Disc Herniation
Original Editors Fauve simoens, Nele Postal
Top Contributors - Lucinda hampton, Andeela Hafeez, Chelsea Mclene, Fauve simoens, Admin, Liesa Rodet, Kim Jackson, Mariam Hashem, Teugels Amber, Nele Postal, Rachael Lowe, Simisola Ajeyalemi, Laura Ritchie, Fien Van Buggenhout, Kai A. Sigel, Evan Thomas, Lisa De Donder, Ellen Wynant, Lara Lagrange, Tony Lowe, Uchechukwu Chukwuemeka and Jess Bell - Your name will be added here if you are a lead editor on this page.
Definition/Description[edit | edit source]
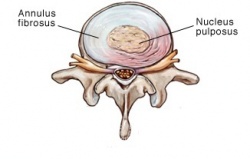
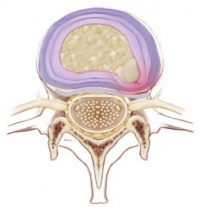
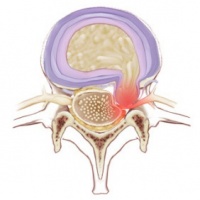
The herniation process begins from failure in the innermost annulus rings and progresses radially outward. The damage to the annulus of the disc appears to be associated with fully flexing the spine for a repeated or prolonged period of time. The nucleus loses its hydrostatic pressure and the annulus bulges outward during disc compression. [1]
Clinically Relevant Anatomy[edit | edit source]
There are many structures surrounding a discus intervertebralis: annulus fibrosus, anterior longitudinal ligament, posterior longitudinal ligament, nerve roots, nerves and muscles. A discus herniation can cause mechanical irritation of these structures which in turn can cause pain. This is presented as low back pain with possible radiculopathy if a nerve is affected.[2]
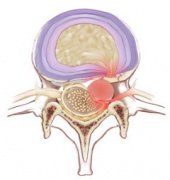
In the lumbar region, the level at which a disc herniates does not always correlate to the level of nerve root symptoms. When the herniation is in the posterolateral direction the affected nerve root is the one that exits at level below the disk herniation. This is because the nerve root at the hernia-level has already exited the transverse foramen. A foraminal herniation on the other hand affects the nerve root that is situated at the same level.
In the cervical region the herniated disc compresses the nerve actually exiting at that level.[2]
There are four types of herniated discs described in Clinical Anatomy and Management of Back Pain (2006)[3]:
Epidemiology /Etiology[edit | edit source]
Disc herniations are often asymptomatic, and 75% of the intervertebral disc herniations recover spontaneously within 6 months. In 95% of the lumbar disc herniations the L4-L5 and L5-S1 discs are most commonly affected. The cervical disc herniations are most locate at level C5-C6 and C6-C7. [2]
The most common direction for a disc herniation to occur is in the posterolateral direction, where the annulus fibrosis is thin and not supported by the anterior or posterior longitudinal ligament. [2] Chronic or sudden forcible hyperflexion or torsion can cause a disc hernia, but mostly there are no specific inciting events. Other possible causes can be a whiplash, poor posture, obesity smoking and occupational risks such as driving for a long time. [3][4]
Characteristics/Clinical Presentation[edit | edit source]
The arm pain from a cervical herniated disc results because the herniated disc material “pinches” or presses on a cervical nerve, causing pain to radiate along the nerve pathway down the arm. Along with the arm pain, numbness and tingling can be present down the arm and into the fingertips. Muscle weakness may also be present.[5]
Leg pain (also known as sciatica) is the most common symptom associated with a herniated disc in the lumbar spine. Approximately 90% of herniated discs occur at L4-L5 and L5-S1, causing pain in the L5 or S1 nerve that radiates down the sciatic nerve. Symptoms of a herniated disc at these locations are described below:
A herniated disc at lumbar segment 4 and 5 (L4-L5) usually causes L5 nerve impingement. In addition to sciatica pain, this type of herniated disc can lead to weakness when raising the big toe and possibly in the ankle, also known as foot drop. Numbness and pain can also be felt on top of the foot.[5]
Muscles served by the affected nerves tend to weaken. This may cause you to stumble, or impair your ability to lift or hold items.[6]
Differential Diagnosis[edit | edit source]
Mechanical pain[7]
Discogenic pain
Myofascial pain
Spondylosis/spondylolisthesis
Spinal stenosis
Abscess
Hematoma
Discitis/osteomyelitis
Mass lesion/malignancy
Myocardial infarction
Aortic dissection
Diagnostic Procedures[edit | edit source]
physical examination[edit | edit source]
Straight_Leg_Raise_Tes tis a test done during the physical examination to determine whether a patient with low back pain has an underlying herniated disk, often located at L5 (fifth lumbar spinal nerve).[8]
imagining[edit | edit source]
Imaging can be used to reveal disc herniations[2], note that most disc herniations are asymptomatic:
Plain X-rays don't detect herniated disks, but they may be performed to rule out other causes of back pain, such as an infection, tumor, spinal alignment issues or a broken bone.[9]
MRI_Scans This test can be used to confirm the location of the herniated disk and to see which nerves are affected
ACT scanner takes a series of X-rays from many different directions and then combines them to create cross-sectional images of your spinal column and the structures around it.[9]
Myelogram A dye is injected into the spinal fluid, and then X-rays are taken. This test can show pressure on your spinal cord or nerves due to multiple herniated disks or other conditions.
Nerve tests Electromyograms and nerve conduction studies measure how well electrical impulses are moving along nerve tissue. This can help pinpoint the location of the nerve damage.[9]
Outcome Measures[edit | edit source]
If the disc herniation is symptomatic different outcome measures can be used[10]:
Short Form-36 bodily pain (SF-36 BP)
Physical function scale (PF scores)
Oswestry disability index
Roland-Morris disability index
VAS-score
north american spine society score for neurologic symptoms[11]
Examination[edit | edit source]
See cervical or lumbar radiculopathy for the examination that can be used to assess if the radiant pain is caused by disc herniation.
Medical Management
[edit | edit source]
Over-the-counter pain medications. If your pain is mild to moderate, your doctor may tell you to take an over-the-counter pain medication, such as ibuprofen (Advil, Motrin IB, others) or naproxen (Aleve, others).
Narcotics. If your pain doesn't improve with over-the-counter medications, your doctor may prescribe narcotics, such as codeine or an oxycodone-acetaminophen combination (Percocet, Oxycontin, others), for a short time. Sedation, nausea, confusion and constipation are possible side effects from these drugs.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Nerve pain medications. Drugs such as gabapentin (Neurontin, Gralise, Horizant), pregabalin (Lyrica), duloxetine (Cymbalta), tramadol (Ultram) and amitriptyline often help relieve nerve-damage pain. Because these drugs have a milder set of side effects than do narcotic medications, they're increasingly being used as first line prescription medications for people who have herniated disks.
Muscle relaxers. Muscle relaxants may be prescribed if you have muscle spasms. Sedation and dizziness are common side effects of these medications.
Cortisone injections. Inflammation-suppressing Therapeutic Corticosteroid Injection may be given directly into the area around the spinal nerves. Spinal imaging can help guide the needle more safely. Occasionally a course of oral steroids may be tried to reduce swelling and inflammation.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
A very small number of people with herniated disks eventually need surgery. Your doctor may suggest surgery if conservative treatments fail to improve your symptoms after six weeks, especially if you continue to experience:
Numbness or weakness
Difficulty standing or walking
Loss of bladder or bowel control
In many cases, surgeons can remove just the protruding portion of the disk. Rarely, however, the entire disk must be removed. In these cases, the vertebrae may need to be fused together with metal hardware to provide spinal stability. Rarely, your surgeon may suggest the implantation of an artificial disk.Cite error: Invalid <ref> tag; name cannot be a simple integer. Use a descriptive title
Surgical Treatment[edit | edit source]
Only a small percentage of patients with lumbar disk herniations require surgery. Spine surgery is typically recommended only after a period of nonsurgical treatment has not relieved painful symptoms.
Microdiskectomy. The most common surgical procedure for a herniated disk in the lower back is a lumbar microdiskectomy. Microdisketomy involves removing the herniated part of the disk and any fragments that are putting pressure on the spinal nerve.[12]
Physical Therapy Management[edit | edit source]
<u</u>Physical therapy often plays a major role in herniated disc recovery. Its methods not only offer immediate pain relief, but they also teach you how to condition your body to prevent further injury.[13]
There are a variety of physical therapy techniques
Deep Tissue Massage: There are more than 100 types of massage, but deep tissue massage is an ideal option if you have a herniated disc because it uses a great deal of pressure to relieve deep muscle tension and spasms, which develop to prevent muscle motion at the affected area.
Hot and cold therapies offer their own set of benefits, and your physical therapist may alternate between them to get the best results.
Your physical therapist may use heat to increase blood flow to the target area. Blood helps heal the area by delivering extra oxygen and nutrients. Blood also removes waste byproducts from muscle spasms.[13]
Conversely, cold therapy (also called cryotherapy) slows circulation. This reduces inflammation, muscle spasms and pain. Your physical therapist may place an ice pack on the target area, give you an ice massage, or even use a spray known as fluoromethane to cool inflamed tissues.
Hydrotherapy: As the name suggests, hydrotherapy involves water. As a passive treatment, hydrotherapy may involve simply sitting in a whirlpool bath or warm shower. Hydrotherapy gently relieves pain and relaxes muscles.
Transcutaneous electrical nerve stimulation (TENS): A TENS machine uses an electrical current to stimulate your muscles. It sounds intense, but it really isn't painful. Electrodes taped to your skin send a tiny electrical current to key points on the nerve pathway. TENS reduces muscle spasms and is generally believed to trigger the release of endorphins, which are your body's natural pain killers.
Traction: The goal of traction is to reduce the effects of gravity on the spine. By gently pulling apart the bones, the intent is to reduce the disc herniation. The analogy is much like a flat tire "disappearing" when you put a jack under the car and take pressure off the tire. It can be performed in the cervical or lumbar spine.[13]
Core stability: Many people don't realize how important a strong core is to their spinal health. Your core (abdominal) muscles help your back muscles support your spine. When your core muscles are weak, it puts extra pressure on your back muscles. Your physical therapist may teach you core stabilizing exercises to strengthen your back.
Flexibility: Learning proper stretching and flexibility techniques will prepare you for aerobic and strength exercises. Flexibility helps your body move easier by warding off stiffness[13].
Muscle strengthening: Strong muscles are a great support system for your spine and better handle pain
Rehabilitation interventions with postoperative lumbar disc hernia
The first thing to do when patients come out of the surgery, is to give information about the rehabilitation program they will follow the next few weeks. The patients are instructed and accompanied in daily activities such as: coming out of bed, going to the bathroom and clothing. Besides all this the patients have to pay attention on the ergonomics of the back throughout back school.[14][15][16][17]
Most studies start their rehabilitation program 4-6 weeks postsurgery. In the meantime, the patients were followed on the above mentioned instructions.[17] Unlike, the most important goals of the rehabilitation of other peripheral joints, namely: regaining strength and range of motion; the most important goal of the rehabilitation of the low back is to improve the patients’ health. Regaining strength and range of motion are commonly used wrong as most important goals of the low back rehabilitation because of the influence from the athletic world and sport rehabilitation. These goals increase the risk for more back problems.[1]
During back rehabilitation of postoperative disc hernia it is important to regain core stability first. The ‘ corset ‘ of the lumbar spine -formed by the abdominal and back muscles- has to be rebuild. Maintaining this corset is important during various movements, activities and several situations.[14][15][1][16][17] Keeping this in mind it is self-evident that the endurance of these muscles have to be trained too. Endurance of the muscles participating in the core stability are educated in a neutral position of the upper body/back due to start with short term repetitions that shift into long term repetitions. The exercises that are given in the beginning are subsequently performed in different positions and with several arm and leg movements.[1][16]
A few studies mention stretching of shortened muscles, such as Hamstrings and Quadriceps.[14][15] Hip flexion restriction seem not to be linked with any back pain and maybe unnecessary if the goal is just solving back problems. Eventually if Hamstrings and Quadriceps are shortened, restricted functioning of the hip may occur. For this reason stretching is necessary to regain full function of the hip.[1]
If core stability is totally regained and fully under control, strength and power can be trained. But only when this is necessary for the patients functioning/activities. This power needs to be avoided during the core stability exercises because of the combination of its two components: force and velocity. This combination forms a higher risk to gain back problems and back pain.[1]
Various studies have shown that a treatment with accompaniment of a physical therapist or a multi-disciplinary treatment have a positive effect on the regularity of doing the exercises and the rapidity of return-to-work.[14][16][17] A high intensity program gains faster results as a low intensity program, but the results are the same in the end.[16] During the rehabilitation the patients have to be supported to restart and preserve their daily activities; active coping has to be stimulated. Guiding and instructing the patients are of great importance during the treatment/rehabilitation.[14][1][17]
Key Research[edit | edit source]
add links and reviews of high quality evidence here (case studies should be added on new pages using the case study template)
Resources
[edit | edit source]
http://www.isass.org/h/patient_resources_spine_conditions.html
http://orthoinfo.aaos.org/topic.cfm?topic=a00534
https://my.clevelandclinic.org/health/diseases_conditions/hic_Herniated_Disc
https://www.spine.org/Portals/0/Documents/ResearchClinicalCare/Guidelines/LumbarDiscHerniation.pdf
Clinical Bottom Line[edit | edit source]
add text here
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
see adding references tutorial.
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 McGill, S. (2007). Low Back Disorders: Evidence Based Prevention and Rehabilitation, Second Edition. USA: Human Kinetics.
- ↑ 2.0 2.1 2.2 2.3 2.4 Lena Shahbandar and Joel Press. Diagnosis and Nonoperative Management of Lumbar Disk Herniation.fckLROperative Techniques in Sports Medicine, 2005; 13: 114-121
- ↑ 3.0 3.1 L. G. F. Giles, K. P. Singer. The Clinical Anatomy and Management of Back Pain. Butterworth-Heinemann, 2006.
- ↑ Pradeep Suri, David J. Hunter, Cristin Jouve. Inciting events associated with lumbar disc herniation.fckLRThe Spine Journal, 2010; 10: 388–395
- ↑ 5.0 5.1 http://www.spine-health.com/conditions/herniated-disc/typical-symptoms-a-herniated-disc
- ↑ http://www.mayoclinic.org/diseases-conditions/herniated-disk/basics/symptoms/con-20029957
- ↑ https://en.wikipedia.org/wiki/Spinal_disc_herniation
- ↑ https://en.wikipedia.org/wiki/Straight_leg_raise
- ↑ 9.0 9.1 9.2 http://www.mayoclinic.org/diseases-conditions/herniated-disk/basics/tests-diagnosis/con-20029957
- ↑ Wayne Moschetti, Adam M. Pearson, and William A. Abdu. Treatment of Lumbar Disc Herniation: An Evidence-Based Review.fckLRSeminars Spine Surgery, 2009; 21: 223-229
- ↑ https://www.duo.uio.no/bitstream/handle/10852/28055/dravhandling-haugen.pdf?sequence=3
- ↑ http://orthoinfo.aaos.org/topic.cfm?topic=a00534
- ↑ 13.0 13.1 13.2 13.3 http://www.spineuniverse.com/conditions/herniated-disc/physical-therapy-herniated-discs
- ↑ 14.0 14.1 14.2 14.3 14.4 Ann-Christin Johansson, S. J. (2009). Clinic-based training in comparison to home-based training after first-time lumbar disc surgery: a randomised controlled trial. Eur Spine Journal , 398-409.
- ↑ 15.0 15.1 15.2 Cele B. Erdogmus, K.-L. R. (2007 Vol.32 Nr.19). Physiotherapy-Based Rehabilitation Following Disc Herniation Operation. Spine , 2041-2049.
- ↑ 16.0 16.1 16.2 16.3 16.4 Mustafa Filiz, A. C. (2005). The effectiveness of exercise programmes after lumbar disc surgery: a randomised controlled trial. Clinical Rehabilitation , 4-11.
- ↑ 17.0 17.1 17.2 17.3 17.4 Raymond W. J. G Ostelo, L. O. (2009). Rehabilitation After Lumbar Disc Surgery: An update Cochrane Review. Spine Vol. 34 Nr. 17 , 1839 - 1848.