mild (20-25%), moderate (25-40%) or severe (> 40%). It commonly affects the thoracolumbar region, though any vertebra may be disturbed. - The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture.
- The pain resolves over a period of six to 12 weeks.
- Chronic pain may also occur in patients with multiple compression fractures, height loss and low bone density (also due to structural changes or osteoarthritis).
- Radiographic VCF may not be symptomatic. The greater the deformity, the greater the likelihood of pain and disability.
- As height is lost, patients experience discomfort from the rib cage pressing downward on the pelvis.
- Patients develop an exaggerated thoracic kyphosis and/or an exaggerated lumbar lordosis[8]which may result in decreased exercise tolerance and reduced abdominal space giving rise to early satiety and weight loss.
- Sleep disorders may occur and decreased self esteem +/- depression.
- Self care may become difficult. [9][10][11].
- Associated with an increased morbidity and increased mortality[8][12]
Risk factors[edit | edit source]
Vertebral fractures aren’t only due to osteoporosis. It’s possible that atraumatic vertebral compression fracture is caused due to[13]:
● Osteomalacia/ Rickets: softening of the bones due to a Vitamin D deficiency in adults. In time it can result in decalcification of the bone, fractures, skeletal deformities, bone pain and muscle weakness. Rickets is a similar condition in children.
● Paget's Disease: Bone is resorbed and formed at an increased rate, which may lead to pain, fractures, deformity, headaches, dizziness, osteoarthritis, spinal stenosis, and increased size of clavicle are a few common presentation.
● Bone Infection
● Pediatric osteogenesis imperfecta
● Cancer: Low-energy fractures may also be result of bone cancer or metastatic cancer.
● Multiple Myeloma
● Renal osteodystrophy
● Scurvy (Vitamin C deficiency) and Vitamin D deficiency
Diagnostic Procedures[edit | edit source]
Diagnosed on Xrays when there is a loss of height in the anterior, middle, or posterior dimension of the vertebral body that exceeds 20%.
Osteoporotic spine fractures can be graded based on vertebral height loss as:
- mild: up to 20-25%
- moderate: 25-40%
- severe: >40%
Chronicity of the fracture indicates its temporal relationship with symptoms and hence is an important determination.
On conventional imaging, acute fracture signs include cortical breaking or impaction of trabeculae; in the absence of these signs fractures are chronic.
In uncertain cases, MRI signs of oedema (acute) and presence of radiotracer uptake on bone scintigraphy (acute) help decide the age of the fracture.
Outcome Measures[edit | edit source]
- Visual analogue scale for overall pain (VAS).
- Quality of Life questionnaire: this can be measured with the use of the Quality of Life Questionnaire of the European Foundation for Osteoporosis (QUALEFFO). An other possibility is to use the Assessment of Quality of Life (AQoL) questionnaire or the European Quality of Life–5 Dimensions (EQ–5D) scale.
- Physical functioning: measured by a modified 23-item version of the Roland–Morris Disability Questionnaire.
- Pain at night and at rest (VAS score)[14]
Examination[edit | edit source]
Clinical assessment of vertebral fractures is generally poor and reliance is made on imaging studies for diagnosis[10].
2 tests that help the practitioner to predict more accurately which patients have an acute vertebral fracture[15].
- Closed-fist percussion sign[15]
This test has a sensitivity of 87,5% and a specificity of 90%, which is good. Stand behind the patiënt and the patiënt stand in front of a mirror allowing you to see the reaction of the patiënt. Firm closed-fist percussion is used to examine the entire length of the spine. The clinical sign is positive when the patiënt complains of a sharp, sudden pain.
2. The supine sign[15]
This test has a sensitivity of 81,25% and a specificity of 93,33%, which is also pretty good. The patiënt is asked to lie supine with only one pillow for the head. The clinical sign is positive when the patiënt is unable to lie supine due to severe pain.
Medical Management[edit | edit source]
Good quality evidence supports that several medications (e.g. bisphosphonates) for bone density reduce fracture risk. Nevertheless side effects vary among drugs. (Crandall CJ, 2014: LoE 1A) [16].
At first, conservative treatment still is the method of choice. In case of resulting deformity and persistent pain vertebral cement augmentation techniques today are widely used. Treatment after vertebral fracture should include appropriate pain management and possibly bracing[17]. Forms of conservative treatment commonly used in these patients include bed rest, analgesic medication, physiotherapy and bracing.
Pain management
Frequently used analgesia are paracetamol or salicylates and non-steroidal anti-inflammatory drugs (NSAIDs). The risk of gastrointestinal bleeding and insufficiency should be taken into account when prescribing NSAIDs[18]. There is only low or very low-quality evidence on the efficacy of non-surgical treatment of symptoms of acute osteoporotic VCFs. Immediate- and short-term effects of opioids on pain were found inconsistent across trials with different comparators. Low-quality evidence supports the immediate- and short-term effects of an NSAID on reducing pain intensity.
Spinal orthoses
The primary goal of bracing is to reduce pain by stabilising the spine and limiting progression of the deformity. A spinal orthosis should reduce gross spinal movement and segmental movement at the injured segment, reduction in the period of bed rest, facilitate earlier mobilization[19]
An ideal brace should be light-weight and easy to put on. It should be comfortable to obtain patient compliance and it has to avoid respiratory impairments. Examples of braces are the Jewett brace, Taylor brace and cruciform anterior spinal hyperextension (CASH) orthosis, they keep the spine in hyperextension. Even though bracing is widely used in these patients, its use is still opinion-based. Important: the evidence for a conservative spinal orthosis in patients with osteoporotic vertebral fractures is based on evidence from studies in patients with non-osteoporotic vertebral burst fractures[18].
There is low-quality evidence indicating the value of spinal orthoses for pain relief and disability at medium term. At present, there is insufficient evidence to inform conservative care for acute pain related to VCF. This was concluded by Rzewuska M. and colleagues after a 2015 systematic review with meta-analysis[17].
We could only find one study evaluating spinal orthoses in the treatment of osteoporotic VCFs. Pfeifer, Begerow and Minne[20] performed a prospective randomised trial using a thoracolumbar orthosis (TLO) to manage VCFs in women with postmenopausal osteoporosis. They reported increased trunk muscle strength and improvement of posture and body height in patients treated with an orthosis. They noted that patients had less pain, a better quality of life and restoration of their ability to perform daily living tasks.
Vertebral fractures can also be treated surgically using vertebroplasty and kyphoplasty[16][18]:
- Percutaneous vertebroplasty (VP) began as a simple, low-cost procedure that aimed to provide pain relief for patients with vertebral compression fractures (VCF).In which, usually polymethylmethacrylate (PMMA), is injected into the vertebral bone
- Balloon Kyphoplasty (KP) was introduced later, and was presented not only as a ‘‘pain killer,’’ but also as a deformity correction procedure[18].Where a balloon is inserted into the vertebral body, the balloon is inflated to attempt to re-establish normal height and posture, the balloon is removed and cement injected. It permits kyphosis correction if performed within 3 months post-fracture. Height restoration is not a perquisite for pain control[7].
The video clip below tells of an elderly lady with an osteoporotic insufficiency fracture and an animated version of a vertebroplasty.
Indications for surgery are: failed medical treatment for pain control, patients with co-morbidities that make prolonged bed rest dangerous, patients with fractures that fail to heal, resulting deformity, an unstable fracture (pattern) and involvement of spinal cord[22]. This was proved in both retrospective and prospective studies as well as in meta-analysis[6][20][23]. The procedures are proved to be cost effective[24].
Buchbinder R. et al (2009) performed a randomized controlled trial in which they compared a vertebroplasty surgery with a sham treatment in patients who suffer from an osteoporotic vertebral fracture. There were significant improvements at all follow-up measurements for several outcome measures: overall pain, pain at night, pain at rest, physical functioning and quality of life. They concluded that there is no beneficial effect of vertebroplasty as compared with a sham procedure in patients with painful osteoporotic vertebral fractures[24]. This has been confirmed by a Cochrane review[6].
Diamond TH. et al (2003) compared a conservative and percutaneous vertebroplasty treatment for patients with an osteoporotic vertebral fracture. As outcome measures they used physical functioning and pain scores. They concluded that the operatively treated group scored significantly higher on the outcome measures than the conservatively treated group. This was the case for the short-term as well as the long-term measurements[17].
Alvarez L. et al.[18] compared a conservative and operative treatment (percutaneous vertebroplasty). Similar to the results of Diamond TH. et al[17], they found that treatment with percutaneous vertebroplasty gives a rapid and significant relief of pain and improvement in quality of life.
Anderson, Froyshteter and Tontz[24] conducted a meta-analysis on vertebral augmentation (kyphoplasty). They compared vertebral augmentation with conservative treatment for osteoporotic spinal fractures. The meta-analysis showed greater pain relief, functional recovery and helath-related quality of life with cement augmentation compared with controls. Cement augmentation results were significant in the early (<12 weeks) and the late time points (six to 12 months). This meta-analysis provides strong evidence in favor of cement agmentation in the treatment of sympotmatic VCF fractures.
Chang X et al (2015) compared vertebroplasty to kyphoplasty in a meta-analysis of prospective comparative studies. They concluded that percutaneous vertebroplasty takes less time in the operation, has a greater risk of cement leakage, was inferior in reducing cobb angle in the long term and results in lower anterior vertebral body height after surgery. For pain relief (main desire of patients) both procedures still remain effective[12].
Low bone mineral densitiy, presence of multiple treated vertebrae and a history of steroid usage were associated with new VCFs after vertebroplasty according to a meta-analysis from Cao J et al. (2016). Patients with these factors should be informed of the potential increased risk[7].
Song D and colleagues (2015) found no differences in the incidence of secondary fractures between vertebral augmentation techniques and conservative treatment for patients with osteoporotic vertebral compression fractures. They conducted a systematic review and meta-analysis of randomized controlled trials and prospective non-randomized controlled trials[16].
Physical Therapy Management[edit | edit source]
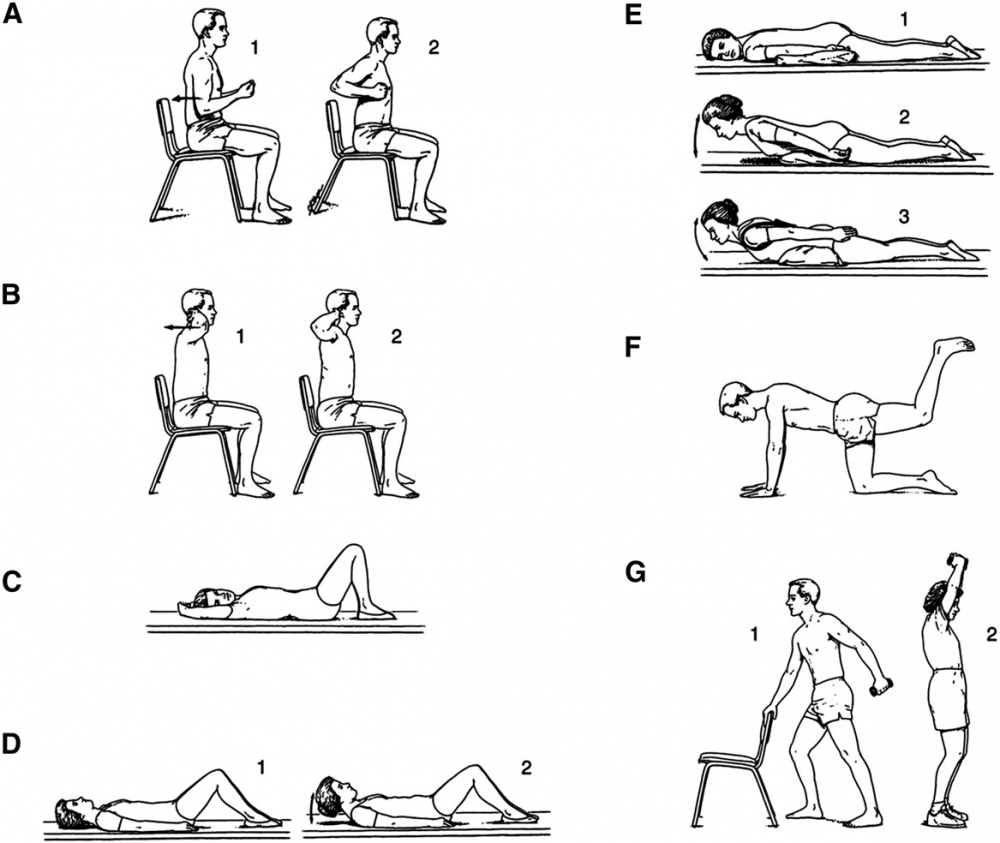
After a short period of bed rest patients should begin mobilisation with a rehabilitation and exercise program. The goals of rehabilitation are the prevention of falls, reduction of the Thoracic Hyperkyphosis, enhancing axial muscle strength and providing correct spine alignment[25].
Regarding Physiotherapy management, there are a number of treatment approaches, including strengthening exercise, stabilisation exercise, balance training, stretching, relaxation techniques, manual therapy and taping[26][27]. Currently, a large RCT is comparing exercise based and ‘hands on’ manual therapy based physiotherapy against a control[27].
Zehnacker and Bemis‐Dougherty conducted a systematic review to study the effect of weighted exercises on bone mineral density in post menopausal women[28]. Exercises such as walking has been shown to maintain or improve bone density in an osteoporotic population. Strengthening exercises, using weights or resistance bands, has also been shown to maintain or improve bone density at the location of the targeted muscle attachments[29]. Maintaining bone health is extremely important, especially in the elderly as there typically is a decline in bone mass with age.
Strengthening and flexability exercises improve overall physical function and postural control. Improving postural control is important to reduce risk for falls. Falls often result in fractures in an osteoporotic population. Balance exercises are also important to further reduce the risk of falls[30].
Studies from De Kam et al. (2009, LoE:1A), Karinkanta et al. (2007, LoE:1B) and Hourigan SR et al. (2008, LoE:1B) all found that a combined balance and progressive strength training programme produced the best results in terms of maintaining leg strength, balance, bone mineral density and physical function compared to balance or strength training alone[31][32][33].
Sinaki et al demonstrated that a spinal extensor strengthening programme and a dynamic proprioceptive programme increased bone density and reduced the risk of VCFs. Moreover the incidence of new fractures associated with back extension exercises is lower than the incidence related to abdominal flexion exercises (16% versus 89%)[34].
Exercise and exercise technique that focuses on spinal extension play an important role in reducing the risk of osteoporosis-related fractures. In addition, reports have shown that strenuous spinal flexion exercise, whether therapeutic, recreational, or job related, may induce compression fracture if beyond the biomechanical competence of the vertebral bodies. In other words, extreme flexion is contra-indicated[35].
Back extensor exercises improve muscle strength, providing a better dynamic-static posture and reduction of the kyphotic deformity. Correction of the kyphosis also results in pain relief, increased mobility and an improvement in the quality of life[36].
It has been previously hypothesized that horizontal nonloading back extension exercises from a prone position can decrease the incidence of vertebral fractures[37]. Back extension exercises performed from the prone position load vertebral horizontal trabeculae without the risk of vertebral compression fracture that can occur with vertical loading[35].
For some individuals with frequent falling with or without VCF, we'll find them suffer from fear avoidance so it will be a good choice to start exercises; strengthening, weight bearing with aqua therapy it's an effective intervention to decrease the risk of falling, improve gait pattern and balance[38]
Chen BL and colleagues studied the effectiveness of systematic back muscle exercises after vertebroplasty for spinal osteoporotic compression fractures. They found that systematic back muscle exercises resulted in a significant better outcome on the Oswestry Disability Index and pain level (VAS) compared to the control group. Control group only received general postoperation therapy without systematic back exercises[39].
Wendlova J. concluded that after a biomechanical analysis that carrying a backpack on the back is recommended to patients with osteoporotic vertebral fractures. This is based upon removing the muscular dysbalance of the trunk muscles and upon increasing the bone strength by compressive force acting upon the vertebrae. Compressive forces activate osteoblasts to enhance osteoformation.The backpack load is differentiated: patients with vertebral fractures put a weight up to 1 kg into their backpacks, patients without vertebral fractures but diagnosed with osteoporosis increase the load up to 2kg. Further research is needed[40].
To prevent falls and fractures, an exercise program should include balance and lower extremity strength training combined with a coordinated approach[35].
Postural taping can help in maintaining postural alignment. Tape is applied to the skin to provide increased proprioceptive feedback about postural alignment, improve thoracic extension, reduce pain and facilitate postural muscle activity and balance[41]. For example;
Clinical Bottom Line[edit | edit source]
Osteoporotic vertebral fractures are fractures of one or more of the vertebrae due to osteoporosis. Osteoporosis causes the bones to be more fragile and more likely to fracture. Osteoporotic vertebral fractures classically occur during normal day-to-day activities such as bending, twisting, walking or lifting relatively light objects.
The pain of acute fracture usually lasts 4 to 6 weeks with intense pain at the site of fracture. Chronic pain may also occur in patients with multiple compression fractures, height loss and low bone density. Although this is probably due to structural changes or osteoarthritis.
Vertebral fractures don't only occur due to osteoporosis. Also a trauma or metastasis can cause a vertebral fracture. The diagnosis of osteoporosis can be confirmed by Dual Energy X-ray Absorptiometry (DXA).
Often used outcome measures to evaluate the progression of a patient are: Visual analogue scale for overall pain and pain during day and night (VAS), a Quality of Life questionnaire and a Physical functioning questionaire ( modified 23-item version of the Roland–Morris Disability Questionnaire).
Conservative treatment (bed rest, analgesic medication, physiotherapy and bracing) still is the method of choice as medical treatment. Vertebral fractures can also be treated surgically using vertebroplasty and kyphoplasty.
As physical therapy management there are a number of treatment approaches, including strengthening exercise, stabilisation exercise, balance training, stretching, relaxation techniques, manual therapy and taping.
Key Research[edit | edit source]
The following articles are key evidence pieces for physical therapy interventions:
- Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials[23]
- A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial [20]
- Positive effects of exercise on falls and fracture risk in osteopenic women[24]
- Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study
- Identifying osteoporotic vertebral fracture[22]
- Position Statement of the Korean Society for Bone and Mineral Research[22]
Resources[edit | edit source]
www.nhs.uk/conditions/Osteoporosis/Pages/Introduction.aspx
www.nos.org.uk/about-osteoporosis
References[edit | edit source]
- ↑ Yoo JH, Moon SH, Ha YC, Lee DY, Gong HS, Park SY, Yang KH.Osteoporotic Fracture: 2015 Position Statement of the Korean Society for Bone and Mineral Research.J Bone Metab. 2015 Nov;22(4):175-81. 30. Level of Evidence: 2B.
- ↑ Donnally, Chester & Varacallo, Matthew. (2018). Fracture, Compression. Available from:https://www.researchgate.net/publication/329717392_Fracture_Compression (last accessed 22.4.2020)
- ↑ Spine live. Spinal compression fractures reasons. Available from: https://www.youtube.com/watch?v=LILgFAEMAbg (last accessed 12.4.2019)
- ↑ 4.0 4.1 Radiopedia. Vertebral compression fractures. Available from:https://radiopaedia.org/articles/osteoporotic-spinal-compression-fracture
- ↑ Pain doctor Nevada. Spinal compression fracture. Available from: https://www.youtube.com/watch?v=dLiOQfr4e_A&t=20s (last accessed 12.4.2019)
- ↑ 6.0 6.1 6.2 Buchbinder R, Golmohammadi K, Johnston RV, Owen RJ, Homik J, Jones A, Dhillon SS, Kallmes DF, Lambert RG.Percutaneous vertebroplasty for osteoporotic vertebral compression fracture.Cochrane Database Syst Rev. 2015 Apr 30;4:CD006349. Level of Evidence: 1A.
- ↑ 7.0 7.1 7.2 NOF. Osteoporosis and your spine. National Osteoporosis Foundation. http://nof.org/articles/18 (accessed 03/02/15.
- ↑ 8.0 8.1 8.2 Griffith JF. Identifying osteoporotic vertebral fracture. Quant Imaging Med Surg. 2015 Aug;5(4):592-602. (Level of Evidence: 2C)
- ↑ El-Fiki M. Vertebroplasty, Kyphoplasty, Lordoplasty, expandable devices and current treatment of painful osteoporoticvertebral fractures.World Neurosurg. 2016 Apr 9
- ↑ 10.0 10.1 Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Conservative management of patients with an osteoporotic vertebral fracture: a review of the literature. J Bone Joint Surg Br. 2012 Feb;94(2):152-7. (Level of Evidence: 2A)
- ↑ Silverman SL. The Clinical Consequences of Vertebral Compression Fracture. Bone 13, S27-S31. 1992. (Level of Evidence: 3B)
- ↑ 12.0 12.1 Puisto V, Rissanen H, Heliövaara M, Impivaara O, Jalanko T, Kröger H, Knekt P, Aromaa A, Helenius I. Vertebral fracture and cause-specific mortality: a prospective population study of 3,210 men and 3,730 women with 30 years of follow-up. Eur Spine J 2011 20:2181–2186 DOI 10.1007/s00586-011-1852-0.
- ↑ Medscape. Osteoporosis Differential Diagnoses. http://emedicine.medscape.com/article/330598-differential (accessed 10 May 2016) (Level of Evidence: 5)
- ↑ Diamond TH. et al. Management of Acute Osteoporotic Vertebral Fractures: A Nonrandomized Trial Comparing Percutaneous Vertebroplasty with Conservative Therapy. Am J Med. 2003;114:257–265. (Level of Evidence: 2B)
- ↑ 15.0 15.1 15.2 James Langdon et al. Vertebral compression fractures - new clinical signs to aid diagnosis. Ann R Coll Surg Engl 2010; 92: 163–166 (Level of evidence: 2C)
- ↑ 16.0 16.1 16.2 Crandall CJ, Newberry SJ, Diamant A, Lim YW, Gellad WF, Booth MJ, Motala A, Shekelle PG.Comparative effectiveness of pharmacologic treatments to prevent fractures: an updated systematic review. Ann Intern Med. 2014 Nov 18;161(10):711-23. Level of Evidence: 1A.
- ↑ 17.0 17.1 17.2 17.3 Gerdhem P. Osteoporosis and fragility fractures: Vertebral fractures. Best Practice Research Clinical Rheumatology 2013 27: 743–755.
- ↑ 18.0 18.1 18.2 18.3 18.4 NICE. Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for treating osteoporotic vertebral compression fractures: NICE technology appraisal guidance TA279. Manchester: National Institute for Health and Care Excellence, 2013.
- ↑ Kim DH, Vaccaro AR. Osteoporotic compression fractures of the spine; current options and considerations for treatment.Spine J. 2006 Sep-Oct;6(5):479-87. Level of Evidence: 3A.
- ↑ 20.0 20.1 20.2 Gauthier A, Kanis JA, Jiang Y, Martin M, Compston JE, Borgström F, Cooper C, McCloskey EV. Epidemiological burden of postmenopausal osteoporosis in the UK from 2010 to 2021: estimations from a disease model. Arch Osteoporos 2011 6:179–188.
- ↑ Lee Health. Fixing a fractured spine. Available from: https://www.youtube.com/watch?v=QjvKkYehpUI (last accessed 12.4.2019)
- ↑ 22.0 22.1 22.2 NICE. Alendronate, etidronate, risedronate, raloxifene and strontium ranelate for the primary prevention of osteoporotic fragility fractures in postmenopausal women (amended): NICE technology appraisal guidance 160. Manchester: National Institute for Health and Care Excellence, 2011.
- ↑ 23.0 23.1 Liu JT et al. Balloon kyphoplasty versus vertebroplasty for treatment of osteoporotic vertebral compression fracture: a prospective, comparative, and randomized clinical study. Osteoporos Int. 2010 Feb;21(2):359-64. Level of Evidence: 1B.
- ↑ 24.0 24.1 24.2 24.3 Kim DH, Vaccaro AR. Contemporary Concepts in Spine Care: Osteoporotic compression fractures of the spine; current options and considerations for treatment. The Spine Journal. 2006 6 479–487.
- ↑ Yoo JH, Moon SH, Ha YC, Lee DY, Gong HS, Park SY, Yang KH.Osteoporotic Fracture: 2015 Position Statement of the Korean Society for Bone and Mineral Research.J Bone Metab. 2015 Nov;22(4):175-81. 30. (Level of Evidence: 2B)
- ↑ Pratelli E, Cinotti I, Pasquetti P. Rehabilitation in osteoporotic vertebral fractures. Clin Cases Miner Bone Metab. 2010 7(1): 45–47.
- ↑ 27.0 27.1 Barker K, Javaid MK, Newman M, Minns Lowe C, Stallard N, Campbell H, Gandhi V, Lamb S. Physiotherapy Rehabilitation for Osteoporotic Vertebral Fracture (PROVE): study protocol for a randomised controlled trial. Trials 2014 15:22
- ↑ Zehnacker CH, Bemis‐Dougherty A. Effect of Weighted Exercises on Bone Mineral Density in Post Menopausal Women A Systematic Review. Journal of Geriatric Physical Therapy. 2007; 30(2):79-88. (Level of Evidence: 1A)
- ↑ Hong AR, Kim SW. Effects of resistance exercise on bone health. Endocrinology and Metabolism. 2018 Dec 1;33(4):435-44.
- ↑ Burke TN, Franca FJR, Ferreira de Meneses SR, Pereira RMR, Marques AP. Postural control in elderly women with osteoporosis: comparison of balance, strengthening and stretching exercises. A randomized controlled trial. Clinical Rehabilitation; 26 (11): 1021-1031. 2012. (Level of Evidence: 1B)
- ↑ De Kam D, Smulders E, Weerdesteyn V, Smits-Engelsman BCM. Exercise interventions to reduce fall-related fractures and their risk factors in individuals with low bone density: a systematic review of randomized controlled trials. Osteoporos Int. 2009;20:2111–2125 (Level of evidence: 1A)
- ↑ Karinkanta S, Heinonen A, Sievänen H, Uusi-Rasi K, Pasanen M, Ojala K. A multi-component exercise regimen to prevent functional decline and bone fragility in home-dwelling elderly women: a randomized, controlled trial. Osteoporos Int. 2007;18:453–462. (Level of evidence: 1B)
- ↑ Hourigan SR, Nitz JC, Brauer SG, O'Neill S, Wong J, Richardson CA. Positive effects of exercise on falls and fracture risk in osteopenic women. Osteoporos Int. 2008;19:1077–1086. (Level of evidence: 1B)
- ↑ Sinaki M, Lynn SG. Reducing the risk of falls through proprioceptive dynamic posture training in osteoporotic women with kyphotic posturing: a randomized pilot study.Am J Phys Med Rehabil. 2002 Apr;81(4):241-6. (Level of Evidence: 3B)
- ↑ 35.0 35.1 35.2 Sinaki M. Exercise for patients with osteoporosis: management of vertebral compression fractures and trunk strengthening for fall prevention.PM R. 2012 Nov;4(11):882-8. (Level of Evidence: 3A)
- ↑ Itoi E, Sinaki M.Effect of back-strengthening exercise on posture in healthy women 49 to 65 years of age.Mayo Clin Proc. 1994 Nov;69(11):1054-9. (Level of Evidence: 3B)
- ↑ Sinaki M.The role of physical activity in bone health: a new hypothesis to reduce risk of vertebral fracture.Phys Med Rehabil Clin N Am. 2007 Aug;18(3):593-608, xi-xii. (Level of Evidence: 5)
- ↑ Kim SB, O’sullivan DM. Effects of aqua aerobic therapy exercise for older adults on muscular strength, agility and balance to prevent falling during gait. Journal of physical therapy science. 2013;25(8):923-7.
- ↑ Chen BL, Zhong Y, Huang YL, Zeng LW, Li YQ, Yang XX, Jiang Q, Wang CH. Systematic back muscle exercise after percutaneous vertebroplasty for spinal osteoporotic compression fracture patients: a randomized controlled trial.Clin Rehabil. 2012 Jun;26(6):483-92. (Level of Evidence: 1B)
- ↑ Wendlova J. The importance of carrying a backpack in the rehabilitation of osteoporotic patients (biomechanical analysis).Bratisl Lek Listy. 2011;112(1):41-3. (Level of Evidence: 4)
- ↑ Bautmans I, Van Arken J, Van Mackelenberg M, Mets T. Rehabilitation using manual mobilization for thoraic kyphosis in elderly postmenopauzal patients with osteoporosis. J Rehabil Med 2010, 42: 129-135. (Level of Evidence: 3B)
- ↑ John Gibbons. Try this Kinesiology Taping technique for poor posture - its incredible. Available from: http://www.youtube.com/watch?v=996cC3ovLEQ[last accessed 21/4/2020]