Meniscal Repair: Difference between revisions
Evan Thomas (talk | contribs) mNo edit summary |
Evan Thomas (talk | contribs) mNo edit summary |
||
| Line 158: | Line 158: | ||
<references /> | <references /> | ||
<br> | |||
[[Category: | [[Category:Procedures]] [[Category:Knee]] [[Category:Knee_Injuries]] [[Category:Musculoskeletal/Orthopaedics]] [[Category:Vrije_Universiteit_Brussel_Project]] | ||
[[Category:Vrije_Universiteit_Brussel_Project]] | |||
Revision as of 09:30, 10 August 2016
Original Editor - Rachael Lowe, Jennifer Uytterhaegen
Top Contributors - Rachael Lowe, Laura Ritchie, Admin, Van Horebeek Erika, Scott Cornish, Kim Jackson, David Bayard, Lauren Heydenrych, Yannick Goubert, 127.0.0.1, Wendy Walker, Evan Thomas, George Prudden, Wanda van Niekerk and Mahbubur Rahman
Definition/Description[edit | edit source]
| [1] |
An arthroscopic meniscectomy is a procedure to remove some or all of a meniscus from the tibio-femoral joint of the knee using arthroscopic (aka 'keyhole') surgery. In a complete meniscectomy the meniscus including the meniscal rim is removed. A partial meniscectomy involves partial removal of the meniscus. This may vary from minor trimming of a frayed edge to anything short of removing the rim. This is a minimally invasive procedure often done as day suas an outpatient in a one-day clinic [2]
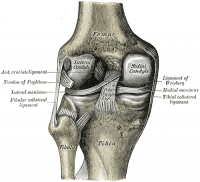
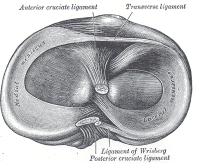
Clinically Relevant Anatomy[edit | edit source]
The menisci of the knee are crescent-shaped fibrocartilaginous structures which add to the tibio-femoral joint congruency while also dispersing friction and body weight. A difference exists between the medial and the lateral meniscus: [3]
- The medial meniscus is larger than the lateral meniscus and has a C shape. It blends with the medial collateral ligament [4]
- The lateral meniscus is smaller than the medial meniscus and has an O-shape. This is more mobile than the medial meniscus and blends with the popliteus muscle. [4]
Indication for Procedure
[edit | edit source]
This procedure is performed when a meniscal tear is too large to be corrected by a surgical meniscal repair.[2]
Clinical Presentation[edit | edit source]
- joint line tenderness and effusion
- symptoms are frequently worsened by flexing and loading the knee, activities such as squatting and kneeling are poorly tolerated
- complaints of 'clicking', 'locking' and 'giving way' are common
- functionally unstable knee [3]
- symptoms are frequently worsened by flexing and loading the knee, activities such as squatting and kneeling are poorly tolerated because of stiffness and pain [2]
Diagnostic Tests[edit | edit source]
- Joint line tenderness has been reported to be the best common test for meniscal injury [2]
- McMurray's test positive if a pop or a snap at the joint line occurs while flexing and rotating the patient's knee.
- Apley's test performed with the patient prone, and with the examiner hyperflexing the knee and rotating the tibial plateau on the femoral condyles.
- Steinman's test performed on a supine patient by bringing the knee into flexion and rotating.
- Ege's Test is performed with the patient squatting, an audible and palpable click is heard/felt over the area of the meniscus tear. The patient's feet are turned outwards to detect a medial meniscus tear, and turned inwards to detect a lateral meniscus tear.
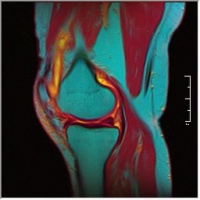
- MRI: The demonstration of meniscal lesions by MRI has a crucial role in patients with combined injuries as the menisci. The main challenge for MRI is the assessment of the meniscal surfaces. MRI signs of abnormal findings include: [5]
- Grade I: Discrete central degeneration - an intrameniscal lesion of increased signal without connection to articular surface [5]
- Grade II: Extensive central degeneration - a larger intrameniscal area of increased signal intensity, again without connection to articular surface. May be horizontal or linear in orientation [5]
- Grade III: Meniscal tear - increased intrameniscal signal intensity with contour disruption of articular surface. May be associated with displacement of meniscal fragments or superficial step formation [5]
- Grade IV: Complex meniscal tear - multiple disruption of meniscal surfaces
The presence of tears in the red versus white zones of the meniscus is important since reattachment of meniscal fragments is promising only in the vascularized zone. [5]
| [6] | [7] |
File:Knee MRI.jpg T1 Weighted MRI |
Medical Management
[edit | edit source]
add text here
Physical Therapy Management
[edit | edit source]
Pre-Operative[edit | edit source]
add text here relating to the pre-operative advice
Post-Operative[edit | edit source]
The goal of rehabilitation is to restore patient function based on individual needs. It is important to consider:
- the type of surgical procedure
- the post-surgical protocol determined by the surgeon [8]
- which meniscus was repaired
- the type of meniscal tear
- preoperative knee status (including time between injury and surgery)
- decreased range of motion or strength
- the patient's age
- the presence of coexisting knee pathology (particularly ligamentous laxity or articular cartilage degeneration)
- the patient's functional and/or athletic expectations and motivations
Rehabilitation Overview[edit | edit source]
- Control the pain, swelling and inflammation by using: cryotherapy, analgaesics, NSAIDs. [5]
- As rehabilitation progresses, continued use of modalities may be required to control residual pain and swelling. [9]
- Restore range of motion using exercises within the limits that the surgeon has specified [5]
- If a meniscal repair has been performed, extreme flexion and rotation should be limited until the wound in the meniscus has had time to heal (8 to 12 weeks).
- Restore muscle function using specific strengthening exercises including quadriceps, hamstrings, hip. Examples: [5][4]
- for quadriceps: squads
- for hamstrings: leg curl with resistance (eg resistance band)
- for hip: bridging
- Strengthening around the knee is crucial but it may also be necessary to strengthen the adjacent joints if weight-bearing was restricted pre- or post-operatively.
- While strong muscles around the joint are critical, flexibility exercises of the same muscle groups must be considered and should be included throughout the period of strengthening.
- Optimize neuromuscular coordination and proprioceptive re-education. [5]
- The patient, physical therapist and surgeon will determine the extent of these exercises. [9]
- Progress weight-bearing: weight-bearing and joint stress are necessary to enhance the functionality of the meniscal repair and should be progressed as indicated by the surgeon.[5]
Additional Considerations[edit | edit source]
| [10] |
- Full weight bearing or bearing weight as tolerated immediately after the meniscectomy
- Passive and active range-of-motion exercises begin immediately postoperatively and quadriceps strengthening exercises
- Crutches are usually required for 2-5 days until the patient is able to fully put his/her body weight on the knee without significant discomfort
- Return to full daily activities usually at 4-6 weeks, providing full range of motion has been regained
- Athletes may return to full athletic activities when normal quadriceps muscle tone has recovered and range of motion is full and pain-free
- EMG-B (electromyography-biofeedback) is an effective treatment in improving quadriceps muscle strength after arthroscopic meniscectomy surgery [4]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
Brindle T, Nyland J, Johnson DL. The meniscus: review of basic principles with application to surgery and rehabilitation. J Athl Train. 2001;36(2):160-169.
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1luR_fr_DOPErVjI4XolF8V92LLei4UyHCfYkHofoMPgh6yYmk|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
- ↑ BJC Houston. Arthroscopic Partial Meniscectomy. Available from: http://www.youtube.com/watch?v=VElp9SpGS-Q [last accessed 18/08/12]
- ↑ 2.0 2.1 2.2 2.3 Meserve BB, Cleland JA, Boucher TR. A meta-analysis examining clinical test utilities for assessing meniscal injury. Clin Rehabil. 2008;22(2):143-161.
- ↑ 3.0 3.1 McKeon B, Bono J, Richmond J, editors. Knee arthroscopy. London:Springer, 2009.
- ↑ 4.0 4.1 4.2 4.3 Atkinson HDE, Laver JM, Sharp E. Physiotherapy and rehabilitation following soft tissue surgery of the knee. Orthop Trauma. 2010;24(2):129-138. Cite error: Invalid
<ref>tag; name "Atkinson" defined multiple times with different content - ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Teller P, Konig H, Weber U, Hertel P. MRI atlas of orthopedics and traumatology of the knee. London:Springer, 2003.
- ↑ CRTechnologies. Steinman I Sign Test (CR). Available from: http://www.youtube.com/watch?v=31mbTI4CsUI[last accessed 15/12/12]
- ↑ CRTechnologies. Ege's Test (CR). Available from: http://www.youtube.com/watch?v=BVXDEAYPYCg[last accessed 15/12/12]
- ↑ Kohn D, Aagaard H, Verdonk R, Dienst M, Seil R. Postoperative follow-up and rehabilitation after meniscus replacement. Scand J Med Sci Sports. 1999;9(3):177-80.fckLR
- ↑ 9.0 9.1 Thomson LC, Handoll HH, Cunningham A, Shaw PC. Physiotherapist-led programmes and interventions for rehabilitation of anterior cruciate ligament, medial collateral ligament and meniscal injuries of the knee in adults. Cochrane Database Syst Rev. 2002;(2):CD001354.
- ↑ MegaElectronicsLtd. Biofeedback rehabilitation after ACL reconstruction (eMotion Biofeedback). Available from: http://www.youtube.com/watch?v=MQYo8B8wKWc[last accessed 15/12/12]