Muscle Spindles: Difference between revisions
No edit summary |
Ahmed M Diab (talk | contribs) m (Ahmed M Diab moved page Muscle spindles to Muscle Spindles: Corrected title) |
||
| (33 intermediate revisions by 9 users not shown) | |||
| Line 4: | Line 4: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
[[File:MuscleSpindle.png| | == Definition == | ||
[[File:303px-MuscleSpindle.svg.png|alt=|right|frameless]]Almost every muscle contains muscle spindles. These delicate sensory receptors inform the [[Introduction to Neuroanatomy|central nervous system]] (CNS) about changes in the length of individual [[Muscle|muscles]] and the speed of [[stretching]]. With this information, the CNS computes the position and movement of our extremities in space, which is a requirement for [[Motor Control and Learning|motor control]], for maintaining [[posture]] and for a stable [[gait]]. The responses of muscle spindles to changes in length also play an important role in regulating the contraction of muscles, by activating motor neurons via the stretch reflex to resist muscle stretch<ref name="idiopathic">Kröger S, Watkins B. Muscle spindle function in healthy and diseased muscle. Skeletal muscle. 2021 Dec;11(1):1-3. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7788844/]</ref><ref name="senses">Proske U, Gandevia SC. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2754351/ The kinaesthetic senses]. The Journal of physiology. 2009 Sep 1;587(17):4139-46.</ref>. | |||
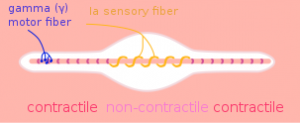
Image 1: Muscle Spindle (located in muscle belly) | |||
* Many [[Neuromuscular Disorders|neuromuscular diseases]] affect muscle spindle function contributing, among others, to an unstable gait, frequent [[falls]] and [[Ataxia|ataxic]] behavior in the affected patients.<ref name=":2">Kröger S, Watkins B. [https://skeletalmusclejournal.biomedcentral.com/articles/10.1186/s13395-020-00258-x Muscle spindle function in healthy and diseased muscle.] Skeletal Muscle. 2021 Dec;11(1):1-3. | |||
</ref> | |||
== | =='''Role in Proprioception'''== | ||
[[File: | [[File:Balance-board-benefits.jpg|right|frameless]] | ||
Although Golgi tendon organs, joint receptors and other [[Sensation|sensory systems]] also contribute to [[proprioception]], muscle spindles are the most important proprioceptors. | |||
* Muscle spindles are the most frequently found sense organs in skeletal [[Muscle Cells (Myocyte)|muscles]] and present in almost every muscle. | |||
* The density of muscle spindles within the large muscle mass, however, is low so that they are rather difficult to detect. Rough estimates have suggested approximately 50,000 muscle spindles in the entire human body (interestingly, in humans, muscle spindles are mostly absent in facial muscles).<ref name=":2" /> | |||
Two important proprioceptors that play a role in flexibility are the muscle spindle and the golgi tendon organ (GTO), together reflexively work to regulate muscle stiffness. | |||
The function of the GTO can be considered opposite of the muscle spindle, which serves to produce muscle contraction. When a GTO is stimulated, it causes its associated muscle to relax by interrupting its contraction.<ref name=":3">Golgi Tendon Organs and Muscle Spindles Explained. Available from:https://www.acefitness.org/fitness-certifications/ace-answers/exam-preparation-blog/5336/golgi-tendon-organs-and-muscle-spindles-explained/ (Accessed, 17.5.2021).</ref> | |||
== | == Composition == | ||
[[File:Spindle- comp.jpg|A mammalian muscle spindle showing typical position in a muscle (left), neuronal connections in spinal cord (middle) and expanded schematic (right).|alt=|right|frameless|429x429px]]Muscle spindles are small sensory organs with an elongated shape, involved in proprioception. | |||
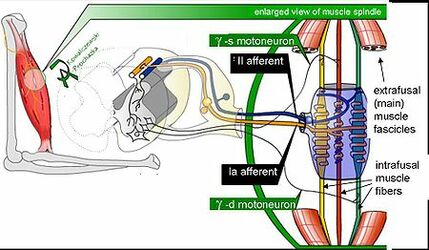
Image 2: Mammalian muscle spindle showing typical position in a muscle (left), neuronal connections in [[Spinal cord anatomy|spinal cord]] (middle) and expanded schematic (right). The spindle is a stretch receptor with its own motor supply consisting of several intrafusal muscle fibres. The sensory endings of a primary (group Ia) afferent and a secondary (group II) afferent coil around the non-contractile central portions of the intrafusal fibres. Gamma motor neurons activate the intrafusal muscle fibres, changing the resting firing rate and stretch-sensitivity of the afferents. | |||
* Consist of several modified muscle fibers enclosed in a sheath of [[Connective Tissue Disorders|connective tissue]]<ref name=":0" />. | |||
* The modified fibers are called intrafusal fibers. These fibers are oriented parallel to the regular, power-producing extrafusal muscle fibers. | |||
* Multiply innervated and named according to the arrangement of their nuclei as nuclear bag or nuclear chain fibers. | |||
* Intrafusal muscle fibers are up to 8-mm long in humans. Each muscle spindle contains on average 8–20 (human) intrafusal fibers. With a diameter of 8 to 25 μm [30], intrafusal muscle fibers are much thinner than extrafusal muscle fibers<ref name=":2" /> | |||
== Function == | |||
[[File:Reflex.jpg|right|frameless|532x532px]] | |||
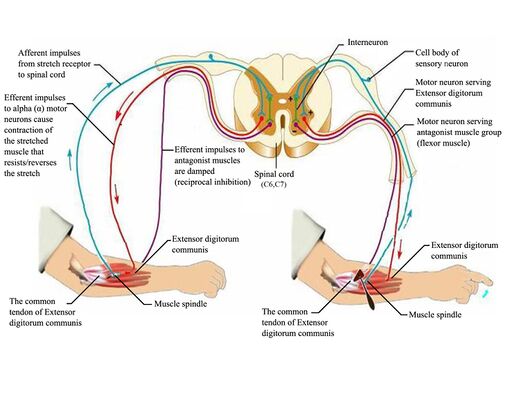
Imagine a muscle spindle as if it were a thread spiraled (or wrapped around) muscle fibers near the muscle belly; as the muscle lengthens or stretches, it pulls on the spindle causing it to lose its spiral shape and also stretch. This signals the muscle to contract (after which, the spiral regains its shape), in turn protecting the muscle from being overstretched. This process is called the stretch [[Reflexes|reflex]]. | |||
When a muscle spindle’s associated muscle is rapidly stretched, the spindle can cause two things to happen: | |||
* Functionally, muscle spindles are stretch detectors, and sense how much and how fast a muscle is lengthened or shortened. Accordingly, when a muscle is stretched, this change in length is transmitted to the spindles and their intrafusal fibers which are subsequently similarly stretched <ref name=":2" />. | |||
* It may signal its muscle to contract to prevent it from going too far, too quickly in the stretch. The stimulation of a reflexive muscle contraction is known as the stretch or myotatic [[Reflexes|reflex]] <ref name="idiopathic" />. | |||
* It can inhibit the opposing muscle, ie the antagonist to the muscle being stretched, to prevent it from contracting so that it can’t contribute to any further stretching (ie [[Stretching|reciprocal inhibition]]) . | |||
* In humans, the sensory innervation of the muscle spindle arises from both group Ia and group II afferent fibers which differ in their axonal conduction velocity. The sensory terminals form irregular coils with branches and varicose swellings. | |||
* The cell bodies of these proprioceptive afferent fibers constitute 5–10% of all neurons in the dorsal root ganglion <ref name=":2" /> . | |||
Ultimately, the muscle spindle functions to alert the brain that nearby joints and soft tissues are in danger of being stretched too far. These are important concepts in understanding body awareness (also known as proprioception and kinesthetic awareness)<ref name=":3" />. | |||
Spindles thus indicate the degree to which the muscle must be activated in order to overcome a given resistance. As a load increases, the muscle is stretched to a greater extent, and engagement of muscle spindles results in greater activation of the muscle. Muscles that perform precise movements have many spindles per unit of mass to help ensure exact control of their contractile activity<ref name=":0" />. | Spindles thus indicate the degree to which the muscle must be activated in order to overcome a given resistance. As a load increases, the muscle is stretched to a greater extent, and engagement of muscle spindles results in greater activation of the muscle. Muscles that perform precise movements have many spindles per unit of mass to help ensure exact control of their contractile activity<ref name=":0" />. | ||
{{#ev:youtube|442UbX9qeLk |300}}<ref > Animated Anatomy. Muscle Spindle - Muscle Stretch Reflex. Available from: https://www.youtube.com/watch?v=442UbX9qeLk [Accessed, 08/10/2021] </ref> | |||
'''Example''' | |||
A simple example of muscle spindle activity is the knee jerk reflex (Patellar reflex), sudden kicking movement of the lower leg in response to a sharp tap on the patellar tendon, which lies just below the kneecap<ref name=":0">Brukner P. Brukner & Khan's clinical sports medicine. North Ryde: McGraw-Hill; 2012.</ref>. Tapping on the tendon of the [[Quadriceps Muscle|knee extensor muscle group]] below the [[patella]] stretches the muscle spindle fibers. This causes activation of extrafusal muscle fibers in the same muscle. A knee jerk occurs as these fibers actively shorten. This, in turn, shortens the intrafusal fibers and causes their discharge to cease<ref name=":0" />. | |||
See [[Reflexes]] | |||
== Dysfunctions in the Muscle Spindle == | |||
Problems may arise in the functioning of the muscle spindle. An upper motor neuron lesion can lead to a loss of supraspinal inhibition. A basal ganglia disorder can cause excessive supraspinal activation<ref name=":1">https://kin450-neurophysiology.wikispaces.com/Muscle+Spindle</ref>. If there is a problem with the muscles spindle it may present as abnormal muscle tone such as spasticity (a velocity dependent increase in resistance to passive stretch which causes exaggerated tendon reflexes called hypereflexia)<ref>Young RR. [https://europepmc.org/article/med/7970006 Spasticity: a review]. Neurology. 1994 Nov;44(11 Suppl 9):S12-20. | |||
</ref>. There are several causes of spasticity associated with the muscle spindle: | |||
* Overactive input from gamma motor neurons or increased excitability at the central synapse can present as spasticity. This usually occurs due to cortical damage and a loss of inhibitory impulses. | |||
* Spasticity may be caused by problems with the renshaw cells. Renshaw cells are interneurons that are stimulated by the alpha motor neuron and then, by a feedback mechanism, inhibit the alpha motor neuron, causing autoinhibition.<ref>Thomas RC, Wilson VJ. [https://www.nature.com/articles/206211b0 Precise localization of Renshaw cells with a new marking technique.] Nature. 1965 Apr 10;206(4980):211-3.</ref> Problems with the renshaw cells lead to a loss of inhibition on the alpha motor neurons so they simply continue firing. | |||
* Spasticity can arise because of the loss of appropriate pre-synaptic inhibition of Ia afferent.<ref>Mukherjee A, Chakravarty A. [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3009478/ Spasticity mechanisms–for the clinician.] Frontiers in neurology. 2010;1.</ref> | |||
* It can also arise from a neuro-related or structural change in the muscle fibers.<ref name=":1" /> | |||
It is often believed that dysfunction caused by [[Stroke|strokes]] and [https://physio-pedia.com/Parkinson's_Disease_-_Clinical_Presentation movement disorders], such as [[Muscle Disorders|muscular dystrophy]], also affect the function of muscle spindles. For example, strokes are known to cause weakness, loss of dexterity, and exaggerated reflex response to proprioceptive and cutaneous stimuli due to problems with the gamma motor system. However, current research shows that the gamma motor system is not responsible for the deficits of the skeletal-motor system. The discharge rate of muscle spindles in stroke patients was found to be similar to normal subjects. There was no difference in the reflex response to peripheral afferent inputs or in the response to supraspinal drive<ref>Wilson LR, Gandevia SC, Inglis JT, Gracies JM, Burke D. [https://doi.org/10.1093/brain/122.11.2079 Muscle spindle activity in the affected upper limb after a unilateral stroke]. Brain. 1999 Nov 1;122(11):2079-88.</ref>. | |||
On the structural level, muscle spindles in [[Older People Introduction|aged humans]] possess fewer intrafusal fibers, an increased capsular thickness and some spindles which show signs of denervation. Together with the proprioceptive system in general and with ageing, significant structural and functional changes occur and the changes are consistent with a gradual decline in proprioceptive function in elderly individuals and animals. These changes might contribute to the frequent falls and motor control problems observed in older adults <ref name=":2" />. | |||
[ | An impaired proprioception, in some cases associated with an altered muscle spindle morphology, has been documented as a secondary effect in many diseases. In any neuromuscular disease, therapeutic strategies should therefore also aim at restoring/maintaining proprioception and muscle spindle function.<ref name=":2" /> For example, [[Muscular Dystrophy|Muscular dystrophy]] is characterized by the degeneration of skeletal muscle fibers. Research examining the effect of the degeneration on intrafusal fibers have found that the proprioceptive function of muscle spindles is spared in muscular dystrophy. Research confirmed that muscular dystrophy patients perceived passive movements and experienced illusory movements similar to those perceived by healthy subjects in terms of the movement direction and velocity. They also found that muscular dystrophy patients were able to respond with similar spatial and temporal movement characteristics when compared with the normal subjects<ref>Ribot‐Ciscar E, Tréfouret S, Aimonetti JM, Attarian S, Pouget J, Roll JP. [https://doi.org/10.1002/mus.20044 Is muscle spindle proprioceptive function spared in muscular dystrophies? A muscle tendon vibration study.] Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 2004 Jun;29(6):861-6.</ref>. Common therapeutic interventions for patients with muscular dystrophy should aim at increasing muscle strength and reducing muscle fatigue and degeneration. Moreover, therapeutic strategies should also aim at restoring/maintaining proprioception and muscle spindle function in any neuromuscular disease <ref name=":2" />. | ||
== References == | == References == | ||
<references /><br> | <references /><br> | ||
[[Category:Muscles]] | |||
[[Category:Muscles]] [[Category:Anatomy]] [[Category:Neurology]] [[Category: | [[Category:Anatomy]] | ||
[[Category:Neurology]] | |||
[[Category:Cerebral Palsy]] | |||
[[Category:Musculoskeletal/Orthopaedics]] | |||
[[Category:Sports Medicine]] | |||
Latest revision as of 12:46, 3 June 2023
Original Editor - Bo Hellinckx
Top Contributors - Tania Appelmans, Adam Vallely Farrell, Kirenga Bamurange Liliane, Lucinda hampton, Laura Ritchie, Vidya Acharya, Oyemi Sillo, Bo Hellinckx, Scott Buxton, Cindy John-Chu, Ahmed M Diab, Rachael Lowe, Evan Thomas, WikiSysop, Kim Jackson and Wanda van Niekerk
Definition[edit | edit source]
Almost every muscle contains muscle spindles. These delicate sensory receptors inform the central nervous system (CNS) about changes in the length of individual muscles and the speed of stretching. With this information, the CNS computes the position and movement of our extremities in space, which is a requirement for motor control, for maintaining posture and for a stable gait. The responses of muscle spindles to changes in length also play an important role in regulating the contraction of muscles, by activating motor neurons via the stretch reflex to resist muscle stretch[1][2].
Image 1: Muscle Spindle (located in muscle belly)
- Many neuromuscular diseases affect muscle spindle function contributing, among others, to an unstable gait, frequent falls and ataxic behavior in the affected patients.[3]
Role in Proprioception[edit | edit source]
Although Golgi tendon organs, joint receptors and other sensory systems also contribute to proprioception, muscle spindles are the most important proprioceptors.
- Muscle spindles are the most frequently found sense organs in skeletal muscles and present in almost every muscle.
- The density of muscle spindles within the large muscle mass, however, is low so that they are rather difficult to detect. Rough estimates have suggested approximately 50,000 muscle spindles in the entire human body (interestingly, in humans, muscle spindles are mostly absent in facial muscles).[3]
Two important proprioceptors that play a role in flexibility are the muscle spindle and the golgi tendon organ (GTO), together reflexively work to regulate muscle stiffness.
The function of the GTO can be considered opposite of the muscle spindle, which serves to produce muscle contraction. When a GTO is stimulated, it causes its associated muscle to relax by interrupting its contraction.[4]
Composition[edit | edit source]
Muscle spindles are small sensory organs with an elongated shape, involved in proprioception.
Image 2: Mammalian muscle spindle showing typical position in a muscle (left), neuronal connections in spinal cord (middle) and expanded schematic (right). The spindle is a stretch receptor with its own motor supply consisting of several intrafusal muscle fibres. The sensory endings of a primary (group Ia) afferent and a secondary (group II) afferent coil around the non-contractile central portions of the intrafusal fibres. Gamma motor neurons activate the intrafusal muscle fibres, changing the resting firing rate and stretch-sensitivity of the afferents.
- Consist of several modified muscle fibers enclosed in a sheath of connective tissue[5].
- The modified fibers are called intrafusal fibers. These fibers are oriented parallel to the regular, power-producing extrafusal muscle fibers.
- Multiply innervated and named according to the arrangement of their nuclei as nuclear bag or nuclear chain fibers.
- Intrafusal muscle fibers are up to 8-mm long in humans. Each muscle spindle contains on average 8–20 (human) intrafusal fibers. With a diameter of 8 to 25 μm [30], intrafusal muscle fibers are much thinner than extrafusal muscle fibers[3]
Function[edit | edit source]
Imagine a muscle spindle as if it were a thread spiraled (or wrapped around) muscle fibers near the muscle belly; as the muscle lengthens or stretches, it pulls on the spindle causing it to lose its spiral shape and also stretch. This signals the muscle to contract (after which, the spiral regains its shape), in turn protecting the muscle from being overstretched. This process is called the stretch reflex.
When a muscle spindle’s associated muscle is rapidly stretched, the spindle can cause two things to happen:
- Functionally, muscle spindles are stretch detectors, and sense how much and how fast a muscle is lengthened or shortened. Accordingly, when a muscle is stretched, this change in length is transmitted to the spindles and their intrafusal fibers which are subsequently similarly stretched [3].
- It may signal its muscle to contract to prevent it from going too far, too quickly in the stretch. The stimulation of a reflexive muscle contraction is known as the stretch or myotatic reflex [1].
- It can inhibit the opposing muscle, ie the antagonist to the muscle being stretched, to prevent it from contracting so that it can’t contribute to any further stretching (ie reciprocal inhibition) .
- In humans, the sensory innervation of the muscle spindle arises from both group Ia and group II afferent fibers which differ in their axonal conduction velocity. The sensory terminals form irregular coils with branches and varicose swellings.
- The cell bodies of these proprioceptive afferent fibers constitute 5–10% of all neurons in the dorsal root ganglion [3] .
Ultimately, the muscle spindle functions to alert the brain that nearby joints and soft tissues are in danger of being stretched too far. These are important concepts in understanding body awareness (also known as proprioception and kinesthetic awareness)[4].
Spindles thus indicate the degree to which the muscle must be activated in order to overcome a given resistance. As a load increases, the muscle is stretched to a greater extent, and engagement of muscle spindles results in greater activation of the muscle. Muscles that perform precise movements have many spindles per unit of mass to help ensure exact control of their contractile activity[5].
Example
A simple example of muscle spindle activity is the knee jerk reflex (Patellar reflex), sudden kicking movement of the lower leg in response to a sharp tap on the patellar tendon, which lies just below the kneecap[5]. Tapping on the tendon of the knee extensor muscle group below the patella stretches the muscle spindle fibers. This causes activation of extrafusal muscle fibers in the same muscle. A knee jerk occurs as these fibers actively shorten. This, in turn, shortens the intrafusal fibers and causes their discharge to cease[5].
See Reflexes
Dysfunctions in the Muscle Spindle[edit | edit source]
Problems may arise in the functioning of the muscle spindle. An upper motor neuron lesion can lead to a loss of supraspinal inhibition. A basal ganglia disorder can cause excessive supraspinal activation[7]. If there is a problem with the muscles spindle it may present as abnormal muscle tone such as spasticity (a velocity dependent increase in resistance to passive stretch which causes exaggerated tendon reflexes called hypereflexia)[8]. There are several causes of spasticity associated with the muscle spindle:
- Overactive input from gamma motor neurons or increased excitability at the central synapse can present as spasticity. This usually occurs due to cortical damage and a loss of inhibitory impulses.
- Spasticity may be caused by problems with the renshaw cells. Renshaw cells are interneurons that are stimulated by the alpha motor neuron and then, by a feedback mechanism, inhibit the alpha motor neuron, causing autoinhibition.[9] Problems with the renshaw cells lead to a loss of inhibition on the alpha motor neurons so they simply continue firing.
- Spasticity can arise because of the loss of appropriate pre-synaptic inhibition of Ia afferent.[10]
- It can also arise from a neuro-related or structural change in the muscle fibers.[7]
It is often believed that dysfunction caused by strokes and movement disorders, such as muscular dystrophy, also affect the function of muscle spindles. For example, strokes are known to cause weakness, loss of dexterity, and exaggerated reflex response to proprioceptive and cutaneous stimuli due to problems with the gamma motor system. However, current research shows that the gamma motor system is not responsible for the deficits of the skeletal-motor system. The discharge rate of muscle spindles in stroke patients was found to be similar to normal subjects. There was no difference in the reflex response to peripheral afferent inputs or in the response to supraspinal drive[11].
On the structural level, muscle spindles in aged humans possess fewer intrafusal fibers, an increased capsular thickness and some spindles which show signs of denervation. Together with the proprioceptive system in general and with ageing, significant structural and functional changes occur and the changes are consistent with a gradual decline in proprioceptive function in elderly individuals and animals. These changes might contribute to the frequent falls and motor control problems observed in older adults [3].
An impaired proprioception, in some cases associated with an altered muscle spindle morphology, has been documented as a secondary effect in many diseases. In any neuromuscular disease, therapeutic strategies should therefore also aim at restoring/maintaining proprioception and muscle spindle function.[3] For example, Muscular dystrophy is characterized by the degeneration of skeletal muscle fibers. Research examining the effect of the degeneration on intrafusal fibers have found that the proprioceptive function of muscle spindles is spared in muscular dystrophy. Research confirmed that muscular dystrophy patients perceived passive movements and experienced illusory movements similar to those perceived by healthy subjects in terms of the movement direction and velocity. They also found that muscular dystrophy patients were able to respond with similar spatial and temporal movement characteristics when compared with the normal subjects[12]. Common therapeutic interventions for patients with muscular dystrophy should aim at increasing muscle strength and reducing muscle fatigue and degeneration. Moreover, therapeutic strategies should also aim at restoring/maintaining proprioception and muscle spindle function in any neuromuscular disease [3].
References[edit | edit source]
- ↑ 1.0 1.1 Kröger S, Watkins B. Muscle spindle function in healthy and diseased muscle. Skeletal muscle. 2021 Dec;11(1):1-3. [1]
- ↑ Proske U, Gandevia SC. The kinaesthetic senses. The Journal of physiology. 2009 Sep 1;587(17):4139-46.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Kröger S, Watkins B. Muscle spindle function in healthy and diseased muscle. Skeletal Muscle. 2021 Dec;11(1):1-3.
- ↑ 4.0 4.1 Golgi Tendon Organs and Muscle Spindles Explained. Available from:https://www.acefitness.org/fitness-certifications/ace-answers/exam-preparation-blog/5336/golgi-tendon-organs-and-muscle-spindles-explained/ (Accessed, 17.5.2021).
- ↑ 5.0 5.1 5.2 5.3 Brukner P. Brukner & Khan's clinical sports medicine. North Ryde: McGraw-Hill; 2012.
- ↑ Animated Anatomy. Muscle Spindle - Muscle Stretch Reflex. Available from: https://www.youtube.com/watch?v=442UbX9qeLk [Accessed, 08/10/2021]
- ↑ 7.0 7.1 https://kin450-neurophysiology.wikispaces.com/Muscle+Spindle
- ↑ Young RR. Spasticity: a review. Neurology. 1994 Nov;44(11 Suppl 9):S12-20.
- ↑ Thomas RC, Wilson VJ. Precise localization of Renshaw cells with a new marking technique. Nature. 1965 Apr 10;206(4980):211-3.
- ↑ Mukherjee A, Chakravarty A. Spasticity mechanisms–for the clinician. Frontiers in neurology. 2010;1.
- ↑ Wilson LR, Gandevia SC, Inglis JT, Gracies JM, Burke D. Muscle spindle activity in the affected upper limb after a unilateral stroke. Brain. 1999 Nov 1;122(11):2079-88.
- ↑ Ribot‐Ciscar E, Tréfouret S, Aimonetti JM, Attarian S, Pouget J, Roll JP. Is muscle spindle proprioceptive function spared in muscular dystrophies? A muscle tendon vibration study. Muscle & Nerve: Official Journal of the American Association of Electrodiagnostic Medicine. 2004 Jun;29(6):861-6.