Hepatitis A, B, C: Difference between revisions
No edit summary |
Rujuta Naik (talk | contribs) No edit summary |
||
| (116 intermediate revisions by 14 users not shown) | |||
| Line 1: | Line 1: | ||
<div class="editorbox"> | |||
'''Original Editors '''- Emily Schmidt | '''Original Editors '''-[[User:Emily Schmidt|Emily Schmidt]] [[User:Allyson Simmonds|Allyson Simmonds]] [[Pathophysiology of Complex Patient Problems|from Bellarmine University's Pathophysiology of Complex Patient Problems project.]] | ||
''' | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Introduction == | |||
[[File:Liver gif.gif|right|frameless]]Hepatitis is defined as an inflammation of the [[Liver Disease|liver]]. | |||
< | The condition can be self-limiting or can progress to fibrosis (scarring), cirrhosis or liver [[Oncology|cancer]]. Hepatitis viruses are known to be the most common cause of hepatitis in the world. Other causes include [[Infectious Disease|infections]], toxic substances, and [[Autoimmune Disorders|autoimmune diseases]].<ref name=":1">WHO [https://www.who.int/news-room/q-a-detail/hepatitis Hepatitis] Available from:https://www.who.int/news-room/q-a-detail/hepatitis (last accessed 2.11.2020)</ref><ref name="CDC Hepatitis B">Centers for Disease Control and Prevention. Information for the Public: Hepatitis B FAQs. http://www.cdc.gov/hepatitis/b/bFAQ.htm#statistics (accessed March 3, 2013).</ref> | ||
The most common types of viral hepatitis are Hepatitis A, Hepatitis B, and Hepatitis C. The other types of viral hepatitis are Hepatitis D and E and are less frequently encountered. Based on the etiology of hepatitis, the severity can range from mild and self-limiting to severe illness requiring liver transplantation. | |||
< | Hepatitis can be further classified as:- | ||
* Acute - inflammation of the liver lasts for less than 6 months; usually, self-resolving but can cause fulminant liver failure depending on the etiology | |||
* Chronic - inflammation/insult of the liver lasts longer than 6 months; can cause liver damage that includes liver fibrosis, cirrhosis, hepatocellular carcinoma, and features of portal hypertension leading to significant morbidity and mortality<ref name=":0">Mehta P, Reddivari AK. [https://www.ncbi.nlm.nih.gov/books/NBK554549/ Hepatitis].2020 Available from:https://www.ncbi.nlm.nih.gov/books/NBK554549/ (last accessed 2.11.2020)</ref> | |||
Hepatitis | == Epidemiology == | ||
Viral Hepatitis is considered a major public health issue. Viral hepatitis infects millions of people annually causing significant morbidity and mortality. | |||
*Chronic Hepatitis B and C infection can cause liver damage that includes liver fibrosis, cirrhosis, hepatocellular carcinoma, and features of portal hypertension. | |||
* Viral hepatitis ends up causing 1.4 million deaths annually, and hepatitis B and C viruses are responsible for about 90% of those deaths. | |||
* The World Health Organization (WHO) estimated that 1.3 million people have died due to hepatitis in 2015, and 1 in 3 people in the world have had infections with either hepatitis B or hepatitis C virus. | |||
* Reportedly, infection rates show that 2 billion people infected with the hepatitis B virus, 185 million with the hepatitis C virus, and 20 million with the hepatitis E virus. | |||
* Hepatitis A virus affects 90% of children in high endemic regions<ref name=":0" />. <br> | |||
== Characteristics/Clinical Presentation == | == Characteristics/Clinical Presentation == | ||
Hepatitis | Viral Hepatitis can be different in every individual depending on the type of virus causing the infection. Patients can be entirely asymptomatic or only mildly symptomatic at presentation. A small number of patients can present with rapid onset of fulminant hepatic failure. | ||
Typically patients with viral hepatitis go through 4 phases. | |||
* Phase 1 (viral replication phase) - Patients are usually asymptomatic in this phase, and laboratory studies are positive for markers of hepatitis. | |||
* Phase 2 (prodromal phase) - Patients in this phase usually present with anorexia, nausea, vomiting, malaise, pruritus, urticaria, arthralgias, and fatigue. Many times these patients are misdiagnosed as having gastroenteritis or viral infection. | |||
* Phase 3 (jaundice phase) - Patients in this phase present with dark-colored urine and pale-colored stool. Some patients develop jaundice and right upper quadrant pain with liver enlargement. | |||
* Phase 4 (convalescent phase) - Patients typically start noticing the resolution of symptoms, and [[Laboratory Tests|laboratory studie]]<nowiki/>s show liver enzymes returning to normal levels<ref name=":0" />. | |||
Hepatitis A - Usually presents with symptoms similar to gastroenteritis or viral respiratory infection, including symptoms of fatigue, nausea, vomiting, fever, jaundice, anorexia, and dark urine. Symptoms usually start after the incubation period is over, and they resolve spontaneously in a majority of patients | |||
Hepatitis B - Enter the prodromal phase after the incubation period and have symptoms of anorexia, malaise, and fatigue which are the most common initial clinical symptoms. Some patients may experience right upper quadrant pain due to hepatic inflammation. Once these patients progress to the jaundice phase, they develop jaundice and painful hepatomegaly. dark-colored urine and pale-colored stools. After this phase, clinical course can be variable, some patients experience rapid improvement in the symptoms, and others can develop a prolonged illness with a slow resolution with periodic flareups. A small number of patients can have rapid progression of the disease that can lead to fulminant hepatic failure over a few days to weeks. | |||
Hepatitis C - Develop similar symptoms after the incubation period to those of hepatitis B virus infection during the acute infection phase with symptoms of anorexia, malaise, and fatigue. However, 80% of patients remain asymptomatic and do not develop jaundice<ref name=":0" /> | |||
== Causes == | |||
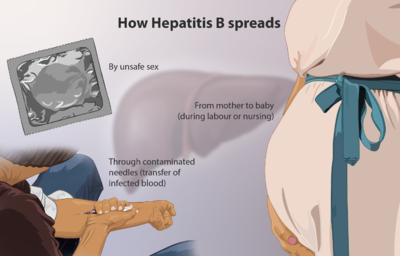
[[File:Hepatitis B.png|right|frameless|400x400px]] | |||
* Hepatitis A and E are typically caused by ingestion of contaminated food or water. Hepatitis B, C and D usually occur as a result of parenteral contact with infected body fluids. Common modes of transmission for these viruses include receipt of contaminated blood or blood products, invasive medical procedures using contaminated equipment. Hepatitis B transmission occurs from mother to baby at birth, from family member to child, and also by sexual contact.<ref name=":1" /> | |||
* Most of the time, hepatitis results from hepatitis viruses A, B, C, D, and E. Hepatitis A, B, and C are endemic to the United States with hepatitis A, B, and C viruses causing 90% of acute viral hepatitis in the United States and Hepatitis C being the most common cause of chronic hepatitis. | |||
Hepatitis A | |||
== Systemic Involvement == | == Systemic Involvement == | ||
Variable systemic involvement can occur with Hepatitis due to the nature of the virus causing a widespread infection in the body. Most predominantly the infection involves the liver and [[Lymphatic System|lymphatic system]]. Other systemic areas of involvement include progression into [[Chronic Kidney Disease|renal]], endocrine, dermatological, [[Cardiovascular Disease|cardiovascular]], rheumatologic, and central nervous system diseases.<ref name="systemic c">Zignego AL, Gragnani L, Giannini C, Laffi G. The Hepatitis C Virus Infection as a Systemic Disease.Intern Emerg Med 2012;7(Suppl 3):S201-S208.</ref>''<u></u>'' | |||
= | |||
== Diagnostic Tests == | |||
Depending on the cause and how advanced the disease is, hepatitis typically is diagnosed with some combination of blood tests, imaging tests, and liver biopsy. | |||
1. [[Blood Tests|Blood tests]] are run to | |||
* Detect the presence of a specific hepatitis virus or for antibodies produced by the immune system to fight the virus | |||
* May include- Liver Function Tests, Antibody Tests,Antibody Tests. | |||
* Look for signs of liver damage . | |||
2. Imaging tests - cannot detect a viral infection of the liver, but can reveal inflammation, changes in size, and tumors that can be consequences of chronic infection or liver disease caused by hepatitis. | |||
3. Liver biopsy - a section of tissue taken from the liver and evaluated under a microscope to look for identifying features disease. The most common type of liver biopsy is a percutaneous biopsy<ref name=":2">verywellhealth [https://www.verywellhealth.com/hepatitis-diagnosis-1759919 Hepatitis] Available from:https://www.verywellhealth.com/hepatitis-diagnosis-1759919 (last accessed 2.11.2020)</ref>, | |||
== | == Management == | ||
The most effective treatment plan for viral hepatitis uses a multifaceted approach and varies depending on the specific type of viral hepatitis. Treatment plans are individualized to best fit the patient's age, medical history, and type and stage of the disease. The goal of treatment is to stop or slow the progression of damage to the liver and minimize and quickly treat any complications, such as such as chronic hepatitis, cirrhosis of the liver, liver failure, liver cancer and death. | |||
The first step in treatment is prevention. Prevention can help avoid passing on the disease or contracting the illness. The risk of infection can be reduced by: | |||
* Receiving Hepatitis A and B [[Vaccines|vaccine]]<nowiki/>s | |||
* Avoiding unnecessary and unsafe injections | |||
* Avoiding unsafe blood products | |||
* Avoiding unsafe sharps and waste collection and disposal | |||
* Avoiding the use of illicit drugs and sharing injection equipment | |||
* Avoiding unprotected sex with infected individuals | |||
* Avoiding the sharing of sharp personal items that may be contaminated with infected [[Blood Physiology|blood]] | |||
* Avoiding tattoos, piercings, and acupuncture performed with contaminated equipment<ref name="WHO Hep C">World Health Organization. Hepatitis C. http://www.who.int/mediacentre/factsheets/fs164/en/ (accessed February 19,2013)</ref><ref name="CDC Hepatitis B" /> | |||
* Keeping a good personal hygiene | |||
* Wash food before consumption | |||
* Ensure the water is clean and safe to drink | |||
* Regular sanitation to control infection or to avoid contracting virus | |||
Viral hepatitis cannot be treated with antibiotics because it is caused by a virus and will be ineffective. Some forms of viral hepatitis are treated with antiviral medications. General treatment of viral hepatitis also includes rest and ensuring good nutrition. | |||
People with viral hepatitis should not drink alcohol or take any supplements, over-the-counter medications or prescription drugs without consulting their health care provider because they can cause liver damage. | |||
For serious cases of viral hepatitis like in the case of liver damage, hospitalization may be necessary. Treatment in the hospital may include medications, a liver biopsy, and other diagnostic testing and treatment. | |||
Complications of viral hepatitis are also treated as appropriate. Treatment of the life-threatening complications of liver failure may include liver transplant for some people. This major surgical procedure involves using a healthy donor liver to replace a severely diseased liver<ref name=":2" />.<ref name="CDC Chronic">Center for Disease Control. Medical Management of Chronic Hepatitis B and Chronic Hepatitis C. http://www.cdc.gov/idu/hepatitis/manage_chronich_hep_b-c.pdf (accessed March 2, 2013).</ref> | |||
Hepatitis A usually requires only supportive/symptomatic treatment as it resolves on its own within a few months time. Targeted HepB antiviral therapy, immunomodulatory drugs and gene silencing technology have been recently used in practice to eradicate the Hepatitis B virus<ref>Almeida PH, Matielo CE, Curvelo LA, Rocco RA, Felga G, Della Guardia B, Boteon YL. Update on the management and treatment of viral hepatitis. World Journal of Gastroenterology. 2021 Jun 6;27(23):3249.</ref>. There are different strains of Hepatitis C virus. A directly acting antiviral drug will be prescribed at first with regular checkups and nutritional advices. The doctor will also advice on preventing the spread of infection. Refer [[Infection Prevention and Control]] for further information. | |||
== | === Physical Therapy Management === | ||
A multifaceted approach is needed in the treatment of '''Hepatitis A, B, and C'''. No specific physical therapy intervention is appropriate for the specific infection of Hepatitis, but Hepatitis may likely be a comorbidity of a patient seen in physical therapy. With any other medical condition, it is important to educate patients on their disease and risk factors to promote awareness and improvement in their healthy lifestyle. In physical therapy, an emphasis on proper musculoskeletal health will be an important foundation for the patient's overall health. Stretching to improve flexibility could help alleviate symptoms of muscle pain. It is also important for the patient to remain physically active in order to maintain the healthiest lifestyle possible and prevent the patient from developing secondary co-morbidities due to inactivity. General strengthening and aerobic activity might be appropriate for a deconditioned patient. Individualizing a physical therapy program focusing on the impairments of the patient is of utmost importance for any patient. | |||
During physical therapy active monitoring the patient for signs and symptoms of fatigue is important. For Hepatitis A, bed rest is the recommended form of treatment and being aware of the acuteness of the Hepatitis infection is important when screening for physical therapy. Supportive therapy and patient education are used to ensure the patient is comfortable and has an adequate nutritional balance for all three infections. It is also important to remind the patient to refrain from the use of alcohol or intake of fatty substances.<ref name="WHO Hep A">World Health Organization. Hepatitis A. http://www.who.int/mediacentre/factsheets/fs328/en/ (accessed February 19, 2013)</ref> | |||
== Measures to take while treating a patient with Hepatitis == | |||
When a confirmed case of hepatitis is admitted to the hospital, individual should be isolated and separate toilet facility should be provided. The area should be disinfected regularly. Doctors and nurses must use gloves and apron while handling contaminated materials. Washing of hands before and after the contact with patient should be done. Decontamination of medical equipment, mattresses, bedsheets and curtains should also be done. The waste should be disposed in appropriate bins. Avoid contact with body fluids of the patient and sharp objects used for the patient. | |||
== | == Complications == | ||
Complications of viral hepatitis include chronic infection with chronic active hepatitis, acute or subacute hepatic necrosis, cirrhosis, liver failure, hepatocellular carcinoma in patients with hepatitis B or C infection. | |||
Patients who have hepatitis B inmonitoring the patient for signs and symptoms of fatigue is important | |||
* Are at high risk of developing chronic infection. | |||
* Also at significant risk of developing hepatocellular carcinoma, which is responsible for 45% of primary liver cancer worldwide. | |||
* About 1% of patients can also develop fulminant hepatic failure, and the mortality rate is about 80% in those patients. | |||
Patients who have hepatitis C infection | |||
* About 75 to 85% of patients with hepatitis C end up developing chronic infection and about 20% of those patients end up developing cirrhosis and eventually hepatocellular carcinoma. | |||
* Cirrhosis developing from hepatitis C infection is a leading cause of liver transplantation in the United States. | |||
* Also have a high risk of developing extrahepatic complications including cryoglobulinemia which can lead to rash, vasculitis, and glomerulonephritis secondary to deposition of immune complexes in the small vessels, non-Hodgkin lymphoma, focal lymphocytic sialadenitis, autoimmune thyroiditis, | |||
== | == Further Reading == | ||
[[Hepatitis C Case Study|Hepatitis C Case Study]] | |||
[[Liver Disease]] | |||
[[Liver Function Tests]] | |||
== References == | == References == | ||
<references /><br> | |||
<references /> | |||
[[Category: | [[Category:Medical]] | ||
[[Category:Global Health]] | |||
[[Category:Bellarmine Student Project]] | |||
[[Category:Acute Care]] | |||
[[Category:Conditions]] | |||
[[Category:Communicable Diseases]] | |||
[[Category:Infection prevention and control]] | |||
Latest revision as of 11:33, 23 May 2023
Original Editors -Emily Schmidt Allyson Simmonds from Bellarmine University's Pathophysiology of Complex Patient Problems project.
Top Contributors - Allyson Simmonds, Emily Schmidt, Vidya Acharya, Lucinda hampton, Kim Jackson, Admin, Elaine Lonnemann, Rujuta Naik, WikiSysop, 127.0.0.1, Wendy Walker, Evan Thomas, Karen Wilson and Nupur Smit Shah
Introduction[edit | edit source]
Hepatitis is defined as an inflammation of the liver.
The condition can be self-limiting or can progress to fibrosis (scarring), cirrhosis or liver cancer. Hepatitis viruses are known to be the most common cause of hepatitis in the world. Other causes include infections, toxic substances, and autoimmune diseases.[1][2]
The most common types of viral hepatitis are Hepatitis A, Hepatitis B, and Hepatitis C. The other types of viral hepatitis are Hepatitis D and E and are less frequently encountered. Based on the etiology of hepatitis, the severity can range from mild and self-limiting to severe illness requiring liver transplantation.
Hepatitis can be further classified as:-
- Acute - inflammation of the liver lasts for less than 6 months; usually, self-resolving but can cause fulminant liver failure depending on the etiology
- Chronic - inflammation/insult of the liver lasts longer than 6 months; can cause liver damage that includes liver fibrosis, cirrhosis, hepatocellular carcinoma, and features of portal hypertension leading to significant morbidity and mortality[3]
Epidemiology[edit | edit source]
Viral Hepatitis is considered a major public health issue. Viral hepatitis infects millions of people annually causing significant morbidity and mortality.
- Chronic Hepatitis B and C infection can cause liver damage that includes liver fibrosis, cirrhosis, hepatocellular carcinoma, and features of portal hypertension.
- Viral hepatitis ends up causing 1.4 million deaths annually, and hepatitis B and C viruses are responsible for about 90% of those deaths.
- The World Health Organization (WHO) estimated that 1.3 million people have died due to hepatitis in 2015, and 1 in 3 people in the world have had infections with either hepatitis B or hepatitis C virus.
- Reportedly, infection rates show that 2 billion people infected with the hepatitis B virus, 185 million with the hepatitis C virus, and 20 million with the hepatitis E virus.
- Hepatitis A virus affects 90% of children in high endemic regions[3].
Characteristics/Clinical Presentation[edit | edit source]
Viral Hepatitis can be different in every individual depending on the type of virus causing the infection. Patients can be entirely asymptomatic or only mildly symptomatic at presentation. A small number of patients can present with rapid onset of fulminant hepatic failure.
Typically patients with viral hepatitis go through 4 phases.
- Phase 1 (viral replication phase) - Patients are usually asymptomatic in this phase, and laboratory studies are positive for markers of hepatitis.
- Phase 2 (prodromal phase) - Patients in this phase usually present with anorexia, nausea, vomiting, malaise, pruritus, urticaria, arthralgias, and fatigue. Many times these patients are misdiagnosed as having gastroenteritis or viral infection.
- Phase 3 (jaundice phase) - Patients in this phase present with dark-colored urine and pale-colored stool. Some patients develop jaundice and right upper quadrant pain with liver enlargement.
- Phase 4 (convalescent phase) - Patients typically start noticing the resolution of symptoms, and laboratory studies show liver enzymes returning to normal levels[3].
Hepatitis A - Usually presents with symptoms similar to gastroenteritis or viral respiratory infection, including symptoms of fatigue, nausea, vomiting, fever, jaundice, anorexia, and dark urine. Symptoms usually start after the incubation period is over, and they resolve spontaneously in a majority of patients
Hepatitis B - Enter the prodromal phase after the incubation period and have symptoms of anorexia, malaise, and fatigue which are the most common initial clinical symptoms. Some patients may experience right upper quadrant pain due to hepatic inflammation. Once these patients progress to the jaundice phase, they develop jaundice and painful hepatomegaly. dark-colored urine and pale-colored stools. After this phase, clinical course can be variable, some patients experience rapid improvement in the symptoms, and others can develop a prolonged illness with a slow resolution with periodic flareups. A small number of patients can have rapid progression of the disease that can lead to fulminant hepatic failure over a few days to weeks.
Hepatitis C - Develop similar symptoms after the incubation period to those of hepatitis B virus infection during the acute infection phase with symptoms of anorexia, malaise, and fatigue. However, 80% of patients remain asymptomatic and do not develop jaundice[3]
Causes[edit | edit source]
- Hepatitis A and E are typically caused by ingestion of contaminated food or water. Hepatitis B, C and D usually occur as a result of parenteral contact with infected body fluids. Common modes of transmission for these viruses include receipt of contaminated blood or blood products, invasive medical procedures using contaminated equipment. Hepatitis B transmission occurs from mother to baby at birth, from family member to child, and also by sexual contact.[1]
- Most of the time, hepatitis results from hepatitis viruses A, B, C, D, and E. Hepatitis A, B, and C are endemic to the United States with hepatitis A, B, and C viruses causing 90% of acute viral hepatitis in the United States and Hepatitis C being the most common cause of chronic hepatitis.
Systemic Involvement[edit | edit source]
Variable systemic involvement can occur with Hepatitis due to the nature of the virus causing a widespread infection in the body. Most predominantly the infection involves the liver and lymphatic system. Other systemic areas of involvement include progression into renal, endocrine, dermatological, cardiovascular, rheumatologic, and central nervous system diseases.[4]
Diagnostic Tests[edit | edit source]
Depending on the cause and how advanced the disease is, hepatitis typically is diagnosed with some combination of blood tests, imaging tests, and liver biopsy.
1. Blood tests are run to
- Detect the presence of a specific hepatitis virus or for antibodies produced by the immune system to fight the virus
- May include- Liver Function Tests, Antibody Tests,Antibody Tests.
- Look for signs of liver damage .
2. Imaging tests - cannot detect a viral infection of the liver, but can reveal inflammation, changes in size, and tumors that can be consequences of chronic infection or liver disease caused by hepatitis.
3. Liver biopsy - a section of tissue taken from the liver and evaluated under a microscope to look for identifying features disease. The most common type of liver biopsy is a percutaneous biopsy[5],
Management[edit | edit source]
The most effective treatment plan for viral hepatitis uses a multifaceted approach and varies depending on the specific type of viral hepatitis. Treatment plans are individualized to best fit the patient's age, medical history, and type and stage of the disease. The goal of treatment is to stop or slow the progression of damage to the liver and minimize and quickly treat any complications, such as such as chronic hepatitis, cirrhosis of the liver, liver failure, liver cancer and death.
The first step in treatment is prevention. Prevention can help avoid passing on the disease or contracting the illness. The risk of infection can be reduced by:
- Receiving Hepatitis A and B vaccines
- Avoiding unnecessary and unsafe injections
- Avoiding unsafe blood products
- Avoiding unsafe sharps and waste collection and disposal
- Avoiding the use of illicit drugs and sharing injection equipment
- Avoiding unprotected sex with infected individuals
- Avoiding the sharing of sharp personal items that may be contaminated with infected blood
- Avoiding tattoos, piercings, and acupuncture performed with contaminated equipment[6][2]
- Keeping a good personal hygiene
- Wash food before consumption
- Ensure the water is clean and safe to drink
- Regular sanitation to control infection or to avoid contracting virus
Viral hepatitis cannot be treated with antibiotics because it is caused by a virus and will be ineffective. Some forms of viral hepatitis are treated with antiviral medications. General treatment of viral hepatitis also includes rest and ensuring good nutrition.
People with viral hepatitis should not drink alcohol or take any supplements, over-the-counter medications or prescription drugs without consulting their health care provider because they can cause liver damage.
For serious cases of viral hepatitis like in the case of liver damage, hospitalization may be necessary. Treatment in the hospital may include medications, a liver biopsy, and other diagnostic testing and treatment.
Complications of viral hepatitis are also treated as appropriate. Treatment of the life-threatening complications of liver failure may include liver transplant for some people. This major surgical procedure involves using a healthy donor liver to replace a severely diseased liver[5].[7]
Hepatitis A usually requires only supportive/symptomatic treatment as it resolves on its own within a few months time. Targeted HepB antiviral therapy, immunomodulatory drugs and gene silencing technology have been recently used in practice to eradicate the Hepatitis B virus[8]. There are different strains of Hepatitis C virus. A directly acting antiviral drug will be prescribed at first with regular checkups and nutritional advices. The doctor will also advice on preventing the spread of infection. Refer Infection Prevention and Control for further information.
Physical Therapy Management[edit | edit source]
A multifaceted approach is needed in the treatment of Hepatitis A, B, and C. No specific physical therapy intervention is appropriate for the specific infection of Hepatitis, but Hepatitis may likely be a comorbidity of a patient seen in physical therapy. With any other medical condition, it is important to educate patients on their disease and risk factors to promote awareness and improvement in their healthy lifestyle. In physical therapy, an emphasis on proper musculoskeletal health will be an important foundation for the patient's overall health. Stretching to improve flexibility could help alleviate symptoms of muscle pain. It is also important for the patient to remain physically active in order to maintain the healthiest lifestyle possible and prevent the patient from developing secondary co-morbidities due to inactivity. General strengthening and aerobic activity might be appropriate for a deconditioned patient. Individualizing a physical therapy program focusing on the impairments of the patient is of utmost importance for any patient.
During physical therapy active monitoring the patient for signs and symptoms of fatigue is important. For Hepatitis A, bed rest is the recommended form of treatment and being aware of the acuteness of the Hepatitis infection is important when screening for physical therapy. Supportive therapy and patient education are used to ensure the patient is comfortable and has an adequate nutritional balance for all three infections. It is also important to remind the patient to refrain from the use of alcohol or intake of fatty substances.[9]
Measures to take while treating a patient with Hepatitis[edit | edit source]
When a confirmed case of hepatitis is admitted to the hospital, individual should be isolated and separate toilet facility should be provided. The area should be disinfected regularly. Doctors and nurses must use gloves and apron while handling contaminated materials. Washing of hands before and after the contact with patient should be done. Decontamination of medical equipment, mattresses, bedsheets and curtains should also be done. The waste should be disposed in appropriate bins. Avoid contact with body fluids of the patient and sharp objects used for the patient.
Complications[edit | edit source]
Complications of viral hepatitis include chronic infection with chronic active hepatitis, acute or subacute hepatic necrosis, cirrhosis, liver failure, hepatocellular carcinoma in patients with hepatitis B or C infection.
Patients who have hepatitis B inmonitoring the patient for signs and symptoms of fatigue is important
- Are at high risk of developing chronic infection.
- Also at significant risk of developing hepatocellular carcinoma, which is responsible for 45% of primary liver cancer worldwide.
- About 1% of patients can also develop fulminant hepatic failure, and the mortality rate is about 80% in those patients.
Patients who have hepatitis C infection
- About 75 to 85% of patients with hepatitis C end up developing chronic infection and about 20% of those patients end up developing cirrhosis and eventually hepatocellular carcinoma.
- Cirrhosis developing from hepatitis C infection is a leading cause of liver transplantation in the United States.
- Also have a high risk of developing extrahepatic complications including cryoglobulinemia which can lead to rash, vasculitis, and glomerulonephritis secondary to deposition of immune complexes in the small vessels, non-Hodgkin lymphoma, focal lymphocytic sialadenitis, autoimmune thyroiditis,
Further Reading[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 WHO Hepatitis Available from:https://www.who.int/news-room/q-a-detail/hepatitis (last accessed 2.11.2020)
- ↑ 2.0 2.1 Centers for Disease Control and Prevention. Information for the Public: Hepatitis B FAQs. http://www.cdc.gov/hepatitis/b/bFAQ.htm#statistics (accessed March 3, 2013).
- ↑ 3.0 3.1 3.2 3.3 Mehta P, Reddivari AK. Hepatitis.2020 Available from:https://www.ncbi.nlm.nih.gov/books/NBK554549/ (last accessed 2.11.2020)
- ↑ Zignego AL, Gragnani L, Giannini C, Laffi G. The Hepatitis C Virus Infection as a Systemic Disease.Intern Emerg Med 2012;7(Suppl 3):S201-S208.
- ↑ 5.0 5.1 verywellhealth Hepatitis Available from:https://www.verywellhealth.com/hepatitis-diagnosis-1759919 (last accessed 2.11.2020)
- ↑ World Health Organization. Hepatitis C. http://www.who.int/mediacentre/factsheets/fs164/en/ (accessed February 19,2013)
- ↑ Center for Disease Control. Medical Management of Chronic Hepatitis B and Chronic Hepatitis C. http://www.cdc.gov/idu/hepatitis/manage_chronich_hep_b-c.pdf (accessed March 2, 2013).
- ↑ Almeida PH, Matielo CE, Curvelo LA, Rocco RA, Felga G, Della Guardia B, Boteon YL. Update on the management and treatment of viral hepatitis. World Journal of Gastroenterology. 2021 Jun 6;27(23):3249.
- ↑ World Health Organization. Hepatitis A. http://www.who.int/mediacentre/factsheets/fs328/en/ (accessed February 19, 2013)