Foundations for Ankle Foot Orthoses
Top Contributors - Carin Hunter, Jess Bell, Kim Jackson and Tarina van der Stockt
Introduction[edit | edit source]
an overview of different types of ankle-foot orthosis. In orthotics, we tend to name the devices by the joints that we are trying to control or where the device is fitted. So, with an ankle-foot orthosis, we're obviously going to include the foot and the ankle and as we go higher up the body, then KAFO is knee-ankle-foot orthosis, and so on.
So, different types of AFOs that we see. There's an AFO and I've also mentioned a GRAFO, which is a ground reaction AFO. So, I'll talk a little bit about that as we move through the different types. And then we have DAFOs, or dynamic AFOs, SMAFOs, which are supramalleolar AFOs, and all of these different types of orthotic devices can be custom made, which with AFOs is more common or there are a number of off-the-shelf devices, which we can also use to treat our patients.
So, before we consider what we're going to do, we need to have a look at our patients and always, we start with our orthotic assessment.
Types of AFO[edit | edit source]
- AFO - Ankle Foot Orthosis
- GRAFO - Ground Reaction Ankle Foot Orthosis
- DAFO - Dynamic Ankle Foot Orthosis
- SMAFO - Supramalleolar Ankle Foot Orthosis
- Custom Made
- Off the shelf
Orthotic Assessment [edit | edit source]
Passive Assessment:
Active Assessment:
- Level of mobility
- Gait Pattern
- Compensation Mechanisms of Instability
- Risk of injury
- Pain
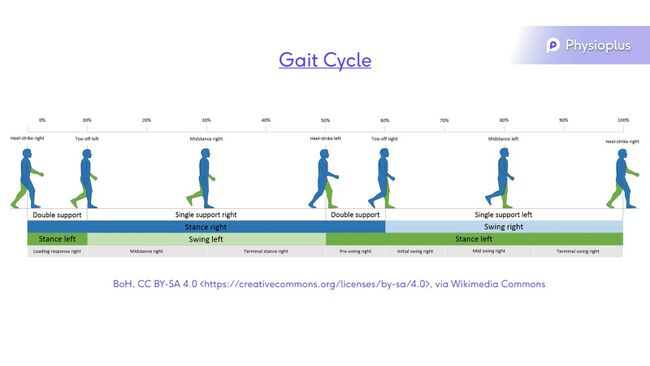
Gait Cycle[edit | edit source]
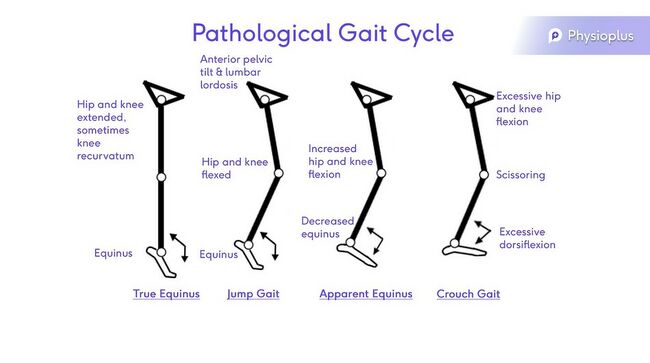
Pathological Gait Cycle:
This can be dues to:
- Pain
- Joint ROM limitations
- Muscle weakness/ paralysis
- Neurological deficit
- Sensory deficit
- Leg length
Pathologies[edit | edit source]
- Paediatrics:
- Neural Tube Defect / Spina Bifida
- Cerebral Palsy
- Muscular Dystrophy
- Cerebral Vascular Accident
- Sometimes fitted with an off-the-shelf device.
- Early intervention will produce the best outcomes and function.
- Late intervention often includes the accommodation of a fixed position. The goal is comfort and pain relief, possibly to prevent worsening of the condition.
- Multiple Sclerosis
- This is a progressive condition. Initially an AFO can assist with slowing down the loss of function due to disease progression, but the use of splinting is reduced as the condition progresses further.
- Polio
- Early intervention will produce the best outcomes and function.
- Early intervention can prevent contractures due to muscle weakness following the virus
- AFO's can be used in conjunction with other devices as the weakness can be higher than the ankle.
- Neuropathy
- Hereditary Motor Sensory Neuropathy (HMSN), also known as Charcot-Marie-Tooth Disease
- A hereditary, progressive disease that affects the nerves. It presents as weakness and numbness which is usually more pronounced in the legs than the arms. The condition begins peripherally and advances up the length of the nerve.
- Diabetes
- Orthotics can damage the tissues as the patients commonly have sensory and neuropathic problems. Minimal pressure of the hard orthotic device on the skin is crucial.
- Tumor
- AFO's can assist with complications due to nerve damage.
- Hereditary Motor Sensory Neuropathy (HMSN), also known as Charcot-Marie-Tooth Disease
- Trauma
- Nerve injury
- Nerve damage may be permanent, or temporary
- An AFO could assist with gait and fall prevention.
- Pain
- Movement can often cause pain in certain pathalogical conditions or trauma. An AFO can be used to restrict movements causing pain and therefore reduce pain.
- Instability
- Nerve injury
Goal setting/ Prescription[edit | edit source]
- Positioning
- Should be in the position that causes the least amount of pain.
- Aim for the most functional position
- When neutral is not possible, always aim for the optimal position.
- Provide Support
- Prevent Contractures
- If a contracture is present already, aim to accommodate those contractures.
- Improve Mobility
- Increase Stability
- Decrease Pain
- Patient Needs
Design/ Manufacture[edit | edit source]
- AFOs are broken down to two main catagories: Custom made or Off-the-shelf
- Custom made
- Manufactured using a plaster cast
- Off the shelf
- When sizing an off the shelf AFP either measure for a foot plate or the calf
- Designed in small, medium, and large
- Generally need to be slightly adjusted, especially there is an underlying condition
- Custom made
- Mostly manufactured from a plaster model
- Polypropylene/ lamination/ Carbon Fibre
- Use a 3 point force system
3 point force system[edit | edit source]
• Stabilizes a joint or segment
• Reduces angular rotation
• Medio-lateral or antero-posterior
• Longer the lever arm the greater the force
• Pressure= Force /Area
Generally, within an AFO, we are using what's called a three-point pressure force system and this is really key in all of orthotics, where we're trying to correct a deformity, we can apply a three-point pressure force. So, for example, if you have a joint where it is tending to go into a flexed position, or let's say at the ankle into a valgus position, and we want to correct this, one option is you can correct directly on the at the apex of where you have the deformity. But also, what is from a scientific point of view, if you can apply a force below and above where the joint is, you can also correct this and then with a counterforce over the joint, you can maintain the correction. This can reduce any angular rotations; it can be applied in a mediolateral way or in an anterior-posterior.
So, if you're looking at a valgus or varus deformity in an ankle, you can apply a force above and below the deformity on the medial or lateral sides, and then a counterforce on the opposite side. And in the same way of you have a plantarflexion or dorsiflexion issue, from an anterior-posterior aspect, you can apply a force above the ankle joint and below the ankle joint and then a counterforce at the position of the ankle joint. So, it's a very useful way of correcting a position and it's also very important to understand how a three-point pressure force works when you're manufacturing and designing the orthosis.
And one important point, I think also to note, is when you are applying a force, force over area equals pressure. So, the longer the lever arm, so the longer your orthosis is, and the further away your points of force are, the bigger the correction you will get, the bigger the lever arm, but also the more surface area you have to spread the force over, the less chance you have pressure. So, all of this is it's all down to physics and we would look at this very carefully when we're designing our AFOs and deciding on which type is best, where we need to apply the forces, how we apply the forces and how much surface area we can spread those forces across to reduce discomfort and pressure.
Foot/Ankle Position[edit | edit source]
So, talking of position and how do we correct position? First of all, we must physically look at the patient. So, we've done our assessment and then we have to decide on what is our optimum position for the ankle-foot orthosis. So, before we take our cast, we decide with the patient how we can best position the foot and ankle. So, in the least painful position, in the most functional position, or in the best position that we possibly can because there may be shortening of a muscle. So, if you have shortening of your gastrocnemius or tightness in your tendon Achilles, you may not be able to achieve what we may call a neutral position. So, you have to then accept what is the best position, so we're looking for optimum, but it's not always neutral. And then we have to design the orthosis around that and take that into account then when the patient is walking and functioning with the orthosis.
Casting Procedure[edit | edit source]
A mold of the patient's foot and ankle is made using a plaster cast. It should be positioned in the correct way. And then from that cast, we would manufacture usually using some sort of polypropylene. So, there are different types of materials that we can use and depending on whether we're looking for a rigid splint, if we're looking for a flexible splint, whether we want specific areas of forces, we will use the type of material. You can also have what's called a laminated version or a carbon fibre version where there is very light, but very strong and can also provide flexibility depending on the design of the materials.
So, once we've achieved and decided what our best position is, we would then take a plaster cast. Now, there are technologies which have been around for a number of years now, everyone is familiar with scanning and 3D printing, and often people will ask me, why don't you 3D print your orthosis? And yes, it is possible, of course it is. And in some places around the globe, they are 3D printing orthosis. What I think the challenge that we find as an industry from an orthotic point of view is that it's quite difficult to achieve the optimum position that I've just spoken about and to hold the foot in that position and also take an accurate scan, which can then allow you to make an accurate device. So, I absolutely believe that in the future this will be how orthotics will be manufactured and a shape will be captured and designed, but at the moment, I think taking plaster casts is still probably the most standard way of doing this and certainly how orthotists are still trained.
So, making sure that you have your position, obviously you have to reassure the patient because it can be quite a scary experience, especially for children, having a plaster cast taken and then having it taken off. So, having the patient comfortable, get the position of the foot and ankle where you have decided is the optimum position, and then take your cast. And from that cast you can then make your device. And usually what we do is we do a drape of plastic, which is heated in an oven, and so from the negative cast, we produce a positive cast, it's modified, and from the positive cast, we then produce our device. So, there's quite a lot of intensive man-hours and work involved in producing a custom-made AFO.
Common Ankle Foot Orthosis[edit | edit source]
- Flexible A.F.O.
- Rigid/Solid A.F.O.
- Jointed A.F.O.
1. Flexible AFO[edit | edit source]
And just by its nature, a flexible AFO means that it does move, so there is a certain amount of flexibility around the ankle area in the AFO and the reason that we might want to have flexibility is if we have mobility in our ankle joint, and sometimes the problem is not always tightness or stiffness or reduced movement, sometimes it's too much movement. So, if you have someone who has a drop foot, they have a floppy foot in swing, this can lead to compensation movements, which we spoke about earlier. If someone is walking with a drop foot and to prevent themselves from tripping up, what they're inclined to do is they will excessively flex their hip and excessively flex their knee in order to clear the ground, or perhaps they may even swing the leg into circumduction, they might go up on their toes on the other side, and all of these compensation movements lead to extra energy, and also the nature of the drop foot is that as you get more tired, you're less likely to compensate well, and you're more likely to fall. So, in a drop foot situation, we can correct, if we can correct the position to plantigrade, we can manufacture a flexible AFO which will allow some movement through midstance, which makes a more natural gait pattern but also, more importantly, allows the foot to clear the ground.
So, our mobile foot-ankle would be preferable when prescribing a flexible AFO. Generally, we're looking for good ML alignment, so very little mediolateral instability because the nature of the design of a flexible AFO is that we actually cut away some of the material around the ankle and what this means is that we've lost that surface area to apply our three-point pressure force. So, if we have a large varus or valgus problem, then we may not have enough material in a flexible AFO to provide those forces and more likely they will be suited to a rigid AFO.
But if we have very little instability mediolaterally, so for example, we may have a flaccid drop foot following a stroke. We may have a nerve injury or nerve dysfunction where the dorsiflexors are not working. So, we can correct the foot into a nice position. And often we see them in paediatrics where we have a very active, smaller child and we still have a nice range of movement and we're able to position them into a nice functional position. And there is no doubt that having flexibility at the ankle, it's not natural for us to have a rigid ankle or gait pattern, we spoke about the difference between normal and pathological. It's not always possible to normalise the gait pattern, but that is our aim in a lot of cases. So, if we can allow for some roll over and not have a rigid ankle, then it makes for a much more natural gait pattern. It's easier to get out of chairs. It's easier to go up and down stairs. And for children, it's easier to play on the floor and to move around. So, some advantages, but again, if the position and the assessment that you've done doesn't lend itself to having flexibility in the ankle, then there is no advantage to having a flexible AFO.
There are also a range of off-the-shelf flexible AFOs.
Again, often there is another term for a flexible AFO, which is a PLS or a posterior leaf spring, and that's often a term that's used to describe the fact that we have a spring almost at the back of the AFO. And again, by the nature of the material that we use, which can be carbon fibre, which can give a nice spring, but is very strong, or by some plastic depending on the thickness, you can also get a nice flexible splint and the off-the-shelf splints do have a place. Invariably, we find they're most useful in short-term situations, so perhaps in a hospital setting or a trauma-type setting or following a CVA to maintain range until they can get a customised AFO. And as I say, the carbon fibre AFOs that they are producing now have more longevity and can be a really excellent choice for more active patients and certainly for adolescent and adult patients.
Prescription Criteria For A Flexible A.F.O.[edit | edit source]
- Drop foot
- Mobile foot/ankle
- No tendency to valgus or varus
Common conditions include[edit | edit source]
- CVA
- Nerve injury/dysfunction
- Paediatrics
OTS Flexible AFO[edit | edit source]
2. Rigid A.F.O.[edit | edit source]
And as we'd follow suit, if you have a more severe issue, a more severe condition, or a more severe effect from a condition, then you may require a more in-depth type of orthosis, such as a rigid AFO. And I say that because a rigid AFO does limit what your function is and especially in an awful lot of cases where we're looking after children who have both limbs affected, we may have to fit bilateral or two AFOs and too rigid AFOs can be quite debilitating. So, certainly when we're looking at providing an orthosis or we're assessing for an orthosis, the last thing we want to do is to actually make someone's situation more difficult. So, if someone is struggling with mobility, they're struggling with instability, they're struggling with standing, with sitting, with getting up stairs, what you just have to be careful you don't do is say, okay, on paper, this is what you need, but actually we're going to make your life harder. And a rigid AFO is one of those devices which can actually make life harder if it's not one, prescribed properly, and two, not fitted and designed properly. So, it's very important that we have an idea about what we're trying to do.
So, when might we use a rigid AFO? Someone who has tightness in their tendon Achilles or shortness in their gastrocnemius; a tendency to valgus or varus, so mediolateral instability, which we spoke earlier about; excessive dorsiflexion, which is probably a rather little more unusual one that we see. So, excessive dorsiflexion causes instability because you don't have stability in late-stance, in mid- to late-stance, and you tend to find then your knees will flex, your hips will flex, and it's a very energy consuming way and difficult way to mobilise. A slight tendency to flex at the knee, and again, this may go along with the excessive dorsiflexion, or it may be a crouch-type pattern that we see in our children with cerebral palsy. So, we can produce an extension moment through the rigidity of the AFO, which can affect the flexion at the knee.
Common conditions that we see are our cerebral palsy kids, our spina bifida kids, and adults with stroke, trauma, and often painful conditions where we're trying to perhaps block movements, so in arthritis where you have movement of a joint which causes pain, a rigid AFO stops that movement and will reduce the pain.
So, a little bit just, I had mentioned a GRAFO or a ground-reaction AFO earlier in the presentation and I used to have a slide where I used in some presentations which talked about GRAFOs, but I think the consensus now, and there is some research done on this, is that a GRAFO or a ground-reaction AFO is the same as a rigid AFO or a solid AFO. And the difference is that you attach what's called an anterior shell and what the anterior shell does is the anterior shell will spread the load, which is applied as part of our three-point pressure force system, which is applied to the front of the shin. So, effectively, we're trying to apply a force as part of our three-point pressure at the front of the shin to extend the knee and to maintain the ankle in a plantigrade position. So, a GRAFO, an AFO, a solid AFO, a rigid AFO all do the same thing because we are trying to influence the ground-reaction force.
And by its nature, a rigid AFO will influence the ground-reaction force. And if we move the ground-reaction force in front of the knee joint at mid-stance, we will create a hyperextension moment. If we move the ground-reaction force, or if the ground-reaction force remains behind the knee joint, we will create a flexion moment at mid-stance. And this is what we're always looking at when we're watching the patients walk if we do a gait analysis and what is the effect of the rigidity at the ankle? Is that what we want? Do we want to move the ground-reaction force forward? Do we want to move the ground-reaction force back? And that is part of the fitting of a rigid AFO.
So, it's important when we are deciding on the type of AFO that we look at the position that our patients can achieve. So, looking at muscle tightness as opposed to a fixed muscle tightness, as opposed to a dynamic muscle tightness. And again, this is most commonly seen in the likes of our cerebral palsy kids, or quite often in stroke, in multiple sclerosis where you have some level of spasticity. And if you have a tight muscle which is fixed, then usually you need to accommodate that muscle. And what that might mean is that the position of the ankle is not plantigrade. So, when you're designing your AFO, you have to then make a compensation for the fact that the foot is in an equinus position, or a plantarflexed position, so that when the user of the AFO is standing, that we have the ground-reaction force in the correct position, so we're not pushing the knee into hyperextension or pushing the knee into flexion.
If we have a more dynamic tightness where spasticity is kicking in, it's a little bit more difficult to manage because it's not there all the time. So, when you take your measurement for the AFO, the patient might be quite relaxed and you can get a nice plantigrade position, but when they actually go to walk in the AFO, they get an awful lot of pressure or because the dynamic tightness then appears as they move, they find that they've got an issue at their knee or at their hip because they don't have the muscle length. So, it's quite complex looking at all of the different positions and there is a lot more to AFOs than what you might think.
So, if we look at our valgus deformities, our mediolateral instabilities, where the rigid AFO we can apply that lovely three-point pressure force system. In our valgus deformities, commonly, we see rocker bottom feet, which are fairly fixed, but often need to be supported to reduce pain and also to prevent deterioration.
Hypermobility, we've spoken a little bit about, so where we have excessive dorsiflexion, and perhaps in a spina bifida or a neural tube defect child and we need to try and give them more stability by creating a more rigid base for them to stand on and to influence the ground-reaction force to allow their knees to be extended and their hips to extend. And also, the dynamic tightness that we spoke about can lead to an escape valgus where the hindfoot will escape into a valgus position because of the tightness in the tendon Achilles and this needs to be accommodated within a rigid AFO.
With varus deformities, I think it's fair to say that varus deformities are a little more difficult to correct. Even though we're using the same three-point pressure system to correct this, by their nature, they just tend to be a little bit more difficult to control. And often it involves some adaptation of, say, the foot plate on the AFO, but again, it's about assessing, is it a correctable deformity? If not, accommodate the deformity. If it's a fixed deformity, then accommodate the deformity. If it's a flexible deformity then correct to the optimum position, which will allow the patient to function within that rigid AFO.
We've said a lot about optimisation and optimal position and there is also an optimisation of the AFO once it has been manufactured and once has been fitted and that optimisation is done in conjunction with footwear. Footwear and AFOs go hand-in-hand. You can't walk with an AFO if you don't have suitable footwear, because it can be dangerous, it's slippy. So, we would always prescribe an AFO with a good type of footwear. And the footwear influences how the patient will function in the AFO. So, different types of shoes will have an influence on how the AFO influences then that patient's gait pattern. So, we tend to look at the footwear quite closely, and we tend to then optimise the angles of our AFO so that we can influence the ground-reaction force. And this is probably a little bit more technical for this presentation as an introduction, but also, I think important that we're aware of tuning or optimisation of our AFOs and an AFO footwear combination.
Prescription Criteria For A Rigid A.F.O.[edit | edit source]
- Tightness in T.A.
- Tendency to valgus
- Tendency to varus
- Excessive dorsiflexion
- Slight tendency to flexion at knee
Common Conditions[edit | edit source]
- CP
- NTD
- Stroke
- Trauma
- Pain
Rigid AFO +/- Anterior Shell[edit | edit source]
- Tightness in T.A.
- Tendency to valgus
- Tendency to varus
- Excessive dorsiflexion
- Crouch/ Flexion at knees
(Ries 2019)
Used for[edit | edit source]
- Muscle Tightness- Dynamic/Fixed
- Crouch/ Equinus
- Gait Hyper-extension/ Escape Valgus
- Valgus Deformities
- Rocker Bottom Foot
- Hyper-mobility
- Escape Valgus
- Compensatory movement
- Driven by tight TA
- Can alter foot structure
- Can result in long term issues
- Varus Deformities
- Correctable deformity
- Difficult to control
- Accommodate deformity
- Varus Deformity
- Crouch/Excessive Dorsiflexion
3. Jointed A.F.O.[edit | edit source]
The next type of AFO that we had noted is what's called the jointed AFO, and I like to think of a jointed AFO as somewhere in between our flexible AFO, which has no moving parts, but by its nature of its design and its trim lines is flexible using the type of materials that you have; and a rigid AFO, which is quite unforgiving and can be difficult for people to function in. With a jointed AFO, it's also useful in the optimisation that I just mentioned, where you can use certain types of joints to optimise that angle and to move the ground-reaction force in a controlled way. And it's quite a nice tool for us if we want to try and optimise someone's gait pattern. But, obviously, a joint by its design is about motion. And again, if you don't have a range of motion in your ankle and foot, then it's unlikely that an ankle joint is going to be useful. So, it's always good, again, to do your assessment and if you have a range of motion where an ankle joint might be useful, then it's always an option to put a joint in. You also then by its nature have the ability to apply that nice three-point force system where we can control mediolateral instability as well.
Some of the disadvantages of ankle joints are they tend to be bulkier. We spoke about footwear earlier on. Footwear can be quite a difficult problem for many of our AFO users because the AFO can be bulky and can be difficult to fit into shoes. So, if you add then another additional bulky item, such as an ankle joint, it can then become even more difficult. They can also be noisy. Because it's moving parts, they can break. And so, it's very important to weigh up the pros and cons of a jointed AFO versus a flexible or a rigid where you need to be sure that the advantages of the joints outweigh the disadvantages that the patient may experience. Obviously with that little bit of movement, stairs, getting up from a chair, and again, for the kids moving around the floor, it can be a really, really useful addition to AFO design.
Prescription Criteria For A Jointed A.F.O.[edit | edit source]
- ROM in ankle joint
- Tendency to valgus
- Tendency to varus
- Tendency to Crouch
Prescription criteria for Jointed AFO and DAFO/SMAFO[edit | edit source]
- Hyper mobile foot/ankle
- Ankle to plantargrade
- Medio-lateral instability
Tuning/ Optimising AFOs [edit | edit source]
o There is evidence that tuning AFOs can significantly improve gait and their effect at the proximal joints.
(Owen 2002, Stallard 2003, Butler 2007, Jagadamma 2009)
Tuning/ Optimising AFO’S - AFOFC
xxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxxx
At the beginning of the presentation, I also mentioned a couple of other different types of AFOs, a DAFO, or a dynamic AFO, and a SMAFO, or a supramalleolar AFO. And these are two other types of AFOs which we tend to see used mostly in our children, but they are also can be used in adults. And, usually, you're looking at a situation where you have a hypermobile or a very mobile foot and ankle. Generally, you're looking for a relatively neutral position, so no fixed contractures, and any ML or mediolateral instability can be quite well controlled within a DAFO or a SMAFO. Obviously, these tend to be shorter by nature, so they're not as long as a standard AFO, and by that nature, we've spoken a lot about the three-point pressure system, so if we have a shorter lever arm, we can't apply the same forces, so this is why they're most suited to the less tight patients. So, those who don't maybe have an underlying spasticity, or a very tight dynamic tightness into a certain position, but there certainly is a place for these and they can provide a lot of stability and at the same time allow good function for the patients.
In Conclusion