Neuropathic Pain: Difference between revisions
No edit summary |
No edit summary |
||
| Line 58: | Line 58: | ||
== Pathophysiology == | == Pathophysiology == | ||
Neuropathic pain is the result of disease or lesion of the somatosensory nervous system which results in altered and disordered transmission of sensory signals<ref name=":4" />. Changes in nerve function occur both at the site of the injury and areas around the injury<ref name=":1" />. Peripheral, spinal and central changes result in increases excitability and facilitation of signals, and a loss of inhibition<ref name=":4" />. With increasing chronicity, there is increased involvement of central changes. The pathophysiology is complex and still not fully understood. For more detail see the additional | Neuropathic pain is the result of disease or lesion of the somatosensory nervous system which results in altered and disordered transmission of sensory signals<ref name=":4" />. Changes in nerve function occur both at the site of the injury and areas around the injury<ref name=":1" />. Peripheral, spinal and central changes result in increases excitability and facilitation of signals, and a loss of inhibition<ref name=":4" />. With increasing chronicity, there is increased involvement of central changes. The pathophysiology is complex and still not fully understood. For more detail see the additional reference: <ref name=":6">Zusman M. Mechanisms of peripheral neuropathic pain: implications for musculoskeletal physiotherapy. Physical Therapy Reviews. 2008 Oct 1;13(5):313-23.</ref> | ||
{| class="wikitable" | {| class="wikitable" | ||
|+Pathophysiology in Neuropathic pain<ref name=":4" /><ref>Ochoa J, Torebjork HE. Paraesthesiae from ectopic impulse generation in human sensory nerves. Brain. 1980;103:835–854.</ref><ref name=":5">Finnerup NB, Kuner R, Jensen TS. [[Neuropathic pain: from mechanisms to treatment.]] Physiological reviews. 2020 Nov 3.</ref> | |+Pathophysiology in Neuropathic pain<ref name=":4" /><ref>Ochoa J, Torebjork HE. Paraesthesiae from ectopic impulse generation in human sensory nerves. Brain. 1980;103:835–854.</ref><ref name=":5">Finnerup NB, Kuner R, Jensen TS. [[Neuropathic pain: from mechanisms to treatment.]] Physiological reviews. 2020 Nov 3.</ref> | ||
| Line 108: | Line 108: | ||
'''History:''' Patients will often report spontaneous pain and sensations of ‘pins and needles,’ shooting, burning, stabbing, crawling, and paroxysmal pain (electric-shock like). These sensations affect not only the patient’s sensory system, but also the patient’s well-being, mood and focus. The onset of pain may be delayed, as is often the case in central post-stroke pain, or the phantom limb pain where neuropathic symptoms may start months or years after the primary event of injury. | '''History:''' Patients will often report spontaneous pain and sensations of ‘pins and needles,’ shooting, burning, stabbing, crawling, and paroxysmal pain (electric-shock like). These sensations affect not only the patient’s sensory system, but also the patient’s well-being, mood and focus. The onset of pain may be delayed, as is often the case in central post-stroke pain, or the phantom limb pain where neuropathic symptoms may start months or years after the primary event of injury. | ||
'''Clinical findings:''' There may be decreased reflexes, weakness and autonomic changes<ref name=":5" /> | '''Clinical findings:''' There may be decreased reflexes, weakness and autonomic changes<ref name=":5" />. Sensation testing will reveal abnormalities - if sensation is normal, it is highly likely that the pain experienced is of neuropathic origin. | ||
Neuropathic pain is often mixed with other pain mechanisms ([[Nociception|nociceptive]], [[Central Sensitisation|central sensitisation]]), which may result in a mixed clinical presentation. | Neuropathic pain is often mixed with other pain mechanisms ([[Nociception|nociceptive]], [[Central Sensitisation|central sensitisation]]), which may result in a mixed clinical presentation. | ||
| Line 156: | Line 156: | ||
=== Pharmacological Management === | === Pharmacological Management === | ||
A number of pharmacological treatments can be used to manage neuropathic pain outside of specialist pain management services. However, there is considerable variation in how treatment is initiated, the dosages used and the order in which drugs are introduced, whether therapeutic doses are achieved and whether there is correct sequencing of therapeutic classes. A further issue is that a number of commonly used treatments are unlicensed for treating neuropathic pain, which may limit their use. These factors may lead to inadequate pain control, with considerable morbidity. | A number of pharmacological treatments can be used to manage neuropathic pain outside of specialist pain management services. However, there is considerable variation in how treatment is initiated, the dosages used and the order in which drugs are introduced, whether therapeutic doses are achieved and whether there is correct sequencing of therapeutic classes. A further issue is that a number of commonly used treatments are unlicensed for treating neuropathic pain, which may limit their use. These factors may lead to inadequate pain control, with considerable morbidity. The goal of pharmacotherapy is to selectively block the production and/or transmission of pain-producing afferent activity in the periphery, and to engage mechanisms of endogenous inhibition in the CNS<ref name=":6" />. | ||
For commonly used pharmacological treatments see [[Neuropathic Pain Medication]] <ref name=":0" />. '''First line''' treatment generally includes: Tricyclic anti-depressants (TCAs), Serotonin-reuptake inhibitors (SNRIs), Pregabalin, Gabapentin<ref name=":4" />. Carbamazepine is however regarded as the first-line treatment for trigeminal neuralgia. | For commonly used pharmacological treatments see [[Neuropathic Pain Medication]] <ref name=":0" />. '''First line''' treatment generally includes: Tricyclic anti-depressants (TCAs), Serotonin-reuptake inhibitors (SNRIs), Pregabalin, Gabapentin<ref name=":4" />. Carbamazepine is however regarded as the first-line treatment for trigeminal neuralgia. | ||
| Line 192: | Line 192: | ||
== Resources == | == Resources == | ||
== References == | == References == | ||
<references /> | <references /> | ||
Revision as of 18:38, 19 August 2023
Original Editor - Kerstin McPherson
Top Contributors - Andeela Hafeez, Melissa Coetsee, Kerstin McPherson, Vanessa Rhule, Riccardo Ugrin, Lucinda hampton, Kim Jackson, Admin, Evan Thomas, Chrysolite Jyothi Kommu, WikiSysop, Vidya Acharya, Kapil Narale, Temitope Olowoyeye, Jo Etherton, Lauren Lopez, Amanda Ager, 127.0.0.1, Wendy Walker, Carina Therese Magtibay and Oyemi Sillo
Introduction[edit | edit source]
The International Association for the Study of Pain (2011) defines neuropathic pain as ‘pain caused by a lesion or disease of the somatosensory nervous system’. It is a complex, chronic pain state that presents a challenge to patients and clinicians.
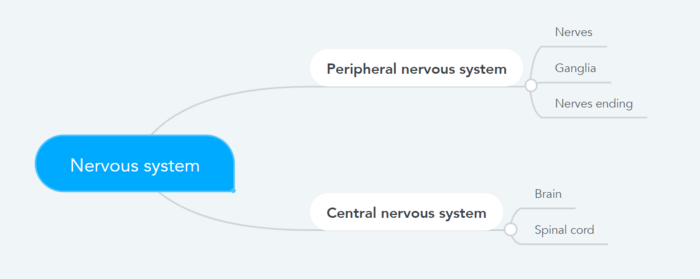
It is the result of disease or damage anywhere along the neuraxis of the peripheral or central (spinal and supraspinal) nervous system[1].
- Central neuropathic pain is defined as ‘pain caused by a lesion or disease of the central somatosensory nervous system’.
- Peripheral neuropathic pain is defined as ‘pain caused by a lesion or disease of the peripheral somatosensory nervous system’.
Neuropathic pain is very challenging to manage because of the heterogeneity of its aetiologies, symptoms, and underlying mechanisms[2].
Aetiology[edit | edit source]
Conditions frequently associated with neuropathic pain can be categorised into two major groups: pain due to damage in the central nervous system (CNS) and pain due to damage to the peripheral nervous system (PNS).
| CNS | PNS |
|---|---|
| Strokes: Cortical and subcortical | Nerve compression/ entrapment neuropathies (carpal tunnel syndrome, thoracic outlet syndrome, nerve root compression |
| Spinal cord injuries | Post-traumatic neuropathy (following surgical procedures or acute injury) |
| Syringomyelia and syringobulbia | Post-amputation stump and phantom limb pain |
| Trigeminal and glossopharyngeal neuralgias | Postherpetic neuralgia |
| Neoplastic and other space-occupying lesions | Disease related neuropathies: Diabetic neuropathy, cancer-related neuropathies and HIV-related neuropathy |
| Central pain in Multiple Sclerosis | Complex regional pain syndrome (CRPS) type 2 |
Also see Neuropathies
Epidemiology[edit | edit source]
The estimated prevalence of neuropathic pain is about 5%, but due to the difficulty in accurately diagnosing neuropathic pain, this number is likely an underestimation[3]. Neuropathic pain is not an inevitable consequence of neural lesion, and the progression from acute to chronic neuropathy occurs only in a minority and is influenced by a huge number of factors[4]
The following risk factors could predispose an individual to the development of neuropathic pain[3]:
- Age 50-64 years
- Being female
- Sociodemographic status: there is some evidence that unemployment and lower educational levels is associated with a higher incidence of neuropathic pain
- Injury sites: some anatomical sites are more prone to developing neuropathic pain
- Emotional and cognitive well-being: can influence how neuropathic pain is experienced
Pathophysiology[edit | edit source]
Neuropathic pain is the result of disease or lesion of the somatosensory nervous system which results in altered and disordered transmission of sensory signals[3]. Changes in nerve function occur both at the site of the injury and areas around the injury[1]. Peripheral, spinal and central changes result in increases excitability and facilitation of signals, and a loss of inhibition[3]. With increasing chronicity, there is increased involvement of central changes. The pathophysiology is complex and still not fully understood. For more detail see the additional reference: [5]
| Peripheral changes | Spinal cord changes | Cortical changes | |
|---|---|---|---|
| Spontaneous pain | Ectopic impulses along Aβ, Aδ, and C fibres of neuromas, nerve ends and nerve roots | Ectopic impulses at the dorsal root ganglia | Ectopic impulses at the thalamus |
| Sensitisation | Alterations in ion-channels: increased function of sodium channels leading to increased excitability, loss of potassium channels to modulate nerve activity | Increased expression and function of calcium channels leading to increased transmitter release and enhanced excitability of spinal neurons; expanded receptor fields through NMDA-receptor activation; A-fibre sprouting into laminae I and II of the dorsal horn, which can result in allodynia | Altered descending inhibition at the brain-stem (modulated by the cingulate cortex and amygdala); Limbic areas drive anxiety, depression and sleep problems; cortical reorganisation |
Central Sensitisation[edit | edit source]
The term central sensitisation (CS) is often incorrectly used synonymously with neuropathic pain. CS is however a mechanism that can occur independent of nerve lesions, but is often at play in chronic neuropathic pain. Central sensitisation is a state where spinal excitability increases due to repeated painful inputs[4]. CS results in decreased thresholds and increased response to nociceptive input
- Following a peripheral origin, central sensitisation may develop as a result of ectopic neuronal activity in the spinal cord dorsal horn, implying a potential autonomous pain-generating mechanism.[7] This leads to an increase in the size of the sensory receptive field, a reduced threshold for nociception, and hypersensitivity to various innocuous stimuli.
- First order neurons may increase their firing if they are partially damaged and increase the number of sodium channels.
- Ectopic discharges are a result of enhanced depolarization at certain sites in the fiber, leading to spontaneous pain and movement-related pain.
- Inhibitory circuits may be impaired at the level of the dorsal horn or brain stem (or both) allowing pain impulses to travel unopposed. See Pain Facilitation and Inhibition
- In addition, there may be alterations in the central processing of pain when. Second- and third-order neurons develop a “memory” of pain and become sensitized. There is then heightened sensitivity in spinal neurons and reduced activation thresholds. [2]
Abnormal Impulse Generating Sites (AIGS)[edit | edit source]
- Abnormal Impulse Generating Sites (AIGS) are defined as the unmyelinated sites along the damaged axon in which the number, kind and excitability of ion channels are altered. This change in ion channel distribution make the site susceptible to non-noxious stimuli such as mechanical, chemical, or thermal stimuli[8][9].
- The high density of ion channels may result in a resting potential close to the threshold, leading to spontaneous ectopic impulses.[10]
- AIGS fires antidromically and orthodromically, resulting in constant noxious stimulus into the central nervous system and neurogenic inflammation in the tissues. For this reason AIGS can persist even though the primary injury on the axon is completely healed.
- Where axons are disconnected from their distal targets (eg. amputation), inflammation and sprouting occur in the resulting and neuromas can form. A neuroma may become an anatomical site for generating nociceptive impulses.
- Together, neuromas, AIGS and dorsal root ganglion changes in receptors can be the peripheral nervous system cause of the phantom limb pain.[11]
Clinical Presentation[edit | edit source]
Neuropathic pain is typically characterised by pain that is associated with sensory symptoms/deficits. The coexistence of both positive and negative somatosensory signs is a key diagnostic feature[3]:
| Positive signs | Negative signs | |
|---|---|---|
| Features | Paraesthesia: crawling/tingling sensation; Spontaneous pain: burning, shooting, electric-like sensations; Hyperalgesia: increased sensitivity to noxious stimuli; Allodynia: pain in response to non-noxious stimuli (eg. light stroking); Summation: progressive worsening of pain with repetitive stimulation | Hyposthesia: sensory loss and numbness
Sensory loss is in the distribution of the damaged nerve or in the areas that correspond to the spinal/cortical region that has been damaged |
History: Patients will often report spontaneous pain and sensations of ‘pins and needles,’ shooting, burning, stabbing, crawling, and paroxysmal pain (electric-shock like). These sensations affect not only the patient’s sensory system, but also the patient’s well-being, mood and focus. The onset of pain may be delayed, as is often the case in central post-stroke pain, or the phantom limb pain where neuropathic symptoms may start months or years after the primary event of injury.
Clinical findings: There may be decreased reflexes, weakness and autonomic changes[4]. Sensation testing will reveal abnormalities - if sensation is normal, it is highly likely that the pain experienced is of neuropathic origin.
Neuropathic pain is often mixed with other pain mechanisms (nociceptive, central sensitisation), which may result in a mixed clinical presentation.
Diagnosis and Assessment[edit | edit source]
One of the challenges of neuropathic pain, is the ability to assess it. Assessing quality, intensity and improvement, as well as accurately diagnosing neuropathic pain is often complex.
There are, however, some diagnostic tools that may assist clinicians in evaluating neuropathic pain. eg nerve conduction studies and sensory-evoked potentials can identify and quantify the extent of damage to sensory (but not nociceptive) pathways by monitoring neurophysiological responses to electrical stimuli.
It is also very important to perform a thorough neurological evaluation to identify motor, sensory and autonomic dysfunctions.
| Possible NP | History of relevant neurological lesion or disease; pain distribution neuroanatomically plausible | History and pain and sensory descriptors are compatible with a lesion in the nervous system and not an inflammatory or non-neurological condition |
|---|---|---|
| Probable NP | Pain associated with sensory signs in the same neuroanatomically plausible distribution on clinical examination | The area of sensory changes may extend beyond, be within, or overlap the area of pain |
| Confirmed | Diagnostic test confirming a lesion or diseae of the somatosensory nervous system explaining the pain | Requires that other types of pain are excluded or highly unlikely to entirely explain the pain condition |
Quantitative Sensory Testing[edit | edit source]
QST is often time consuming and involved expensive equipment, which limits is application in clinical practice. There are however simplified bedside QST tests that can be useful to gain improved understanding related underlying pain mechanisms[3].
Mechanical sensitivity to tactile stimuli is measured with von Frey hairs, pinprick with weighted needles, vibration sensitivity with vibrometers and thermal pain with thermodes.
Outcome Measures[edit | edit source]
The following tools can be used to screen for neuropathic pain and to monitor neuropathic pain over time
- DN4 - a well validated screening tool to rank the probability that of peripheral or central neuropathic mechanisms are involved in chronic pain[3]
- LANSS
- PainDETECT
Management[edit | edit source]
Neuropathic pain often responds poorly to standard pain treatments and occasionally may get worse instead of better over time. For some people, it can lead to significant disability. Since the cause of neuropathic pain can often not be treated, the focus of its management is on alleviating the symptoms which requires an multidisciplinary approach that combines therapies:
- Medical management and the use of pharmacological agents
- Physiotherapy
- Low impact general physical activities
- Counselling
- Relaxation therapy
- Massage therapy
- Acupuncture
Pharmacological Management[edit | edit source]
A number of pharmacological treatments can be used to manage neuropathic pain outside of specialist pain management services. However, there is considerable variation in how treatment is initiated, the dosages used and the order in which drugs are introduced, whether therapeutic doses are achieved and whether there is correct sequencing of therapeutic classes. A further issue is that a number of commonly used treatments are unlicensed for treating neuropathic pain, which may limit their use. These factors may lead to inadequate pain control, with considerable morbidity. The goal of pharmacotherapy is to selectively block the production and/or transmission of pain-producing afferent activity in the periphery, and to engage mechanisms of endogenous inhibition in the CNS[5].
For commonly used pharmacological treatments see Neuropathic Pain Medication [2]. First line treatment generally includes: Tricyclic anti-depressants (TCAs), Serotonin-reuptake inhibitors (SNRIs), Pregabalin, Gabapentin[3]. Carbamazepine is however regarded as the first-line treatment for trigeminal neuralgia.
It is very important to identify concomitant underlying pain mechanisms, as this could improve the effectiveness of pharmacological management by targeting additional mechanisms with different analgesic agents[3].
Other Medical Interventions[edit | edit source]
For some individuals with refractory neuropathic pain, interventional treatments—which deliver medications to specific regions or modify particular brain structures—offer alternative therapy options.
Some of the interventional treatments include:
- Spinal cord stimulation: Requires the application of a monophasic square-wave pulse (at a frequency in the 30–100 Hz range) that results in paraesthesia of the painful part[12][13]
- Cortical stimulation: Using either invasive epidural or transcranial non-invasive procedures (such repetitive transcranial magnetic stimulation (TMS) and transcranial direct current stimulation), cortical stimulation entails stimulating the pre-central motor cortex below the motor threshold.
- Deep brain stimulation: The internal capsule, various nuclei in the sensory thalamus, periaqueductal and periventricular grey, motor cortex, septum, nucleus accumbens, posterior hypothalamus, and anterior cingulate cortex are potential targets for pain relief in deep brain stimulation.
- Intrathecal treatments: In individuals with persistent pain that is severe and otherwise resistant to treatment, this offers a targeted drug delivery option to the painful part.[12]
Physical Therapy Management[edit | edit source]
Physical therapy modalities and rehabilitation techniques are important options and must be considered when pharmacotherapy alone is not sufficient [14].Physical therapy tackles the physical side of the inflammation, stiffness, and soreness with exercise, manipulation, and massage, but it also works to help the body heal itself by encouraging the production of the body's natural pain-relieving chemicals. This two-pronged approach is what helps make physical therapy so effective as a pain treatment.[15]
In addiction to that, exercise is useful to reorganise and sprouting the cortical body representation: the profound change in the neuromatrix related to chronic pain it is part of the central sensitisation [16][17].
- TENS therapy has low quality of evidence for been effective in the treatment of painful peripheral neuropathy. Low level laser therapy could otherwise has positive effects on the control of analgesia for neuropathic pain [18][19].
- Neurostimulation techniques including transcranial magnetic stimulation (TMS) and cortical electrical stimulation (CES), spinal cord stimulation (SCS) and deep brain stimulation (DBS) have also been found effective in the treatment of neuropathic pain.
- Exercise and movement representation techniques (that is, treatments such as mirror therapy and motor imagery that use the observation and/or imagination of normal pain-free movements) have been suggested to be beneficial in neuropathic pain management. Recently, mirror therapy has used for not only patients with phantom limb pain, but also for patients with complex regional pain syndrome and strokes[20]. However the quality of evidence supporting these interventions for neuropathic pain is weak and needs further investigation.
- Exercise: exercising for just 30 minutes a day on at least three or four days a week will help you with chronic pain management by increasing:[15]Muscle Strength; Endurance; Stability in the joints; Flexibility in the muscles and joints. Keeping a consistent exercise routine will also help control pain. Regular therapeutic exercise will help you maintain the ability to move and function physically, rather than becoming disabled by your chronic pain.
- There are studies showing that exercise may be an important part of the treatment and prevention of neuropathic pain after chemotherapy. Although more information is required and detailed exercise prescriptions do not yet exist for patients receiving cancer treatment.[21] It has been also found that physical exercise, such as forced treadmill running and swimming, can sufficiently improve mechanical allodynia and heat hyperalgesia in animal models of neuropathic pain. [22]
Please watch the following video for relevant about neuropathic pain.
Management of Neuropathic Pain[23]
Resources[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 PPM The Pathophysiology of Neuropathic Pain Available:https://www.practicalpainmanagement.com/pain/neuropathic/pathophysiology-neuropathic-pain (accessed 30.10.2021)
- ↑ 2.0 2.1 2.2 NICE. Neuropathic pain in adults: pharmacological management in non-specialist settings.Available: https://www.ncbi.nlm.nih.gov/books/NBK552848/(accessed 30.9.2021)
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 3.9 Bannister K, Sachau J, Baron R, Dickenson AH. Neuropathic pain: mechanism-based therapeutics. Annual Review of Pharmacology and Toxicology. 2020 Jan 6;60:257-74.
- ↑ 4.0 4.1 4.2 4.3 4.4 Finnerup NB, Kuner R, Jensen TS. Neuropathic pain: from mechanisms to treatment. Physiological reviews. 2020 Nov 3.
- ↑ 5.0 5.1 Zusman M. Mechanisms of peripheral neuropathic pain: implications for musculoskeletal physiotherapy. Physical Therapy Reviews. 2008 Oct 1;13(5):313-23.
- ↑ Ochoa J, Torebjork HE. Paraesthesiae from ectopic impulse generation in human sensory nerves. Brain. 1980;103:835–854.
- ↑ Haroutounian S, Nikolajsen L, Bendtsen TF, Finnerup NB, Kristensen AD, Hasselstrøm JB, Jensen TS . Primary afferent input critical for maintaining spontaneous pain in peripheral neuropathy. Pain, 2014; 155 (7): 1272-9
- ↑ Greening J, Lynn B. Minor peripheral nerve injuries an underestimated source of pain? Manual Therapy, 1998; 3: 187-194
- ↑ Gifford L. Acute low cervical nerve root conditions: symptom presentation and pathobiological reasoning. Manual Therapy, 2001; 6: 106-115
- ↑ Sapunar D, Kostic S, Banozic A, Puljak L. Dorsal root ganglion — a potential new therapeutic target for neuropathic pain. J Pain Res. 2012;5:31–38
- ↑ Collins KL, Russell HG, Schumacher PJ, et al. A review of current theories and treatments for phantom limb pain. J Clin Invest. 2018;128(6):2168-2176.
- ↑ 12.0 12.1 Colloca L, Ludman T, Bouhassira D, Baron R, Dickenson AH, Yarnitsky D, Freeman R, Truini A, Attal N, Finnerup NB, Eccleston C. Neuropathic pain. Nature reviews Disease primers. 2017 Feb 16;3(1):1-9.
- ↑ Dones I, Levi V. Spinal cord stimulation for neuropathic pain: current trends and future applications. Brain sciences. 2018 Jul 24;8(8):138.
- ↑ Akyuz G, Kenis O. Physical therapy modalities and rehabilitation techniques in the management of neuropathic pain. Am J Phys Med Rehabil. 2014 Mar;93(3):253-9.
- ↑ 15.0 15.1 Physical Therapy for Pain Management.By Diana Rodriguez | Medically reviewed by Pat F. Bass III, MD, MPH
- ↑ Melzack R. Pain and the neuromatrix in the brain. J Dent Educ. 2001 Dec;65(12):1378-82.
- ↑ Trout KK. The neuromatrix theory of pain: implications for selected nonpharmacologic methods of pain relief for labor. J Midwifery Womens Health. 2004 Nov-Dec;49(6):482-8.
- ↑ Gibson W, Wand BM, O'Connell NE. Transcutaneous electrical nerve stimulation (TENS) for neuropathic pain in adults. Cochrane Database Syst Rev. 2017 Sep 14;9(9):CD011976
- ↑ de Andrade AL, Bossini PS, Parizotto NA. Use of low level laser therapy to control neuropathic pain: A systematic review. J Photochem Photobiol B. 2016 Nov;164:36-42.
- ↑ Kim SY, Kim YY. Mirror therapy for phantom limb pain. Korean J Pain. 2012;25(4):272-274.
- ↑ Majithia N, Loprinzi CL, Smith TJ.New Practical Approaches to Chemotherapy-Induced Neuropathic Pain: Prevention, Assessment, and Treatment. Oncology (Williston Park). 2016 Nov 15;30(11)
- ↑ Kami K, Tajima F, Senba E. Exercise-induced hypoalgesia: potential mechanisms in animal models of neuropathic pain. Anat Sci Int. 2016 Aug 2. [Epub ahead of print]
- ↑ Management of Neuropathic Pain. Available from: https://www.youtube.com/watch?v=hDu_WdRNDzo&t=796s










