Foundations for Ankle Foot Orthoses
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson and Tarina van der Stockt
Introduction[edit | edit source]
An Ankle Foot Orthosis is a specific type of assistive device that, as it’s name suggests, covers the foot and ankle. There are three main types of AFO’s that are constructed, Flexible, Rigid and Jointed. Each device has specific advantages and disadvantages. The goal of the Orthotist is to create an apparatus that will ultimately give the patient the highest functional level. This does not mean a generic one-size-fits -all device, this means the device should have maximal compliance of use and should not hinder the patient but provide assistance for them to achieve their highest functional level. There are many different types of AFOs which will be covered below. Each device has indications and contraindications where an accurate assessment of the patent and their needs is vital. An AFO can be custom made or off-the-shelf, and both have their place in the rehabilitation journey.
Types of AFO[edit | edit source]
- AFO - Ankle Foot Orthosis
- GRAFO - Ground Reaction Ankle Foot Orthosis
- DAFO - Dynamic Ankle Foot Orthosis
- SMAFO - Supramalleolar Ankle Foot Orthosis
- Custom Made
- Off the shelf
Orthotic Assessment [edit | edit source]
Passive Assessment:
Active Assessment:
- Level of mobility
- Gait Pattern
- Compensation Mechanisms of Instability
- Risk of injury
- Pain
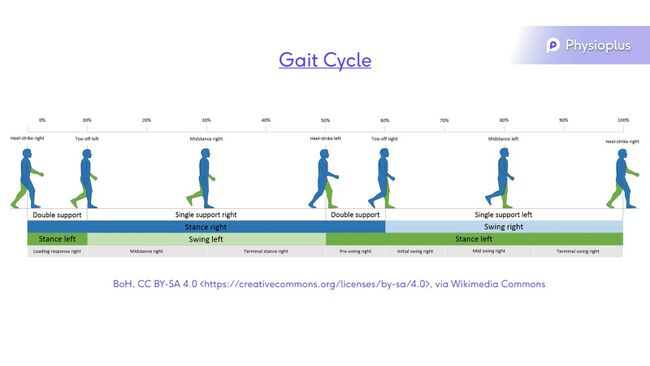
Gait Cycle[edit | edit source]
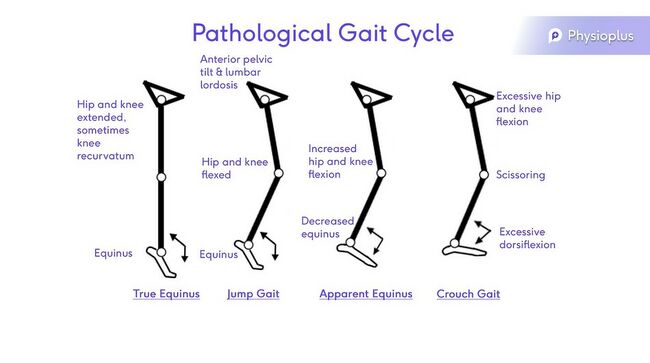
Pathological Gait Cycle:
This can be dues to:
- Pain
- Joint ROM limitations
- Muscle weakness/ paralysis
- Neurological deficit
- Sensory deficit
- Leg length
Pathologies[edit | edit source]
- Paediatrics:
- Neural Tube Defect / Spina Bifida
- Cerebral Palsy
- Muscular Dystrophy
- Cerebral Vascular Accident
- Sometimes fitted with an off-the-shelf device.
- Early intervention will produce the best outcomes and function.
- Late intervention often includes the accommodation of a fixed position. The goal is comfort and pain relief, possibly to prevent worsening of the condition.
- Multiple Sclerosis
- This is a progressive condition. Initially an AFO can assist with slowing down the loss of function due to disease progression, but the use of splinting is reduced as the condition progresses further.
- Polio
- Early intervention will produce the best outcomes and function.
- Early intervention can prevent contractures due to muscle weakness following the virus
- AFO's can be used in conjunction with other devices as the weakness can be higher than the ankle.
- Neuropathy
- Hereditary Motor Sensory Neuropathy (HMSN), also known as Charcot-Marie-Tooth Disease
- A hereditary, progressive disease that affects the nerves. It presents as weakness and numbness which is usually more pronounced in the legs than the arms. The condition begins peripherally and advances up the length of the nerve.
- Diabetes
- Orthotics can damage the tissues as the patients commonly have sensory and neuropathic problems. Minimal pressure of the hard orthotic device on the skin is crucial.
- Tumor
- AFO's can assist with complications due to nerve damage.
- Hereditary Motor Sensory Neuropathy (HMSN), also known as Charcot-Marie-Tooth Disease
- Trauma
- Nerve injury
- Nerve damage may be permanent, or temporary
- An AFO could assist with gait and fall prevention.
- Pain
- Movement can often cause pain in certain pathalogical conditions or trauma. An AFO can be used to restrict movements causing pain and therefore reduce pain.
- Instability
- Nerve injury
Goal setting/ Prescription[edit | edit source]
- Positioning
- Should be in the position that causes the least amount of pain.
- Aim for the most functional position
- When neutral is not possible, always aim for the optimal position.
- Provide Support
- Prevent Contractures
- If a contracture is present already, aim to accommodate those contractures.
- Improve Mobility
- Increase Stability
- Decrease Pain
- Patient Needs
Design/ Manufacture[edit | edit source]
- AFOs are broken down to two main categories: Custom made or Off-the-shelf
- Custom made
- Manufactured using a plaster cast
- Off the shelf
- When sizing an off the shelf AFP either measure for a foot plate or the calf
- Designed in small, medium, and large
- Generally need to be slightly adjusted, especially there is an underlying condition
- Custom made
- Mostly manufactured from a plaster model
- Polypropylene/ lamination/ Carbon Fibre
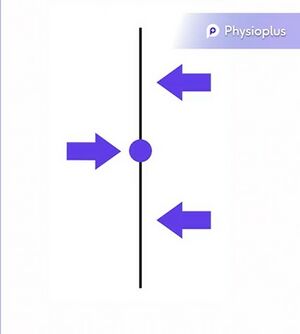
- Use a 3 point force system
3 Point Pressure System[edit | edit source]
This system is used to stabilizes a joint or segment and it can reduce angular rotation. A force is often applied medio-laterally or antero-posteriorly.[1]
The Three Point Force System or Three Point Pressure System is paramount to creating an orthosis. [2] Basically this means, a primary force is applied, with counterforces being applied both above and below the primary force. The sum of these three forces applied should be zero. The amount of force, and the position at which the primary force is applied, should be the point where movement is required to be increased or decreased. This will vary depending on the assessment and functional requirements of the patient, along with the goal of treatment established.[3][4]
When applying a force, it is important to remember the scientific equation of: Pressure equals Force over Area.[5]
In the process of creating an orthotic device the longer the lever arm or the longer the orthosis is, and the further away the points of force is, the bigger the correction will be. As there is more surface area to spread the force over, the pressure can be reduced using this principle. This principle can be used to reduce discomfort of an orthosis.
Foot/Ankle Position[edit | edit source]
When designing an AFO, the goal is the best position the foot and ankle in conjunction with patient requirements. This means:
- The least painful position
- The best position possible
- Might not always be able to reach neutral, so the optimum available position is the most desirable outcome.
- Highest functional level
Casting Procedure[edit | edit source]
When creating an AFO, a mold of the patient's foot and ankle is made using a plaster cast. This is then removed, which can cause some fear is small children or persons with impaired mental ability. From the negative cast of the optimum foot position, a positive cast is made using plastic draping. The custom device can be created using this new positive cast.
3D printing is used occasionally but the disadvantage is that is difficult to maintain the optimum position long enough to complete the scan before the 3D printer can create the device. Once this technology is improved, this might be an effective way of creating an AFO.
Common Ankle Foot Orthosis[edit | edit source]
- Flexible A.F.O.
- Rigid/Solid A.F.O.
- Jointed A.F.O.
1. Flexible AFO[edit | edit source]
A flexible AFO has a certain amount of flexibility around the ankle area. This is achieved by cutting away part of the device around the ankle. The loss of surface area will reduce the effect of the Three Point Pressure System and as a result, this is not suitable for patients with mediolateral instability. A flexible AFO is useful in the group of patients that have increased, uncontrolled movement in the ankle joint with good mediolateral instability. This type of device can allow for some roll over which encourages a natural gait pattern. It's easier to get out of chairs, to go up and down stairs and for children, it's easier to play on the floor and to move around.
Prescription Criteria For A Flexible A.F.O.[edit | edit source]
- Drop foot
- In order for the foot to clear the ground, a patient will often excessively flexes their hip and their knee, swings the leg into circumduction, or toe walks on the opposite side.[6] These compensatory movements lead to extra energy being used, tiring of the patient and an increased falls risk. [7]A flexible AFO can correct the position to plantigrade but will allow some movement through midstance, which makes a more natural gait pattern but also, more importantly, allows the foot to clear the ground.[8]
- Mobile foot/ankle
- No tendency to valgus or varus
Common conditions include[edit | edit source]
- CVA
- Nerve injury/dysfunction
- Pediatrics
Off-the-shelf Flexible AFO[edit | edit source]
Also known as a posterior leaf spring (PLS) as they essentially have a spring at the back of the AFO.[9]
These AFO's are commonly used in short term situations to correct a situation while a custom splint is being designed or while the patients condition improves. These are commonly used in hospital or a trauma-type settings to maintain range.
2. Rigid A.F.O.[edit | edit source]
A rigid AFO is an orthotic device, custom made for the individual that allows no movement. These are often used in more severe situations and in conditions with some mediolateral instability. The rigid AFO allows the three point pressure system to function in the optimal way. It also influences the ground-reaction forces. A gait analysis it is important when constructing these devices because we need to now what type of correction to apply.[10] If the AFO moves the ground-reaction force in front of the knee joint at mid-stance, it will create a hyperextension moment. Alternatively, if the ground-reaction force is moved or remains behind the knee joint, it will create a flexion moment at mid-stance.
A ground-reaction AFO (GRAFO) is essentially the same as a rigid AFO. The difference is that an anterior shell is attached, which will spread the load, which is applied as part of our three-point pressure force system, to the front of the shin. The force is applied at the front of the shin to extend the knee and to maintain the ankle in a plantigrade position.
Prescription Criteria For A Rigid A.F.O.[edit | edit source]
- Slight tendency to flex at knee
- Muscle Tightness
- Dynamic/Fixed
- A tight muscle which is fixed requires accommodation, therefore the position of the ankle is not plantigrade. The design of the AFO must compensate for the equinus position, or a plantarflexed position. This means that when the user of the AFO is standing, the ground-reaction force is in the correct position and the knee is not being pushed into hyperextension or flexion[11].
- Crouch/ Equinus Gait
- Hyper-extension
- Escape Valgus
- Dynamic/Fixed
- Valgus Deformities
- Often a compensatory movement
- Driven by tight tendon Achilles
- Can alter foot structure
- Can result in long term issues
- Mediolateral instabilities, where the rigid AFO we can apply that lovely three-point pressure force system.
- Rocker Bottom Foot
- Need to be supported to reduce pain and prevent deterioration
- Hyper-mobility
- Excessive dorsiflexion requires more stability. This is achieved by creating a more rigid base to stand on and influence the ground-reaction force which allows the knee and hips to extend.
- Escape Valgus
- Dynamic tightness can lead to an escape valgus, where the hindfoot moves into a valgus position because of the tightness in the tendon Achilles. This should be accommodated within a rigid AFO.
- Rocker Bottom Foot
- Varus Deformities
- Often difficult to control
- If presented with a fixed deformity
- Accommodate the deformity
- If presented with a flexible deformity
- Correct to the optimum position to allow the patient to function within the rigid AFO
- Crouch/Excessive Dorsiflexion
- Aim to produce an extension moment through the rigidity of the AFO, which can affect the flexion at the knee[11]
Common Conditions[edit | edit source]
- Cerebral Palsy
- Neural Tube Defect
- Stroke
- Trauma
- Pain
3. Jointed A.F.O.[edit | edit source]
A jointed AFO is made with a moving part, or joint, which hinges at the ankle joint. It s designed to allow motion at the ankle joint but still offer the correction that the Three Point Pressure System offers. The jointed AFO is a good tool to try and optimise a gait pattern.
Disadvantages:
- Tend to be bulkier, which can cause difficulty with footwear
- Can be noisy
- Parts can break
Advantages:
- Walking up and down stairs
- Getting up from a chair
- Moving around the floor, specifically for children
Prescription Criteria for a Jointed A.F.O.[edit | edit source]
- ROM in ankle joint
- Tendency to valgus
- Tendency to varus
- Tendency to Crouch
Prescription criteria for Jointed AFO and DAFO/SMAFO[edit | edit source]
- Hyper mobile foot/ankle
- Ankle to plantargrade
- Medio-lateral instability
Tuning/ Optimising AFOs [edit | edit source]
Once the AFO has been manufactured and fitted, optimisation can done in conjunction with footwear.[12] Walking in an AFO with out footwear is dangerous and slippery. An AFO is always prescribed with a good type of footwear and the footwear will influence how the patient will function in the AFO and their gait pattern.[13] The orthotist needs to look at the footwear closely, and then optimise the angles of the AFO to influence the ground-reaction force[14].[15]
References[edit | edit source]
- ↑ Kadhim FM, Al-Din Tahir MS. Design and Analysis of Three-Point Pressure for Varus Foot Deformity. InJournal of Biomimetics, Biomaterials and Biomedical Engineering 2020 (Vol. 45, pp. 1-11). Trans Tech Publications Ltd.
- ↑ Condie DN, Meadows CB. Some biomechanical considerations in the design of ankle-foot orthoses. Orthot Prosthet. 1977 Jan 1;31(3):45-52.
- ↑ Lahr A. Design of a Modular Ankle-Foot Orthosis (Doctoral dissertation, The Ohio State University).
- ↑ Klenow T, Stevens P. Orthotic Management of the Mangled Extremity. InThe Mangled Extremity 2021 (pp. 243-255). Springer, Cham.
- ↑ Maxwell JC. On Faraday's lines of force. Good Press; 2021 Apr 11.
- ↑ Daryabor A, Arazpour M, Aminian G. Effect of different designs of ankle-foot orthoses on gait in patients with stroke: A systematic review. Gait & posture. 2018 May 1;62:268-79.
- ↑ Pongpipatpaiboon K, Mukaino M, Matsuda F, Ohtsuka K, Tanikawa H, Yamada J, Tsuchiyama K, Saitoh E. The impact of ankle–foot orthoses on toe clearance strategy in hemiparetic gait: a cross-sectional study. Journal of neuroengineering and rehabilitation. 2018 Dec;15(1):1-2.
- ↑ Choo YJ, Chang MC. Effectiveness of an ankle–foot orthosis on walking in patients with stroke: A systematic review and meta-analysis. Scientific reports. 2021 Aug 5;11(1):1-2.
- ↑ Saeedi H, Pourhoseingholi E. Comparison the effect of kinetic parameters of innovative storing-restoring hybrid passive (comfort gait) ankle-foot orthosis (AFO) with posterior leaf spring AFO in drop-foot patients: A prospective cohort study. Current Orthopaedic Practice. 2020 Sep 1;31(5):437-41.
- ↑ Totah D, Menon M, Jones-Hershinow C, Barton K, Gates DH. The impact of ankle-foot orthosis stiffness on gait: A systematic literature review. Gait & posture. 2019 Mar 1;69:101-11.
- ↑ 11.0 11.1 Butler PB, Farmer SE, Stewart C, Jones PW, Forward M. The effect of fixed ankle foot orthoses in children with cerebral palsy. Disability and Rehabilitation: Assistive Technology. 2007 Jan 1;2(1):51-8.
- ↑ Oudenhoven LM, Kerkum YL, Buizer AI, van der Krogt MM. How does a systematic tuning protocol for ankle foot orthosis–footwear combinations affect gait in children in cerebral palsy?. Disability and Rehabilitation. 2021 Sep 7:1-1.
- ↑ Stallard J, Woollam PJ. Transportable two-dimensional gait assessment: routine service experience for orthotic provision. Disability and rehabilitation. 2003 Jan 1;25(6):254-8.
- ↑ Jagadamma KC, Coutts FJ, Mercer TH, Herman J, Yirrel J, Forbes L, Van Der Linden ML. Effects of tuning of ankle foot orthoses-footwear combination using wedges on stance phase knee hyperextension in children with cerebral palsy–preliminary results. Disability and Rehabilitation: Assistive Technology. 2009 Jan 1;4(6):406-13.
- ↑ Owen E. The importance of being earnest about shank and thigh kinematics especially when using ankle-foot orthoses. Prosthetics and orthotics international. 2010 Sep;34(3):254-69.