Osteoarthritis: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) No edit summary |
||
| (6 intermediate revisions by one other user not shown) | |||
| Line 4: | Line 4: | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
Osteoarthritis (OA), also known as degenerative joint disease (DJD), is the most common form of arthritis.<ref>Radiopedia Osteoarthritis Available:https://radiopaedia.org/articles/osteoarthritis (accessed 3.9.2022)</ref> It can be classified into two categories: primary osteoarthritis and secondary osteoarthritis. OA usuallly presents with joint pain and loss of function; however, the disease is clinically very variable and can present merely as an asymptomatic incidental finding to a devastating, permanently disabling disorder.<ref>Sen R, Hurley JA. Osteoarthritis. InStatPearls [Internet] 2021 Aug 19. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK482326/ (accessed 3.9.2022)</ref> | [[File:Osteoarthritis.png|right|frameless|399x399px]] | ||
Osteoarthritis (OA), also known as degenerative joint disease (DJD), is the most common form of [[arthritis]].<ref name=":1">Radiopedia Osteoarthritis Available:https://radiopaedia.org/articles/osteoarthritis (accessed 3.9.2022)</ref> It can be classified into two categories: primary osteoarthritis and secondary osteoarthritis. OA usuallly presents with joint pain and loss of function; however, the disease is clinically very variable and can present merely as an asymptomatic incidental finding to a devastating, permanently disabling disorder.<ref name=":2">Sen R, Hurley JA. Osteoarthritis. InStatPearls [Internet] 2021 Aug 19. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK482326/ (accessed 3.9.2022)</ref> | |||
The 4 and a 12 minute video below gives an overview of OA{{#ev:youtube|https://www.youtube.com/watch?v=41IMR_Dp5bs|width}}<ref>Nucleus medical media Osteoarthritis | Nucleus Health Available from: https://www.youtube.com/watch?v=41IMR_Dp5bs (last accessed 28.5.2019)</ref> | |||
The 4 and a 12 minute video below gives an overview of OA. Press youtube link.{{#ev:youtube|https://www.youtube.com/watch?v=41IMR_Dp5bs|width}}<ref>Nucleus medical media Osteoarthritis | Nucleus Health Available from: https://www.youtube.com/watch?v=41IMR_Dp5bs (last accessed 28.5.2019)</ref> | |||
== Pathophysiology == | == Pathophysiology == | ||
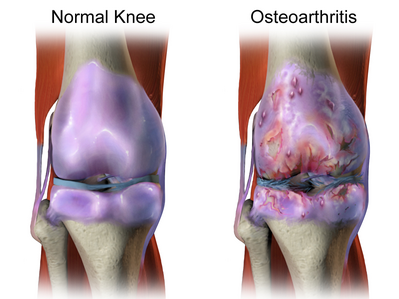
In normal joints hyaline cartilage covers the end of each bone. Hyaline cartilage provides a smooth, gliding surface for joint motion and acts as a cushion between the bones. In OA, the cartilage breaks down, causing pain, swelling and problems moving the joint. As OA worsens over time, bones may break down and develop growths called spurs. Bits of bone or cartilage may flake off and float around in the joint. In the body, an inflammatory process occurs and cytokines | [[File:Knee-OA1.png|thumb|463x463px|Knee OA]] | ||
In normal joints hyaline [[cartilage]] covers the end of each [[bone]]. Hyaline cartilage provides a smooth, gliding surface for joint motion and acts as a cushion between the bones. In OA, the cartilage breaks down, causing pain, swelling and problems moving the joint. As OA worsens over time, bones may break down and develop growths called spurs. Bits of bone or cartilage may flake off and float around in the joint. In the body, an [[Inflammation Acute and Chronic|inflammatory]] process occurs and [[cytokines]] and [[enzymes]] develop, furtherer damaging the cartilage. In the final stages of OA, the cartilage wears away and bone rubs against bone leading to joint damage and more pain.<ref>Arthritis foundation [https://www.arthritis.org/about-arthritis/types/osteoarthritis/what-is-osteoarthritis.php What is arthritis] Available from: https://www.arthritis.org/about-arthritis/types/osteoarthritis/what-is-osteoarthritis.php (last accessed 28.5.2019)</ref> | |||
Osteoarthritis: "A group of overlapping distinct diseases, which may have different etiologies but with similar biologic, morphologic, and clinical outcomes. The disease processes not only affect the [[Cartilage|articular cartilage]], but involve the entire joint, including the subchondral bone, ligaments, capsule, synovial membrane, and periarticular muscles. Ultimately, the articular cartilage degenerates with fibrillation, fissures, ulceration, and full thickness loss of the joint surface." <ref>Kuttner K, Goldberg VM. Osteoarthritis disorders Rosemout. InAmerican Academy of, Orthopedic Surgeons 1995 (pp. 21-25).</ref> | |||
== Epidemiology == | == Epidemiology == | ||
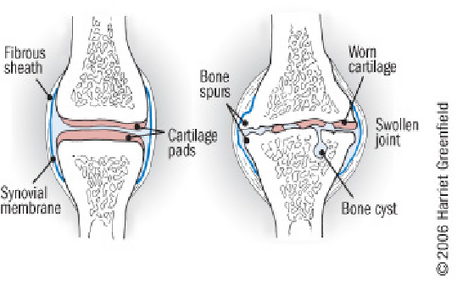
Osteoarthritis is common, affecting ~25% of adults. The prevalence increases with age. In the age group below 50 years, men are more often affected, while in the older population the disease is more common in women. It is estimated that over 300 million people in the world suffered from OA in 2017. | [[File:Osteoarthritis in the Hip.jpg|thumb|219x219px|OA hip]] | ||
Osteoarthritis is common, affecting ~25% of adults. The prevalence increases with age. In the age group below 50 years, men are more often affected, while in the older population the disease is more common in women. It is estimated that over 300 million people in the world suffered from OA in 2017.<ref name=":1" /> | |||
* 80% of the United States population over 65 years old has radiographic evidence of OA, with 60% of this subset having symptoms (radiographic OA is at least twice as common as symptomatic OA). | * 80% of the United States population over 65 years old has radiographic evidence of OA, with 60% of this subset having symptoms (radiographic OA is at least twice as common as symptomatic OA). | ||
| Line 21: | Line 26: | ||
Note changes on radiograph do not prove that OA is the cause of the patient’s joint pain.<ref name=":0">Pearl Stats [https://www.ncbi.nlm.nih.gov/books/NBK482326/ Osteoarthritis] Available from: https://www.ncbi.nlm.nih.gov/books/NBK482326/ (last accessed 28.5.2019)</ref> <u></u> | Note changes on radiograph do not prove that OA is the cause of the patient’s joint pain.<ref name=":0">Pearl Stats [https://www.ncbi.nlm.nih.gov/books/NBK482326/ Osteoarthritis] Available from: https://www.ncbi.nlm.nih.gov/books/NBK482326/ (last accessed 28.5.2019)</ref> <u></u> | ||
== Etiology == | == Etiology == | ||
[[File:Overweight biker.jpg|thumb|Obesity a cause of OA]] | |||
Risk factors for developing OA include age, female gender, obesity, anatomical factors, muscle weakness, and joint injury (occupation/sports activities).<ref name=":0" /> | Risk factors for developing OA include age, female gender, obesity, anatomical factors, muscle weakness, and joint injury (occupation/sports activities).<ref name=":0" /> | ||
We define two types of OA, primary and secondary. Both involve the breakdown of cartilage in joints, which causes bones to rub together. | We define two types of OA, primary and secondary. Both involve the breakdown of cartilage in joints, which causes bones to rub together. | ||
'''Primary Osteoarthritis:''' absence of an antecedent insult. A strong genetic component with the disease primarily affecting middle-aged women[[File:Knee osteoarthritis xray.jpg|thumb|Knee OA: caused by old injury?]]'''Secondary Osteoarthritis: I'''nvolves a specific trigger that exacerbates cartilage breakdown. Common triggers for secondary OA include | |||
* Injury: Bone [[Fracture|fractures]] increase a person’s chance of developing OA and can bring about the disease earlier. | |||
* Abnormal mechanical forces (e.g. occupational stress, [[obesity]])<ref name=":1" /> <ref>Akazawa N, Okawa N, Kishi M, Hino T, Tsuji R, Tamura K, Moriyama H. [https://www.ncbi.nlm.nih.gov/pubmed/31811998 Quantitative features of intramuscular adipose tissue of the quadriceps and their association with gait independence in older inpatients: A cross-sectional study]. Nutrition. 2020 Mar 1;71:110600.</ref> | |||
* Inactivity | * Inactivity | ||
* Inflammatory Diseases: [[Perthes|Perthes']] disease,[[Lyme Disease|Lyme]] disease and all chronic forms of arthritis (e.g., [[costochondritis]], [[gout]], and [[Rheumatoid Arthritis|rheumatoid arthritis)]] | |||
* History of certain conditions eg [[Diabetes]], [[Marfan Syndrome]], Wilson's Disease, Joint infection, Congenital disorders of joints, [[Ehlers-Danlos Syndrome|Ehlers-]]Danlos Syndrome, [[Hemochromatosis]]<ref>Wikipedia [https://en.wikipedia.org/wiki/Osteoarthritis#Secondary Osteoarthritis] Available from: https://en.wikipedia.org/wiki/Osteoarthritis#Secondary (last accessed 29.5.2019)</ref> | |||
* Inflammatory Diseases: [[Perthes|Perthes']] disease,[[Lyme Disease|Lyme]] disease and all chronic forms of arthritis (e.g., costochondritis, [[gout]], and [[Rheumatoid Arthritis|rheumatoid arthritis)]] | |||
* History of certain conditions eg [[Diabetes]], [[Marfan Syndrome]], Wilson's Disease, Joint infection | |||
== Characteristics and Clinical Presentation == | == Characteristics and Clinical Presentation == | ||
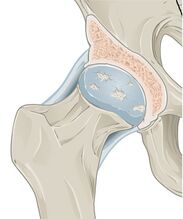
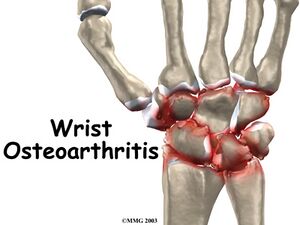
[[File: | [[File:Wrist osteoarthritis intro01.jpg|thumb|Wrist Osteoarthritis]] | ||
OA can affect any joint, but it occurs most often in knees, hips, lower back and neck, small joints of the fingers and the bases of the thumb and big toe | OA can affect any joint, but it occurs most often in knees, hips, lower back and neck, small joints of the fingers and the bases of the thumb and big toe | ||
| Line 55: | Line 54: | ||
*Difficult and painful mobilization: It's important to differentiate between total blocking and limited mobility. Total blocking is caused by the presence of meniscus, unusual structures, etc.and will need further investigation. | *Difficult and painful mobilization: It's important to differentiate between total blocking and limited mobility. Total blocking is caused by the presence of meniscus, unusual structures, etc.and will need further investigation. | ||
*Mild swelling around a joint. | *Mild swelling around a joint. | ||
== Management == | |||
[[File:Knee ext in sitting.png|thumb|Exercise: part of treatment of OA]] | |||
Treatment goals for OA are to minimize pain and functional loss. Management of the disease involves both non-pharmacologic and pharmacologic therapies. Non pharmacological treatment is tried first. | |||
== | |||
[[File: | |||
Mainstays for non-pharmacologic therapy include: avoidance of activities exacerbating pain or overloading the joint; exercise to improve strength; weight loss, if needed, and; unloading joints via brace, splint, cane, or crutch. | |||
Formal physical therapy can immensely assist patients in using equipment (eg correct canes use) while also instructing them on exercises. Exercise programs that combine both aerobic and resistance training have been shown to decrease pain and improve physical function in multiple trials and should be encouraged. | |||
= | Malaligned of joints can be corrected via mechanical means such as realignment knee brace or orthotics.<ref name=":2" /> | ||
== Pharmacologic Therapies == | |||
[[File:Extra_Strength_Tylenol_and_Tylenol_PM.jpg|alt=|right|frameless|250x250px]] | |||
Pharmacotherapy of OA involves oral, topical, and/or intraarticular options. | |||
# Acetaminophen (panadol) and oral NSAIDs are usually the initial choice. NSAIDs are usually prescribed orally or topically and, initially, should be started as needed rather than scheduled. Be aware of the risk of [[NSAID Gastropathy]]Topical NSAIDs are less effective than their oral counterparts but have fewer gastrointestinal and other systemic side effects (they may cause local skin irritation). | |||
# Intra-articular injections: 1.Corticosteroids- Consider when patients are having flare-ups and is not responding to paracetamol and NSAIDs. 2.Platelet-rich plasma (evidence still lacking) 3.Hyaluronic acid - Evidence still lacking for effectiveness in the management of osteoarthritis | |||
# Disease-modifying osteoarthritis drugs (research on this topic still ongoing)<ref>Physiopedia [[Hip Osteoarthritis]] Available from: https://physio-pedia.com/Hip_Osteoarthritis (last accessed 30.5.2019)</ref> eg There are a number of stem cell treatments currently available for osteoarthritis, however there is no credible evidence base for their use and they are often expensive.<ref>Arthritis Queensland. [https://www.arthritis.org.au/arthritis/arthritis-insights/stem-cell-treatments-for-osteoarthritis-what-you-need-to-know/ Stem Cell Treatments For Osteoarthritis What You Need To Know] Available from: https://www.arthritis.org.au/arthritis/arthritis-insights/stem-cell-treatments-for-osteoarthritis-what-you-need-to-know/ (last accessed 30.5.2019)</ref> | |||
Intra-articular injections: 1.Corticosteroids- Consider when patients are having flare-ups and is not responding to paracetamol and NSAIDs. 2.Platelet-rich plasma (evidence still lacking) 3.Hyaluronic acid - Evidence still lacking for effectiveness in the management of osteoarthritis | |||
Disease-modifying osteoarthritis drugs (research on this topic still ongoing)<ref>Physiopedia [[Hip Osteoarthritis]] Available from: https://physio-pedia.com/Hip_Osteoarthritis (last accessed 30.5.2019)</ref> eg There are a number of stem cell treatments currently available for osteoarthritis, however there is no credible evidence base for their use and they are often expensive.<ref>Arthritis Queensland. [https://www.arthritis.org.au/arthritis/arthritis-insights/stem-cell-treatments-for-osteoarthritis-what-you-need-to-know/ Stem Cell Treatments For Osteoarthritis What You Need To Know] Available from: https://www.arthritis.org.au/arthritis/arthritis-insights/stem-cell-treatments-for-osteoarthritis-what-you-need-to-know/ (last accessed 30.5.2019)</ref> | |||
If you are wondering what disease modifying treatments are look at the below, with an obvious bias. | If you are wondering what disease modifying treatments are look at the below, with an obvious bias. | ||
{{#ev:youtube|https://www.youtube.com/watch?v=BgPI7lvIHqM|width}}<ref>R3 Stem Cell The Difference Between PRP Therapy and Stem Cell Treatment Available from: https://www.youtube.com/watch?v=BgPI7lvIHqM (last accessed 30.5.2019)</ref> | {{#ev:youtube|https://www.youtube.com/watch?v=BgPI7lvIHqM|width}}<ref>R3 Stem Cell The Difference Between PRP Therapy and Stem Cell Treatment Available from: https://www.youtube.com/watch?v=BgPI7lvIHqM (last accessed 30.5.2019)</ref> | ||
== Assistive Devices == | ==== Assistive Devices ==== | ||
[[File:Cane length.jpg| | [[File:Cane length.jpg|227x227px|alt=|thumb|Check cane length]] | ||
[[Assistive Devices|Assistive devices]] can help with function and mobility. Physiotherapists are ideally placed to recommend, fit and or teach use of these devices.These include items, such as like scooters, canes, walkers, splints, shoe orthotics or helpful tools, such as jar openers, long-handled shoe horns or steering wheel grips. Some like braces and foot orthotics need to be fitted by a therapist. | [[Assistive Devices|Assistive devices]] can help with function and mobility. Physiotherapists are ideally placed to recommend, fit and or teach use of these devices.These include items, such as like scooters, canes, walkers, splints, shoe orthotics or helpful tools, such as jar openers, long-handled shoe horns or steering wheel grips. Some like braces and foot orthotics need to be fitted by a therapist. | ||
== Surgery == | ==== Surgery ==== | ||
Joint surgery can repair or replace severely damaged joints, especially hips or knees. A doctor will refer an eligible patient to an orthopaedic surgeon to perform the procedure. | Joint surgery can repair or replace severely damaged joints, especially hips or knees. A doctor will refer an eligible patient to an orthopaedic surgeon to perform the procedure.<br> | ||
== Physiotherapy Management == | |||
[[File:Don't sit still for arthritis pain (4648303320).jpg|right|frameless]] | |||
OA causes reduced muscle strength (particularly in those muscles around the affect joint), decreased flexibility, weight gain, limitation in the ability to do ADL-activities and often compromised mobility. Increased physical and psychological function and an increased feeling of well-being are the main goals of an integrated exercise program. Increased joint motion, enhancing muscle strength, increased aerobic capacity and optimal body weight are immediate objectives.<ref name="McCarty">McCarty DJ, Koopman WJ. Arthritis and allied conditions. Lea & Febiger: Philidelphia, London, 1993.</ref> | OA causes reduced muscle strength (particularly in those muscles around the affect joint), decreased flexibility, weight gain, limitation in the ability to do ADL-activities and often compromised mobility. Increased physical and psychological function and an increased feeling of well-being are the main goals of an integrated exercise program. Increased joint motion, enhancing muscle strength, increased aerobic capacity and optimal body weight are immediate objectives.<ref name="McCarty">McCarty DJ, Koopman WJ. Arthritis and allied conditions. Lea & Febiger: Philidelphia, London, 1993.</ref> | ||
| Line 145: | Line 93: | ||
=== Typical Treatment Plans for OA === | === Typical Treatment Plans for OA === | ||
==== Basic Physiotherapy<ref name="p6">Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M. [https://www.sciencedirect.com/science/article/pii/S1063458407003974 OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines.] Osteoarthritis and cartilage 2008;16(2):137-62.</ref> ==== | ==== Basic Physiotherapy<ref name="p6">Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M. [https://www.sciencedirect.com/science/article/pii/S1063458407003974 OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines.] Osteoarthritis and cartilage 2008;16(2):137-62.</ref>==== | ||
Not for patients with acute painful joint swelling and cardiovascular diseases. | Not for patients with acute painful joint swelling and cardiovascular diseases. | ||
*Warm-up and range of motion<ref name="McCarty" /> | *Warm-up and range of motion<ref name="McCarty" /> | ||
*Strengthening (quad sets, supine straight leg raises, prone hip extensions, seated isometric knee extensions, single-leg leg presses, standing hamstring curls, and standing heel raises) | *Strengthening (quad sets, supine straight leg raises, prone hip extensions, seated isometric knee extensions, single-leg leg presses, standing hamstring curls, and standing heel raises) | ||
*Aerobic program<ref name="McCarty" /> | *Aerobic program<ref name="McCarty" /> | ||
*Cooling down with muscle stretching (quadriceps femoris, [[Hamstrings|hamstring]], and calf muscle stretching) | *Cooling down with muscle stretching (quadriceps femoris, [[Hamstrings|hamstring]], and calf muscle stretching) | ||
*Long-sitting knee flexion and extension range of motion, and treadmill walking | *Long-sitting knee flexion and extension range of motion, and treadmill walking | ||
| Line 156: | Line 104: | ||
*Manual therapy can be used as a treatment tool for osteoarthritis. According to a systematic review, manual therapy (mobilisation with movement, passive joint mobilisation, patellar mobilisation therapy ) and exercises effectively reduce knee pain and increase functionality. However, further research is needed to determine the long-term effects of manual therapy on knee OA. <ref>Tsokanos A, Livieratou E, Billis E, Tsekoura M, Tatsios P, Tsepis E, Fousekis K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8304320/ The Efficacy of Manual Therapy in Patients with Knee Osteoarthritis: A Systematic Review.] Medicina. 2021 Jul;57(7):696.</ref><br> | *Manual therapy can be used as a treatment tool for osteoarthritis. According to a systematic review, manual therapy (mobilisation with movement, passive joint mobilisation, patellar mobilisation therapy ) and exercises effectively reduce knee pain and increase functionality. However, further research is needed to determine the long-term effects of manual therapy on knee OA. <ref>Tsokanos A, Livieratou E, Billis E, Tsekoura M, Tatsios P, Tsepis E, Fousekis K. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8304320/ The Efficacy of Manual Therapy in Patients with Knee Osteoarthritis: A Systematic Review.] Medicina. 2021 Jul;57(7):696.</ref><br> | ||
==== Agility and Perturbation Training Techniques<ref name="p7">Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. [https://academic.oup.com/ptj/article/91/4/452/2734990 Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial.] Physical therapy 2011;91(4):452-69.</ref> ==== | ==== Agility and Perturbation Training Techniques<ref name="p7">Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. [https://academic.oup.com/ptj/article/91/4/452/2734990 Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial.] Physical therapy 2011;91(4):452-69.</ref>==== | ||
Agility techniques: | Agility techniques: | ||
*Side stepping | *Side stepping | ||
*Braiding (lateral stepping combined with forward and backward crossover steps) | *Braiding (lateral stepping combined with forward and backward crossover steps) | ||
* Front crossover steps during forward ambulation | * Front crossover steps during forward ambulation | ||
* Back crossover steps during backward ambulation | * Back crossover steps during backward ambulation | ||
*Shuttle walking(forward and backward walking to and from designated markers) | *Shuttle walking(forward and backward walking to and from designated markers) | ||
*A drill requiring multiple changes in direction | *A drill requiring multiple changes in direction | ||
*[[Perturbation-Based Balance Training|Perturbation techniques]] and [[Balance Boards|balance]] training | *[[Perturbation-Based Balance Training|Perturbation techniques]] and [[Balance Boards|balance]] training | ||
| Line 172: | Line 120: | ||
The video below gives some sound basic physiotherapy exercises for all the major joints | The video below gives some sound basic physiotherapy exercises for all the major joints | ||
{{#ev:youtube|https://www.youtube.com/watch?v=FBqxjYvnUI8|width}}<ref>Nuffeild Health How to exercise safely with osteoarthritis. Available from: https://www.youtube.com/watch?v=FBqxjYvnUI8 (last accessed 28.5.2019)</ref> | {{#ev:youtube|https://www.youtube.com/watch?v=FBqxjYvnUI8|width}}<ref>Nuffeild Health How to exercise safely with osteoarthritis. Available from: https://www.youtube.com/watch?v=FBqxjYvnUI8 (last accessed 28.5.2019)</ref> | ||
== Differential Diagnosis == | |||
Diagnosing OA is usually fairly straight forward. In cases were it is not consider: | |||
* Periarticular structure derrangement: Periarticular pain that is not reproduced by passive motion or palpation of the joint should suggest an alternate etiology such as bursitis, tendonitis or periostitis. | |||
* Inflammatory arthritis: If the distribution of painful joints includes MCP, wrist, elbow, ankle or shoulder, OA is unlikely, unless there are specific risk factors (such as occupational, sports-related, history of injury). Prolonged stiffness (greater than one hour) points more to an inflammatory arthritis eg rheumatoid arthritis. Marked warmth and erythema in a joint suggests a crystalline etiology. Arthrocentesis (aspiration of the joint) helps aid in distinguishing between these types of arthritis if the diagnosis is not clear by history, physical exam, and radiographs. If an infected joint is suspected it should be aspirated and the fluid sent for culture. | |||
* Other inflammatory / systemic condition: Weight loss, fatigue, fever and loss of appetite suggestive of a systemic illness eg [[Polymyalgia Rheumatica|polymyalgia]] rheumatica, [[Rheumatoid Arthritis|rheumatoid arthritis]], [[Systemic Lupus Erythematosus|lupus]] or sepsis or malignancy.<ref>John Hopkins Arthritis Centre [https://www.hopkinsarthritis.org/arthritis-info/osteoarthritis/oa-differential-diagnosis/ Osteoarthritis] Available from: https://www.hopkinsarthritis.org/arthritis-info/osteoarthritis/oa-differential-diagnosis/ (last accessed 29.5.2019)</ref> | |||
== Diagnostic Procedures == | |||
[[File:Stages Knee OA.jpg|thumb|Osteoarthritis of the knee]] | |||
The severity of osteoarthritis can be evaluated by [[X-Rays|radiography]], according the Kellgren<ref name="Kellgren">Kellgren JH. Atlas of standard radiographs of arthritis. Volume II of The Epidemiologic of Chronic Rheumatism. Oxford: Blackwell, 1963.</ref>. By this way, we can discriminate four degrees of severity in osteoarthritis:<br>Degree I: normal joint with a minimal osteophyte.<br>Degree II: Osteophytose on two points with minimal subchondral sclerosis, proper joint space and no deformity.<br>Degree III: Moderate osteophytose, early deformity of the bone endings and a joint space which narrows.<br>Degree IV: Large osteophytes, deformity of bone endings, narrowing joint space, sclerosis and cysts. | |||
== Outcome Measures == | |||
=== Outcome Measures Emphasizing the Pain Component of Osteoarthritis === | |||
* [[Hip Disability and Osteoarthritis Outcome Score|Hip Disability and Osteoarthritis Outcome Score]]<ref name="groot">De Groot IB, Reijman M, Terwee CB, Bierma-Zeinstra SM, Favejee M, Roos EM, Verhaar JA. [https://www.sciencedirect.com/science/article/pii/S1063458406002020 Validation of the Dutch version of the Hip disability and Osteoarthritis Outcome Score.] Osteoarthritis and cartilage 2007;15(1):104-9.</ref> | |||
*[[Knee Injury and Osteoarthritis Outcome Score|Knee Injury and Osteoarthritis Outcome Score]] | |||
*Western Ontario and McMaster Universities Osteoarthritis Index, also known as [[WOMAC Osteoarthritis Index]] | |||
*[[Oxford Hip Score]] | |||
**A 12 item subjective questionnaire to measure the outcome of total hip replacement. | |||
*Oxford Knee Score | |||
**Developed as an outcome measure to be used with patients having a total knee replacement. | |||
*[[Short-form McGill Pain Questionnaire|McGill Pain Questionnaire Short-Form]] | |||
**Created to assess both the intensity and quality of pain. | |||
*[[Knee Injury and Osteoarthritis Outcome Score]] | |||
=== Outcome Measures Emphasizing Activities of Daily Living (ADL) Component of Osteoarthritis === | |||
*[[36-Item Short Form Survey (SF-36)|Medical Outcomes Study Short Form 36]] | |||
**The SF-36 is a generic patient-reported outcome measure aimed at quantifying health status, and is often used as a measure of health-related quality of life. | |||
*[https://www.who.int/substance_abuse/research_tools/whoqolbref/en/ WHO Quality of Life-BREF] (WHOQOL-BREF) | |||
**Assesses quality of life (QOL) within the context of an individual's culture, value systems, personal goals, standards and concerns | |||
*[[Physical Activity Scale for the Elderly (PASE)|Physical Activity Scale for the Elderly]] | |||
**Measures the level of self-reported physical activity in individuals aged 65 years or older and is comprised of items regarding occupational, household, and leisure activities during the previous 7-day period. | |||
*[[Lower Extremity Functional Scale (LEFS)|Lower Extremity Functional Scale]] | |||
**Used to evaluate the impairment of a patient with lower extremity musculoskeletal condition or disorders. Can be used clinically to measure the patients’ initial function, ongoing progress, and outcome as well as to set functional goals | |||
*[[Knee Injury and Osteoarthritis Outcome Score]] | |||
== Resources == | == Resources == | ||
| Line 188: | Line 174: | ||
[[Category:Course Pages]] | [[Category:Course Pages]] | ||
[[Category:Plus Content]] | [[Category:Plus Content]] | ||
[[Category:Rheumatology]] | |||
Latest revision as of 12:17, 21 September 2023
Original Editors - Rachael Lowe Top Contributors - Dorien De Strijcker, Kevin Campion, Lucinda hampton, Admin, Sheik Abdul Khadir, Kim Jackson, Rachael Lowe, Vidya Acharya, Lauren Lopez, WikiSysop, Leana Louw, Tarina van der Stockt, 127.0.0.1, Tony Lowe, Hamelryck Sascha, Evan Thomas, George Prudden, Elvira Muhic and Simisola Ajeyalemi
Introduction[edit | edit source]
Osteoarthritis (OA), also known as degenerative joint disease (DJD), is the most common form of arthritis.[1] It can be classified into two categories: primary osteoarthritis and secondary osteoarthritis. OA usuallly presents with joint pain and loss of function; however, the disease is clinically very variable and can present merely as an asymptomatic incidental finding to a devastating, permanently disabling disorder.[2]
The 4 and a 12 minute video below gives an overview of OA. Press youtube link.
Pathophysiology[edit | edit source]
In normal joints hyaline cartilage covers the end of each bone. Hyaline cartilage provides a smooth, gliding surface for joint motion and acts as a cushion between the bones. In OA, the cartilage breaks down, causing pain, swelling and problems moving the joint. As OA worsens over time, bones may break down and develop growths called spurs. Bits of bone or cartilage may flake off and float around in the joint. In the body, an inflammatory process occurs and cytokines and enzymes develop, furtherer damaging the cartilage. In the final stages of OA, the cartilage wears away and bone rubs against bone leading to joint damage and more pain.[4]
Osteoarthritis: "A group of overlapping distinct diseases, which may have different etiologies but with similar biologic, morphologic, and clinical outcomes. The disease processes not only affect the articular cartilage, but involve the entire joint, including the subchondral bone, ligaments, capsule, synovial membrane, and periarticular muscles. Ultimately, the articular cartilage degenerates with fibrillation, fissures, ulceration, and full thickness loss of the joint surface." [5]
Epidemiology[edit | edit source]
Osteoarthritis is common, affecting ~25% of adults. The prevalence increases with age. In the age group below 50 years, men are more often affected, while in the older population the disease is more common in women. It is estimated that over 300 million people in the world suffered from OA in 2017.[1]
- 80% of the United States population over 65 years old has radiographic evidence of OA, with 60% of this subset having symptoms (radiographic OA is at least twice as common as symptomatic OA).
- 1 in 5 Australians (21%) over the age of 45 have osteoarthritis. It is most common in adults aged 80 years and older, with just over one-third (35%) of people in this age group reporting the condition.[6]
- Across the EU Member States, diagnosed OA prevalence varies from 2.8% in Romania to 18.3% in Hungary.[7]
Note changes on radiograph do not prove that OA is the cause of the patient’s joint pain.[8]
Etiology[edit | edit source]
Risk factors for developing OA include age, female gender, obesity, anatomical factors, muscle weakness, and joint injury (occupation/sports activities).[8]
We define two types of OA, primary and secondary. Both involve the breakdown of cartilage in joints, which causes bones to rub together.
Primary Osteoarthritis: absence of an antecedent insult. A strong genetic component with the disease primarily affecting middle-aged women
Secondary Osteoarthritis: Involves a specific trigger that exacerbates cartilage breakdown. Common triggers for secondary OA include
- Injury: Bone fractures increase a person’s chance of developing OA and can bring about the disease earlier.
- Inactivity
- Inflammatory Diseases: Perthes' disease,Lyme disease and all chronic forms of arthritis (e.g., costochondritis, gout, and rheumatoid arthritis)
- History of certain conditions eg Diabetes, Marfan Syndrome, Wilson's Disease, Joint infection, Congenital disorders of joints, Ehlers-Danlos Syndrome, Hemochromatosis[10]
Characteristics and Clinical Presentation[edit | edit source]
OA can affect any joint, but it occurs most often in knees, hips, lower back and neck, small joints of the fingers and the bases of the thumb and big toe
Clinical signs depend mainly to the affected joint but usually, they show some common characteristics. They're mainly local. Symptoms are[11]:
- Pain: This is a 'mechanical' type of pain which is generated by mobilization, increases with fatigue and decreases with rest. Pain occurs in the morning or after a period of inactivity. Mostly, there's no overnight pain. The intensity of pain is variable. Sometimes it's dull and tolerable, other times it's very heavy with short peaks. It can be stimulated by cold, trauma and fatigue. This pain occurs at the level of the subchondral bone and in capsuloligamentar and muscular structures.
- Limitation in movement (loss of ROM): Limitation in movements is insidious, progressive and will be noticed after several years. This limitation is mainly related to the blocking of voluntary muscle functioning and the reflex contracture. It's also the result of changes in the articular spaces, with incongruent joint surfaces. Some patients complain about stiffness in the morning, which holds on for a longer period but is less severe than the morning stiffness from rheumatoid arthritis or ankylosing spondylitis. The severity increases with time and is accompanied with the joint deformities and wear of the cartilage.
- Sounds: The sounds you can hear are cracking, scraping and sounds from crepitation. They're generated by mobilization of the joint. Irregularities in the articulating joint surfaces and poor quality of the remaining cartilage is very likely to be the cause.
- Difficult and painful mobilization: It's important to differentiate between total blocking and limited mobility. Total blocking is caused by the presence of meniscus, unusual structures, etc.and will need further investigation.
- Mild swelling around a joint.
Management[edit | edit source]
Treatment goals for OA are to minimize pain and functional loss. Management of the disease involves both non-pharmacologic and pharmacologic therapies. Non pharmacological treatment is tried first.
Mainstays for non-pharmacologic therapy include: avoidance of activities exacerbating pain or overloading the joint; exercise to improve strength; weight loss, if needed, and; unloading joints via brace, splint, cane, or crutch.
Formal physical therapy can immensely assist patients in using equipment (eg correct canes use) while also instructing them on exercises. Exercise programs that combine both aerobic and resistance training have been shown to decrease pain and improve physical function in multiple trials and should be encouraged.
Malaligned of joints can be corrected via mechanical means such as realignment knee brace or orthotics.[2]
Pharmacologic Therapies[edit | edit source]
Pharmacotherapy of OA involves oral, topical, and/or intraarticular options.
- Acetaminophen (panadol) and oral NSAIDs are usually the initial choice. NSAIDs are usually prescribed orally or topically and, initially, should be started as needed rather than scheduled. Be aware of the risk of NSAID GastropathyTopical NSAIDs are less effective than their oral counterparts but have fewer gastrointestinal and other systemic side effects (they may cause local skin irritation).
- Intra-articular injections: 1.Corticosteroids- Consider when patients are having flare-ups and is not responding to paracetamol and NSAIDs. 2.Platelet-rich plasma (evidence still lacking) 3.Hyaluronic acid - Evidence still lacking for effectiveness in the management of osteoarthritis
- Disease-modifying osteoarthritis drugs (research on this topic still ongoing)[12] eg There are a number of stem cell treatments currently available for osteoarthritis, however there is no credible evidence base for their use and they are often expensive.[13]
If you are wondering what disease modifying treatments are look at the below, with an obvious bias.
Assistive Devices[edit | edit source]
Assistive devices can help with function and mobility. Physiotherapists are ideally placed to recommend, fit and or teach use of these devices.These include items, such as like scooters, canes, walkers, splints, shoe orthotics or helpful tools, such as jar openers, long-handled shoe horns or steering wheel grips. Some like braces and foot orthotics need to be fitted by a therapist.
Surgery[edit | edit source]
Joint surgery can repair or replace severely damaged joints, especially hips or knees. A doctor will refer an eligible patient to an orthopaedic surgeon to perform the procedure.
Physiotherapy Management[edit | edit source]
OA causes reduced muscle strength (particularly in those muscles around the affect joint), decreased flexibility, weight gain, limitation in the ability to do ADL-activities and often compromised mobility. Increased physical and psychological function and an increased feeling of well-being are the main goals of an integrated exercise program. Increased joint motion, enhancing muscle strength, increased aerobic capacity and optimal body weight are immediate objectives.[15]
Falls prevention strategies also play an important role in therapy for older clients. People with osteoarthris are also more prone to falls. Studies have found that OA sufferers compared to non have 30 percent increase in falls and have a 20 percent greater risk of fracture. People with OA have risk factors such as decreased function, muscle weakness and impaired balance that make them more likely to fall. Side effects from medications used for pain relief can also contribute to falls. Narcotic pain relievers can cause people to feel dizzy and unbalanced.
Physiotherapy is important part of OA management and will be instrumental in teaching people to: properly use joints; exercise correctly in both motion and flexibility exercises as well as cardiovascular exercises (e.g.hydrotherapy, swimming), recommend assistive devices, recommend use of modalities (eg. heat or cold therapies, TENS).
Typical Treatment Plans for OA[edit | edit source]
Basic Physiotherapy[16][edit | edit source]
Not for patients with acute painful joint swelling and cardiovascular diseases.
- Warm-up and range of motion[15]
- Strengthening (quad sets, supine straight leg raises, prone hip extensions, seated isometric knee extensions, single-leg leg presses, standing hamstring curls, and standing heel raises)
- Aerobic program[15]
- Cooling down with muscle stretching (quadriceps femoris, hamstring, and calf muscle stretching)
- Long-sitting knee flexion and extension range of motion, and treadmill walking
- All lower-extremity exercises need to be performed bilaterally
- Manual therapy can be used as a treatment tool for osteoarthritis. According to a systematic review, manual therapy (mobilisation with movement, passive joint mobilisation, patellar mobilisation therapy ) and exercises effectively reduce knee pain and increase functionality. However, further research is needed to determine the long-term effects of manual therapy on knee OA. [17]
Agility and Perturbation Training Techniques[18][edit | edit source]
Agility techniques:
- Side stepping
- Braiding (lateral stepping combined with forward and backward crossover steps)
- Front crossover steps during forward ambulation
- Back crossover steps during backward ambulation
- Shuttle walking(forward and backward walking to and from designated markers)
- A drill requiring multiple changes in direction
- Perturbation techniques and balance training
Falls Prevention training see Falls in Elderly
The video below gives some sound basic physiotherapy exercises for all the major joints
Differential Diagnosis[edit | edit source]
Diagnosing OA is usually fairly straight forward. In cases were it is not consider:
- Periarticular structure derrangement: Periarticular pain that is not reproduced by passive motion or palpation of the joint should suggest an alternate etiology such as bursitis, tendonitis or periostitis.
- Inflammatory arthritis: If the distribution of painful joints includes MCP, wrist, elbow, ankle or shoulder, OA is unlikely, unless there are specific risk factors (such as occupational, sports-related, history of injury). Prolonged stiffness (greater than one hour) points more to an inflammatory arthritis eg rheumatoid arthritis. Marked warmth and erythema in a joint suggests a crystalline etiology. Arthrocentesis (aspiration of the joint) helps aid in distinguishing between these types of arthritis if the diagnosis is not clear by history, physical exam, and radiographs. If an infected joint is suspected it should be aspirated and the fluid sent for culture.
- Other inflammatory / systemic condition: Weight loss, fatigue, fever and loss of appetite suggestive of a systemic illness eg polymyalgia rheumatica, rheumatoid arthritis, lupus or sepsis or malignancy.[20]
Diagnostic Procedures[edit | edit source]
The severity of osteoarthritis can be evaluated by radiography, according the Kellgren[21]. By this way, we can discriminate four degrees of severity in osteoarthritis:
Degree I: normal joint with a minimal osteophyte.
Degree II: Osteophytose on two points with minimal subchondral sclerosis, proper joint space and no deformity.
Degree III: Moderate osteophytose, early deformity of the bone endings and a joint space which narrows.
Degree IV: Large osteophytes, deformity of bone endings, narrowing joint space, sclerosis and cysts.
Outcome Measures[edit | edit source]
Outcome Measures Emphasizing the Pain Component of Osteoarthritis[edit | edit source]
- Knee Injury and Osteoarthritis Outcome Score
- Western Ontario and McMaster Universities Osteoarthritis Index, also known as WOMAC Osteoarthritis Index
- Oxford Hip Score
- A 12 item subjective questionnaire to measure the outcome of total hip replacement.
- Oxford Knee Score
- Developed as an outcome measure to be used with patients having a total knee replacement.
- McGill Pain Questionnaire Short-Form
- Created to assess both the intensity and quality of pain.
- Knee Injury and Osteoarthritis Outcome Score
Outcome Measures Emphasizing Activities of Daily Living (ADL) Component of Osteoarthritis[edit | edit source]
- Medical Outcomes Study Short Form 36
- The SF-36 is a generic patient-reported outcome measure aimed at quantifying health status, and is often used as a measure of health-related quality of life.
- WHO Quality of Life-BREF (WHOQOL-BREF)
- Assesses quality of life (QOL) within the context of an individual's culture, value systems, personal goals, standards and concerns
- Physical Activity Scale for the Elderly
- Measures the level of self-reported physical activity in individuals aged 65 years or older and is comprised of items regarding occupational, household, and leisure activities during the previous 7-day period.
- Lower Extremity Functional Scale
- Used to evaluate the impairment of a patient with lower extremity musculoskeletal condition or disorders. Can be used clinically to measure the patients’ initial function, ongoing progress, and outcome as well as to set functional goals
- Knee Injury and Osteoarthritis Outcome Score
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Radiopedia Osteoarthritis Available:https://radiopaedia.org/articles/osteoarthritis (accessed 3.9.2022)
- ↑ 2.0 2.1 Sen R, Hurley JA. Osteoarthritis. InStatPearls [Internet] 2021 Aug 19. StatPearls Publishing. Available:https://www.ncbi.nlm.nih.gov/books/NBK482326/ (accessed 3.9.2022)
- ↑ Nucleus medical media Osteoarthritis | Nucleus Health Available from: https://www.youtube.com/watch?v=41IMR_Dp5bs (last accessed 28.5.2019)
- ↑ Arthritis foundation What is arthritis Available from: https://www.arthritis.org/about-arthritis/types/osteoarthritis/what-is-osteoarthritis.php (last accessed 28.5.2019)
- ↑ Kuttner K, Goldberg VM. Osteoarthritis disorders Rosemout. InAmerican Academy of, Orthopedic Surgeons 1995 (pp. 21-25).
- ↑ AIHW Osteoarthritis snap shot 2018 Available from: https://www.aihw.gov.au/reports/chronic-musculoskeletal-conditions/osteoarthritis/contents/what-is-osteoarthritis (last accessed 28.5.2019)
- ↑ WHO internet Osteoarthritis Available from: https://www.who.int/medicines/areas/priority_medicines/Ch6_12Osteo.pdf (last accessed 28.5.2019)
- ↑ 8.0 8.1 Pearl Stats Osteoarthritis Available from: https://www.ncbi.nlm.nih.gov/books/NBK482326/ (last accessed 28.5.2019)
- ↑ Akazawa N, Okawa N, Kishi M, Hino T, Tsuji R, Tamura K, Moriyama H. Quantitative features of intramuscular adipose tissue of the quadriceps and their association with gait independence in older inpatients: A cross-sectional study. Nutrition. 2020 Mar 1;71:110600.
- ↑ Wikipedia Osteoarthritis Available from: https://en.wikipedia.org/wiki/Osteoarthritis#Secondary (last accessed 29.5.2019)
- ↑ Crielaard JM, Dequeker J, Famaey JP. Osteoartrose. Brussels: Drukkerij Lichtert, 1985.
- ↑ Physiopedia Hip Osteoarthritis Available from: https://physio-pedia.com/Hip_Osteoarthritis (last accessed 30.5.2019)
- ↑ Arthritis Queensland. Stem Cell Treatments For Osteoarthritis What You Need To Know Available from: https://www.arthritis.org.au/arthritis/arthritis-insights/stem-cell-treatments-for-osteoarthritis-what-you-need-to-know/ (last accessed 30.5.2019)
- ↑ R3 Stem Cell The Difference Between PRP Therapy and Stem Cell Treatment Available from: https://www.youtube.com/watch?v=BgPI7lvIHqM (last accessed 30.5.2019)
- ↑ 15.0 15.1 15.2 McCarty DJ, Koopman WJ. Arthritis and allied conditions. Lea & Febiger: Philidelphia, London, 1993.
- ↑ Zhang W, Moskowitz RW, Nuki G, Abramson S, Altman RD, Arden N, Bierma-Zeinstra S, Brandt KD, Croft P, Doherty M, Dougados M. OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines. Osteoarthritis and cartilage 2008;16(2):137-62.
- ↑ Tsokanos A, Livieratou E, Billis E, Tsekoura M, Tatsios P, Tsepis E, Fousekis K. The Efficacy of Manual Therapy in Patients with Knee Osteoarthritis: A Systematic Review. Medicina. 2021 Jul;57(7):696.
- ↑ Fitzgerald GK, Piva SR, Gil AB, Wisniewski SR, Oddis CV, Irrgang JJ. Agility and perturbation training techniques in exercise therapy for reducing pain and improving function in people with knee osteoarthritis: a randomized clinical trial. Physical therapy 2011;91(4):452-69.
- ↑ Nuffeild Health How to exercise safely with osteoarthritis. Available from: https://www.youtube.com/watch?v=FBqxjYvnUI8 (last accessed 28.5.2019)
- ↑ John Hopkins Arthritis Centre Osteoarthritis Available from: https://www.hopkinsarthritis.org/arthritis-info/osteoarthritis/oa-differential-diagnosis/ (last accessed 29.5.2019)
- ↑ Kellgren JH. Atlas of standard radiographs of arthritis. Volume II of The Epidemiologic of Chronic Rheumatism. Oxford: Blackwell, 1963.
- ↑ De Groot IB, Reijman M, Terwee CB, Bierma-Zeinstra SM, Favejee M, Roos EM, Verhaar JA. Validation of the Dutch version of the Hip disability and Osteoarthritis Outcome Score. Osteoarthritis and cartilage 2007;15(1):104-9.