Morton's Toe: Difference between revisions
No edit summary |
Kim Jackson (talk | contribs) m (Text replacement - "[[Orthotics" to "[[Introduction to Orthotics") |
||
| (44 intermediate revisions by 8 users not shown) | |||
| Line 1: | Line 1: | ||
= | <div class="editorbox"> | ||
'''Original Editor '''- [[User:Marlies Verbruggen|Marlies Verbruggen]] | |||
'''Top Contributors '''-{{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | |||
<br> | |||
== | == Introduction == | ||
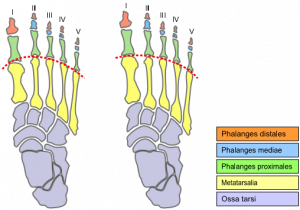
[[Image:Morton's foot comparison.png|thumb|right|Vector-generated image comparing a foot with (left) and without (right) Morton's toe. The dotted curve indicates the joint position.]]A Morton’s toe otherwise called Morton's foot or Greek foot or Royal toe is characterized by a longer second toe. This is because the first metatarsal, behind the big toe, is short compared to the second metatarsal, next to it. The longer second metatarsal puts the joint at the base of the second toe (the second metatarsophalangeal or MTP joint) further forward. It is a type of brachymetatarsia.<ref name="brage">Schimizzi, A; Brage, M (September 2004). "Brachymetatarsia". ''Foot Ankle Clin'' '''9''' (3): 555–70, doi:10.1016/j.fcl.2004.05.002. PMID 15324790.</ref> | |||
Brachymetatarsia is a condition in which the metatarsal physis closes prematurely yielding a pathologically shortened metatarsal length. It can affect any of the five metatarsal bones of the foot and it could be bilateral. Brachymetatarsia of the first metatarsal is also known as “Morton’s syndrome or Toe”<ref name=":1" /> | |||
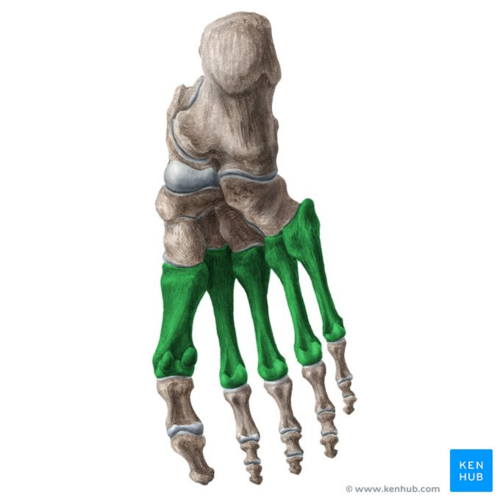
[[File:Metatarsal bones - Kenhub.png|alt=Metatarsal bones of the foot (highlighted in green) - inferior view|right|frameless|500x500px|Metatarsal bones of the foot (highlighted in green) - inferior view]] | |||
Morton's toe is a little misleading, because this condition is not really a long toe, meaning the phalanges (toe bones). It is the relative length of the metatarsal foot bones, specifically the relative length difference between the first and second that defines this foot shape.<ref name="aka">Morton's Toe. <nowiki>http://www.mortonstoe.com/</nowiki> [last accessed 27/6/2018].</ref> | |||
Image: Metatarsal bones of the foot (highlighted in green) - inferior view<ref >Metatarsal bones of the foot (highlighted in green) - inferior view image - © Kenhub https://www.kenhub.com/en/library/anatomy/metatarsal-bones</ref> | |||
< | <br> | ||
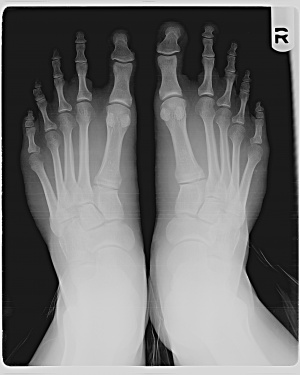
[[Image:Mortons Toe XRay.jpg|thumb|right|X-ray image of a patient with Morton's toe.]] | |||
== History == | |||
The name derives from American orthopedic surgeon Dudley Joy Morton (1884–1960)<ref>[http://www.whonamedit.com/synd.cfm/2701.html Morton's syndrome (Dudley Joy Morton)] at ''Who Named It?''</ref> who originally described it as part of Morton's triad (a.k.a. Morton's syndrome or Morton's foot syndrome) a congenital short first metatarsal bone, a hypermobile first metatarsal segment, and calluses under the second and third metatarsals.<ref name="brage" /> | |||
== Epidemiology == | |||
Tachdjian<ref>Tachdjian MO: “Disorders of the foot” in Tachdjian’s Pediatric Orthopaedics. Ed by JA Herring JA, WB Saunders, Philadelphia, 1990.</ref> reported that the first metatarsal is the most commonly affected metatarsal, although the incidence was found to be 1 in 10,000, whereas a majority of other podiatric and orthopaedic authors claim the fourth brachymetatarsia to be the most common. | |||
The largest series of studies, which are from Japan, reports the incidence of Morton’s syndrome to be somewhere between 1 in 1820-4586 (0.022%-0.05%), and bilateral congenital brachymetatarsia is noted to be 72%. <ref name="brage" /> | |||
There is a strong female to male predisposition in the majority of the podiatric and orthopedic literature. The average ratio is 25:1<ref name="brage" /><ref>Bartolomei FJ: Surgical correction of Brachymetatarsia. J Am Podiatr Med Assoc 80 (2): 76 – 82, 1990.</ref> and the majority of the population studied is between the ages of 5 and 14 years of age.<ref>Goforth WP, Overbeek TD: Brachymetatarsia of the third and fourth metatarsals. J Am Podiatr Med Assoc 91: 373 – 378, 2001.</ref> | |||
== Aetiology == | |||
The aetiology of Morton's toe can be associated with '''idiopathic congenital conditions''' and '''acquired disorders.''' Idiopathic congenital conditions can include such conditions as hereditary early epiphyseal plate closure, associated congenital disorders such as Down’s, Turner’s, Larsen’s, Albright’s syndromes, pseudohypoparathyroidism, [[poliomyelitis]], dystrophic dysplasia, pseudohyperparathyroidism, multiple epiphyseal dysplasia, and myositis ossificans. | |||
Acquired disorders can include trauma, neurotrophic disorder, radiation exposure, surgical resection of the metatarsal head, infection, or osteochondrosis.<ref>Munuera Martínez PV, Lafuente Sotillos G, Domínguez Maldonado G, Salcini Macías JL, Martínez Camuña L: Morphofunctional study of Brachymetatarsia of the fourth metatarsal. J Am Podiatr Med Assoc 94: 347 – 352, 2004.</ref> | |||
Morton’s toe can thus present with one or both of two problems that can affect the first metatarsal bone. | |||
1. First metatarsal bone is shorter than the second metatarsal bone. | |||
< | 2. Hypermobility or instability of the First Metatarsal Bone.<ref name="burton">Burton Schuler. Foot Care for You. <nowiki>http://www.footcare4u.com/mortons-toe-what-is-it-what-causes-it-how-to-treat-it/</nowiki> [last accessed 27/6/2018].</ref> | ||
These in turn affect the normal walking process and places pressure on the second metatarsal during the toe-off phase. | |||
<references /> | Shortness and or hypermobility of the first metatarsal bone is a two-headed monster that decreases the ability of the first metatarsal to work properly. It causes over-pronation when walking and results in putting greater stress and strain not only on the foot but also on the whole body.<ref name="burton" /> | ||
== Pathophysiology == | |||
Pronation is the single most important term used in the discussion of how the foot works. The most common reason for people to have foot problems is due to an abnormal amount of Pronation. Morton’s Toe will cause an individual to have abnormal or overpronation. It is this pronation that is the ultimate cause or contributing factor to most of the problems not only of the foot but also of the whole body.<ref name="burton" /> | |||
Pronation is a series of movements the foot must make in order for us to walk properly. But, it is not that simple. | |||
There are two types of pronation of the foot, | |||
1. normal pronation, or | |||
2. abnormal, or over-pronation | |||
Normal Pronation is a series of motions the foot must-have so that it can absorb the shock of meeting the ground. It must be able to do this, in order to adapt and adjust to the new walking surfaces it has just met. This adjustment should only last a fraction of a second to allow the foot to slow down; absorb the shock of your body weight in order to adjust and adapt to the walking surface.<ref name="burton" /> At this point in time, normal pronation is taking place and the foot is referred to as a “bag of bones” due to its ability to adapt to the new walking or running surfaces. Part of this process of becoming a “bag of bones” is that the arch will start to flatten out and roll toward the ground. Normal pronation should only last no longer than a moment for the foot to adjust. If these adjustments last longer then the foot will begin to abnormally pronate and correct itself. This is the start of a “chain reaction” that puts the foot under a lot of abnormal stress and strain, causing Bunions, Heel Spurs [[Plantarfasciitis|Plantar Fasciitis]], Corns, Callouses, Ingrown Toenail, and numerous other foot problems<ref name="burton" />. | |||
Over or abnormal pronation occurs when the foot is still pronating when it shouldn’t be. Once the foot has adapted to the ground the foot should stop pronating and should be starting to stabilizing itself or locking itself. This locking is called '''Supination''' and is the opposite of Pronation. Supination must take place so the foot can become a “Rigid Lever*” (opposite of “bag of bones”) in order for it to support our body when we push off from the ground and propel us forward for our next step. In Supination the arch of the foot goes up (instead of down as in Pronation) so that it can become the Ridge Lever. But, if you are Over Pronating and you still are a “Bag of Bones and not the Rigid Lever when pushing off from the ground, then your foot and body will attempt to stop the over-pronation by compensation. | |||
This compensation puts the bones, muscles, tendons, ligaments, and other structures under a tremendous amount of abnormal stress and strain not only of the foot but of the whole body. It is this abnormal stress caused by the body attempting to compensate that is the start of most of our feet and body-wide problems. A short first metatarsal bone, and or hypermobility of the first metatarsal bone can lead to a lack of proper stabilization on the forefoot, at the critical moment when the foot must be a “ridge lever” in order for it to push off from the ground. This instability will force the foot to compensate in its attempt to become that “ridge lever”.<ref name="burton" /> | |||
== Associated Problems: == | |||
<span>This foot structure is known to cause and perpetuate musculoskeletal problems. Problems start with the [[Foot Anatomy|feet]] and the list is long.</span><ref name="aka" /> | |||
'''Foot Pain''' | |||
* [[Metatarsalgia]] (ball-of-foot pain) | |||
* [[Morton's Neuroma]] | |||
* Metatarsal Stress Fractures<ref name="burton" /> | |||
* [[Plantarfasciitis]] | |||
* Calluses | |||
* Bunion Hammer, Claw and Mallet toes | |||
<br>'''Lower Extremity Pain''' | |||
* [[Ankle Joint|Ankle]] Pain - Weak Ankles | |||
* Shin splints | |||
* Tight, Sore and Tired Calf Muscles | |||
* [[Knee]] pain | |||
* Tight IT Bands | |||
* Runner's Knee ([[Chondromalacia Patellae|Chondromalacia]]) | |||
* Fractured [[Meniscus rupture|Meniscus]] | |||
* [[Anterior Cruciate Ligament (ACL) Reconstruction|ACL]] Tears | |||
* [[Sciatica]] Pain | |||
* Arthritis | |||
<br>'''Back and Neck''' | |||
* [[Scoliosis]] & [[Thoracic Hyperkyphosis]] | |||
* SI Joint Pain | |||
* Sciatica ([[Piriformis Syndrome]]) | |||
* [[Low Back Pain|Low-Back Pain]] | |||
* Upper Back and [[Shoulder|Shoulder Pain]] | |||
* [[Neck Pain: Clinical Practice Guidelines|Neck Pain]] (head forward posture)<ref name="aka" /><br> | |||
== Treatment == | |||
There are a variety of treatments available for conservative treatment and surgical correction of Morton's toe.<ref name=":1" /> Foot surgery is a last resort, not first aid.<ref name="burton" /> | |||
====Conservative Intervention==== | |||
1. [[Introduction to Orthotics|Orthotic devices]]: Orthotics that feature arch support to keep the foot aligned, and a metatarsal pad to reduce stress on the ball-of-the-foot are often recommended when treating this condition. | |||
2. Metatarsal pads<ref name=":1">Mendeszoon MJ; Kaplan YL; Crockett RS; Cunningham N (2009). Congenital Bilateral First Brachymetatarsia: A Case Report and Review of Available Conservative and Surgical Treatment Options. ''The foot and Ankle Journal'' '''2''' (9): 1.</ref>: The basic, simple treatment for Morton’s Toe and most of the problems associated with it, such as back pain, knee pain, hip pain, fibromyalgia, arthritis, and most foot pains, is with a pad that is applied to the bottom of your first metatarsal bone that we call the “Toe Pad.” It was first written about by Dr. Morton in 1927.<ref name="burton" /> | |||
3. Wide toe-box shoe gear: Proper treatment of Morton's Toe starts with selecting proper footwear. Footwear with a high and wide toe box (toe area) is ideal for treating this condition. It may be necessary to buy footwear a half size to a size larger to accommodate the longer second toe. Proper footwear combined with an effective orthotic will provide relief from the pain associated with Morton's Toe.<ref name="wikihow">How to deal with Morton's Toe. http://www.wikihow.com/Deal-With-Morton's-Toe [last accessed 27 June 2018].</ref> | |||
Taping can also be used to reduce the hypermobility and strengthen the transverse arch of the foot. | |||
{{#ev:youtube|9q0RfhmtDm8|300}} <ref>Dr. Ellen McNally. Morton's Toe Taping Protocol. Available from: https://www.youtube.com/watch?v=9q0RfhmtDm8 [last accessed 27/6/2018]</ref> | |||
====Surgical Intervention==== | |||
1. Metatarsal heads 2-4 resection. | |||
2. Proximal ostectomy of metatarsals 2-4, followed by (Teflon prosthesis) implant arthroplasty in the first metatarsal<ref name=":0">Steedman JT, Peterson HA: Brachymetatarsia of the first metatarsal treated by surgical lengthening. J Pediatr Orthop 12 (6): 780 – 785, 1992.</ref> | |||
3. Chiappara procedure<ref>Chiappara P: Utilisation de la dure-mére dans la chirurgie de l’avant-pied rhumatoide. Mèd Chir Pied 7, 197 – 198, 1991.</ref>: First proximal phalanx shortening, combined with shortening of the proximal aspect of metatarsals 2, 3, 4 and lengthening medial cuneiform – allowing hallucal interphalangeal joint (IPJ) to compensate for first metatarsophalangeal (MTP) joint. <ref name=":0" /> | |||
== Reference: == | |||
<references /> | |||
[[Category:Foot]] | |||
[[Category:Foot - Conditions]] | |||
[[Category:Conditions]] | |||
Latest revision as of 12:46, 12 December 2022
Original Editor - Marlies Verbruggen
Top Contributors -Andeela Hafeez, Marlies Verbruggen, WikiSysop, Edema Emmanuel, Kim Jackson, Admin, Joao Costa, Chrysolite Jyothi Kommu and Richard Benes
Introduction [edit | edit source]
A Morton’s toe otherwise called Morton's foot or Greek foot or Royal toe is characterized by a longer second toe. This is because the first metatarsal, behind the big toe, is short compared to the second metatarsal, next to it. The longer second metatarsal puts the joint at the base of the second toe (the second metatarsophalangeal or MTP joint) further forward. It is a type of brachymetatarsia.[1]
Brachymetatarsia is a condition in which the metatarsal physis closes prematurely yielding a pathologically shortened metatarsal length. It can affect any of the five metatarsal bones of the foot and it could be bilateral. Brachymetatarsia of the first metatarsal is also known as “Morton’s syndrome or Toe”[2]
Morton's toe is a little misleading, because this condition is not really a long toe, meaning the phalanges (toe bones). It is the relative length of the metatarsal foot bones, specifically the relative length difference between the first and second that defines this foot shape.[3]
Image: Metatarsal bones of the foot (highlighted in green) - inferior view[4]
History[edit | edit source]
The name derives from American orthopedic surgeon Dudley Joy Morton (1884–1960)[5] who originally described it as part of Morton's triad (a.k.a. Morton's syndrome or Morton's foot syndrome) a congenital short first metatarsal bone, a hypermobile first metatarsal segment, and calluses under the second and third metatarsals.[1]
Epidemiology[edit | edit source]
Tachdjian[6] reported that the first metatarsal is the most commonly affected metatarsal, although the incidence was found to be 1 in 10,000, whereas a majority of other podiatric and orthopaedic authors claim the fourth brachymetatarsia to be the most common.
The largest series of studies, which are from Japan, reports the incidence of Morton’s syndrome to be somewhere between 1 in 1820-4586 (0.022%-0.05%), and bilateral congenital brachymetatarsia is noted to be 72%. [1]
There is a strong female to male predisposition in the majority of the podiatric and orthopedic literature. The average ratio is 25:1[1][7] and the majority of the population studied is between the ages of 5 and 14 years of age.[8]
Aetiology[edit | edit source]
The aetiology of Morton's toe can be associated with idiopathic congenital conditions and acquired disorders. Idiopathic congenital conditions can include such conditions as hereditary early epiphyseal plate closure, associated congenital disorders such as Down’s, Turner’s, Larsen’s, Albright’s syndromes, pseudohypoparathyroidism, poliomyelitis, dystrophic dysplasia, pseudohyperparathyroidism, multiple epiphyseal dysplasia, and myositis ossificans.
Acquired disorders can include trauma, neurotrophic disorder, radiation exposure, surgical resection of the metatarsal head, infection, or osteochondrosis.[9]
Morton’s toe can thus present with one or both of two problems that can affect the first metatarsal bone.
1. First metatarsal bone is shorter than the second metatarsal bone.
2. Hypermobility or instability of the First Metatarsal Bone.[10]
These in turn affect the normal walking process and places pressure on the second metatarsal during the toe-off phase.
Shortness and or hypermobility of the first metatarsal bone is a two-headed monster that decreases the ability of the first metatarsal to work properly. It causes over-pronation when walking and results in putting greater stress and strain not only on the foot but also on the whole body.[10]
Pathophysiology[edit | edit source]
Pronation is the single most important term used in the discussion of how the foot works. The most common reason for people to have foot problems is due to an abnormal amount of Pronation. Morton’s Toe will cause an individual to have abnormal or overpronation. It is this pronation that is the ultimate cause or contributing factor to most of the problems not only of the foot but also of the whole body.[10]
Pronation is a series of movements the foot must make in order for us to walk properly. But, it is not that simple.
There are two types of pronation of the foot,
1. normal pronation, or
2. abnormal, or over-pronation
Normal Pronation is a series of motions the foot must-have so that it can absorb the shock of meeting the ground. It must be able to do this, in order to adapt and adjust to the new walking surfaces it has just met. This adjustment should only last a fraction of a second to allow the foot to slow down; absorb the shock of your body weight in order to adjust and adapt to the walking surface.[10] At this point in time, normal pronation is taking place and the foot is referred to as a “bag of bones” due to its ability to adapt to the new walking or running surfaces. Part of this process of becoming a “bag of bones” is that the arch will start to flatten out and roll toward the ground. Normal pronation should only last no longer than a moment for the foot to adjust. If these adjustments last longer then the foot will begin to abnormally pronate and correct itself. This is the start of a “chain reaction” that puts the foot under a lot of abnormal stress and strain, causing Bunions, Heel Spurs Plantar Fasciitis, Corns, Callouses, Ingrown Toenail, and numerous other foot problems[10].
Over or abnormal pronation occurs when the foot is still pronating when it shouldn’t be. Once the foot has adapted to the ground the foot should stop pronating and should be starting to stabilizing itself or locking itself. This locking is called Supination and is the opposite of Pronation. Supination must take place so the foot can become a “Rigid Lever*” (opposite of “bag of bones”) in order for it to support our body when we push off from the ground and propel us forward for our next step. In Supination the arch of the foot goes up (instead of down as in Pronation) so that it can become the Ridge Lever. But, if you are Over Pronating and you still are a “Bag of Bones and not the Rigid Lever when pushing off from the ground, then your foot and body will attempt to stop the over-pronation by compensation.
This compensation puts the bones, muscles, tendons, ligaments, and other structures under a tremendous amount of abnormal stress and strain not only of the foot but of the whole body. It is this abnormal stress caused by the body attempting to compensate that is the start of most of our feet and body-wide problems. A short first metatarsal bone, and or hypermobility of the first metatarsal bone can lead to a lack of proper stabilization on the forefoot, at the critical moment when the foot must be a “ridge lever” in order for it to push off from the ground. This instability will force the foot to compensate in its attempt to become that “ridge lever”.[10]
Associated Problems: [edit | edit source]
This foot structure is known to cause and perpetuate musculoskeletal problems. Problems start with the feet and the list is long.[3]
Foot Pain
- Metatarsalgia (ball-of-foot pain)
- Morton's Neuroma
- Metatarsal Stress Fractures[10]
- Plantarfasciitis
- Calluses
- Bunion Hammer, Claw and Mallet toes
Lower Extremity Pain
- Ankle Pain - Weak Ankles
- Shin splints
- Tight, Sore and Tired Calf Muscles
- Knee pain
- Tight IT Bands
- Runner's Knee (Chondromalacia)
- Fractured Meniscus
- ACL Tears
- Sciatica Pain
- Arthritis
Back and Neck
- Scoliosis & Thoracic Hyperkyphosis
- SI Joint Pain
- Sciatica (Piriformis Syndrome)
- Low-Back Pain
- Upper Back and Shoulder Pain
- Neck Pain (head forward posture)[3]
Treatment[edit | edit source]
There are a variety of treatments available for conservative treatment and surgical correction of Morton's toe.[2] Foot surgery is a last resort, not first aid.[10]
Conservative Intervention[edit | edit source]
1. Orthotic devices: Orthotics that feature arch support to keep the foot aligned, and a metatarsal pad to reduce stress on the ball-of-the-foot are often recommended when treating this condition.
2. Metatarsal pads[2]: The basic, simple treatment for Morton’s Toe and most of the problems associated with it, such as back pain, knee pain, hip pain, fibromyalgia, arthritis, and most foot pains, is with a pad that is applied to the bottom of your first metatarsal bone that we call the “Toe Pad.” It was first written about by Dr. Morton in 1927.[10]
3. Wide toe-box shoe gear: Proper treatment of Morton's Toe starts with selecting proper footwear. Footwear with a high and wide toe box (toe area) is ideal for treating this condition. It may be necessary to buy footwear a half size to a size larger to accommodate the longer second toe. Proper footwear combined with an effective orthotic will provide relief from the pain associated with Morton's Toe.[11]
Taping can also be used to reduce the hypermobility and strengthen the transverse arch of the foot.
Surgical Intervention[edit | edit source]
1. Metatarsal heads 2-4 resection.
2. Proximal ostectomy of metatarsals 2-4, followed by (Teflon prosthesis) implant arthroplasty in the first metatarsal[13]
3. Chiappara procedure[14]: First proximal phalanx shortening, combined with shortening of the proximal aspect of metatarsals 2, 3, 4 and lengthening medial cuneiform – allowing hallucal interphalangeal joint (IPJ) to compensate for first metatarsophalangeal (MTP) joint. [13]
Reference:[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Schimizzi, A; Brage, M (September 2004). "Brachymetatarsia". Foot Ankle Clin 9 (3): 555–70, doi:10.1016/j.fcl.2004.05.002. PMID 15324790.
- ↑ 2.0 2.1 2.2 Mendeszoon MJ; Kaplan YL; Crockett RS; Cunningham N (2009). Congenital Bilateral First Brachymetatarsia: A Case Report and Review of Available Conservative and Surgical Treatment Options. The foot and Ankle Journal 2 (9): 1.
- ↑ 3.0 3.1 3.2 Morton's Toe. http://www.mortonstoe.com/ [last accessed 27/6/2018].
- ↑ Metatarsal bones of the foot (highlighted in green) - inferior view image - © Kenhub https://www.kenhub.com/en/library/anatomy/metatarsal-bones
- ↑ Morton's syndrome (Dudley Joy Morton) at Who Named It?
- ↑ Tachdjian MO: “Disorders of the foot” in Tachdjian’s Pediatric Orthopaedics. Ed by JA Herring JA, WB Saunders, Philadelphia, 1990.
- ↑ Bartolomei FJ: Surgical correction of Brachymetatarsia. J Am Podiatr Med Assoc 80 (2): 76 – 82, 1990.
- ↑ Goforth WP, Overbeek TD: Brachymetatarsia of the third and fourth metatarsals. J Am Podiatr Med Assoc 91: 373 – 378, 2001.
- ↑ Munuera Martínez PV, Lafuente Sotillos G, Domínguez Maldonado G, Salcini Macías JL, Martínez Camuña L: Morphofunctional study of Brachymetatarsia of the fourth metatarsal. J Am Podiatr Med Assoc 94: 347 – 352, 2004.
- ↑ 10.0 10.1 10.2 10.3 10.4 10.5 10.6 10.7 10.8 Burton Schuler. Foot Care for You. http://www.footcare4u.com/mortons-toe-what-is-it-what-causes-it-how-to-treat-it/ [last accessed 27/6/2018].
- ↑ How to deal with Morton's Toe. http://www.wikihow.com/Deal-With-Morton's-Toe [last accessed 27 June 2018].
- ↑ Dr. Ellen McNally. Morton's Toe Taping Protocol. Available from: https://www.youtube.com/watch?v=9q0RfhmtDm8 [last accessed 27/6/2018]
- ↑ 13.0 13.1 Steedman JT, Peterson HA: Brachymetatarsia of the first metatarsal treated by surgical lengthening. J Pediatr Orthop 12 (6): 780 – 785, 1992.
- ↑ Chiappara P: Utilisation de la dure-mére dans la chirurgie de l’avant-pied rhumatoide. Mèd Chir Pied 7, 197 – 198, 1991.