Chronic Bronchitis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 38: | Line 38: | ||
== Pathophysiology == | == Pathophysiology == | ||
[[File:Maxresdefault1.jpg|300x300px|alt=|right|frameless]]Chronic bronchitis is thought to be caused by overproduction and hypersecretion of mucus by goblet cells. Epithelial cells lining the airway response to toxic, infectious stimuli by releasing inflammatory mediators and eg pro-inflammatory [[cytokines]]. | [[File:Maxresdefault1.jpg|300x300px|alt=|right|frameless]]Chronic bronchitis is thought to be caused by overproduction and hypersecretion of mucus by goblet cells. Epithelial cells lining the airway response to toxic, infectious stimuli by releasing inflammatory mediators and eg pro-inflammatory [[cytokines]]. | ||
During an acute exacerbation of chronic bronchitis, the bronchial mucous membrane becomes hyperemic and edematous with diminished bronchial mucociliary function. This, in turn, leads to airflow impediment because of luminal obstruction to small airways. The airways become clogged by debris and this further increases the irritation. The characteristic cough of bronchitis is caused by the copious secretion of mucus in chronic bronchitis.<ref name=":0" />[[File:Goblet cells.gif|right|frameless|370x370px]]Image 2: Pseudostratified epithelium, highlighting the pseudostratified epithelial cells, goblets cells (shown in blue), then underlying connective tissue | |||
During an acute exacerbation of chronic bronchitis, the bronchial mucous membrane becomes hyperemic and edematous with diminished bronchial mucociliary function. This, in turn, leads to airflow impediment because of luminal obstruction to small airways. The airways become clogged by debris and this further increases the irritation. The characteristic cough of bronchitis is caused by the copious secretion of mucus in chronic bronchitis.<ref name=":0" /> | |||
Image 2: Pseudostratified epithelium, highlighting the pseudostratified epithelial cells, goblets cells (shown in blue), then underlying connective tissue | |||
* Smokers with moderate COPD and CB had a greater number of goblet cells in their peripheral airways<ref name="Kim and Criner" />, which increases the potential of mucus in the lungs (a greater number of small airways were blocked with mucus increases the severity of the disease).<ref name="Kim and Criner" /> | * Smokers with moderate COPD and CB had a greater number of goblet cells in their peripheral airways<ref name="Kim and Criner" />, which increases the potential of mucus in the lungs (a greater number of small airways were blocked with mucus increases the severity of the disease).<ref name="Kim and Criner" /> | ||
| Line 47: | Line 44: | ||
== Clinical Manifestations == | == Clinical Manifestations == | ||
[[File:Bronchitis.jpg|right|frameless]] | |||
The clinical presentation can be an increased exacerbation rate, accelerated decline in lung function, worse health-related quality of life and an increase in mortality.<ref name="Kim and Criner" /> Common symptoms outlined by the British Lung Foundation include<ref name="British Lung Foundation" />: | The clinical presentation can be an increased exacerbation rate, accelerated decline in lung function, worse health-related quality of life and an increase in mortality.<ref name="Kim and Criner" /> Common symptoms outlined by the British Lung Foundation include<ref name="British Lung Foundation" />: | ||
*Wheezing, particularly breathing out | *Wheezing, particularly breathing out | ||
Revision as of 07:56, 24 May 2021
Original Editors - Students from Glasgow Caledonian University's Cardiorespiratory Therapeutics Project.
Top Contributors - Lindsey Chisholm, Kelly D'Autremont, Lucinda hampton, Kim Jackson, Esraa Mohamed Abdullzaher, Admin, Evan Thomas, Uchechukwu Chukwuemeka, Michelle Lee, WikiSysop and Fasuba Ayobami
Definition/Description[edit | edit source]
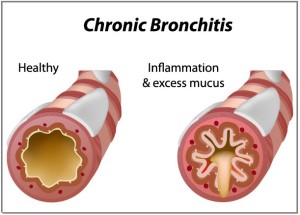
Chronic Bronchitis (CB) is defined as a chronic cough and sputum production for at least 3 months a year for 2 consecutive years. [1]
It is covered under the umbrella term of Chronic Obstructive Pulmonary Disease (COPD). The COPD spectrum ranges from Emphysema to Chronic Bronchitis. Many patients have characteristics of both, putting them somewhere along the spectrum.[1]
- CB is the inflammation and excessive mucus build-up in the bronchi.[2]
- Emphysema occurs when the alveolar membrane breaks down .
The prevalence of the disease has a great impact on society and on health care systems around the world.
Epidemiology[edit | edit source]
The occurrence of Chronic bronchitis
- In the general population has been documented to vary between 3% to 7% of healthy adults.
- It is estimated to be as high as 74% among those diagnosed to have COPD.
Subjects under the age of 50 years who are otherwise healthy and have chronic bronchitis are at a higher risk of morbidity and mortality when compared to healthy subjects.
The increasing prevalence of chronic bronchitis is thought to be associated with increasing age, tobacco smoking, occupational exposure, and socioeconomic status.[3]
Etiology[edit | edit source]
There are many known causes of chronic bronchitis.
The most important causative factor is exposure to cigarette smoke either due to active smoking or passive inhalation. Other causes include:
- Inhaled irritants to the respiratory tract eg smog, industrial pollutants, airborne chemicals (eg ammonia and sulfur) can cause chronic bronchitis.
- Repeated exposure to viral infections can cause chronic bronchitis.
- People with an associated background in respiratory diseases eg asthma, cystic fibrosis, or bronchiectasis have a higher predisposition to develop chronic bronchitis.
- Chronic gastroesophageal reflux is a well documented but less frequent cause of chronic bronchitis[3].
- There is also a genetic factor associated with COPD, it is a deficiency in alpha-1-antitrypsin. This genetic marker is indicative of Emphysema, but many patients on the COPD spectrum have characteristics of both Emphysema and CB.[2]
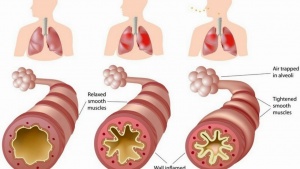
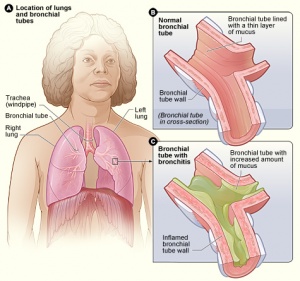
Pathophysiology[edit | edit source]
Chronic bronchitis is thought to be caused by overproduction and hypersecretion of mucus by goblet cells. Epithelial cells lining the airway response to toxic, infectious stimuli by releasing inflammatory mediators and eg pro-inflammatory cytokines. During an acute exacerbation of chronic bronchitis, the bronchial mucous membrane becomes hyperemic and edematous with diminished bronchial mucociliary function. This, in turn, leads to airflow impediment because of luminal obstruction to small airways. The airways become clogged by debris and this further increases the irritation. The characteristic cough of bronchitis is caused by the copious secretion of mucus in chronic bronchitis.[3]
Image 2: Pseudostratified epithelium, highlighting the pseudostratified epithelial cells, goblets cells (shown in blue), then underlying connective tissue
- Smokers with moderate COPD and CB had a greater number of goblet cells in their peripheral airways[1], which increases the potential of mucus in the lungs (a greater number of small airways were blocked with mucus increases the severity of the disease).[1]
- Mucus hypersecretion is one of the risks associated with cigarette smoke exposure, viral infections, bacterial infections, or inflammatory cell activation. When combined with poor ciliary function, distal airway occlusion, ineffective cough, respiratory muscle weakness, and reduced peak expiratory flow clearing secretions is extremely difficult and requires high energy consumption. [1]
Clinical Manifestations[edit | edit source]
The clinical presentation can be an increased exacerbation rate, accelerated decline in lung function, worse health-related quality of life and an increase in mortality.[1] Common symptoms outlined by the British Lung Foundation include[2]:
- Wheezing, particularly breathing out
- Breathlessness when resting or active
- Tight chest
- Cough
- Producing more mucus or phlegm than usual
These symptoms would be persistent for at least 3 months a year for 2 consecutive years to be considered Chronic Bronchitis.[1]
Evaluation[edit | edit source]
The most critical factor in the diagnosis of chronic bronchitis is a typical history to exclude other possible diseases of the lower respiratory tract.
The investigations which assist in confirming the diagnosis of chronic bronchitis are:
- Blood test: This is to see if your symptoms could be due to anemia, or to see if the symptoms are due to the genetic marker alpha-1-antitrypsin deficiency.[4]
- A chest x-ray in the elderly and when physical findings suggest pneumonia is important.
- A culture of the sputum when a bacterial infection is suspected is indicated.
- The additional investigations which are a helpful measurement of oxygen saturation, and pulmonary function tests eg spirometry[3]
Physiotherapy and Other Management[edit | edit source]
The treatment of CB may include a variety of interventions including management through medications, education, physical exercise, and respiratory exercises. The goal of the physiotherapist should involve education, improve exercise tolerance, reduce exacerbations and hospitalization, assist in sputum clearance, and increase thoracic mobility and lung volume.
Medication[edit | edit source]
There are various kinds of short term and long term medications individuals with CB might take to reduce flare-ups, decrease obstruction, improve activity and decrease shortness of breath. These medications may include bronchodilators, corticosteroids, and antibiotics.[6]
Exercise[edit | edit source]
Regular exercise can have positive effects on the management, treatment, and prevention of CB and COPD. Aerobic exercise and upper & lower limb resistance training have shown positive changes in the reduction of airflow obstruction, clearing of airways, improved functional capabilities increased energy levels, and sputum expectoration. Exercise programs should be under the supervision of the treating clinical team and a discussion with the general practitioner should be had before taking part in any exercise program.[7]
Postural Drainage[edit | edit source]
The use of various positions to assist in the expectoration of sputum by using gravity to move sputum towards the throat and mouth. Is can be used with other treatment techniques. These positions can be modified for each client's condition and preferences. Ideally, the client is placed in a position where the affected area is higher than the unaffected area.[6]
Active Cycle of Breathing[edit | edit source]
Consists of the combination of Controlled Breathing, Thoracic Expansion Exercises, and “The Huff” or Force Expiration Exercises at different lung volumes. Can be used to reduce bronchospasms, coughing, airway obstruction, and promote collateral airway ventilation and sputum expectoration. This technique can be modified to the needs of the client and their preferences.[6]
Autogenic Drainage[edit | edit source]
This technique allows for larger airflow in the bronchi without causing a collapse of the airway with proper breathing. This has been shown to promote sputum expectoration, collateral airway airflow, and a reduction in carbon dioxide retention. Similar to the Active Cycle of Breathing this technique can be modified to the needs of the client and their preferences[6]
Percussion and Vibrations[edit | edit source]
Usually used in conjunction with postural drainage. The theory behind the use of percussions and vibrations is that it will assist with the clearing of sputum stuck on the airways. There is little evidence of this effect however, some clients do believe it helps with sputum expectoration. Percussion is the rhythmic clapping on the chest or back of the client with a loose wrist and cupped hands. The clapping should be soothing and relaxing to the client, each client may have their own personal preference. Vibrations consist of while the therapist's hands are against the client's chest or back performing fine movements of the hands, down and inwards, while the client is exhaling after a large breath. [6]
Education[edit | edit source]
Education of the individual with CB by the treating clinical staff in terms of the presenting condition, medication use, treatment options, and self-management may help the psychological effects associated with having a chronic condition and promote a proactive approach to management. [6]
Prevention[edit | edit source]
There is presently no cure for CB. However, with lifestyle changes, education, and proper management it is possible to prevent exacerbations of the condition.
Stopping Smoking[edit | edit source]
Smoking can irritate the lungs leading to irritation, inflammation, and scar. The longer an individual smokes the more damage occurs to the lungs which can lead to increased amounts of exacerbations of the condition. By quitting smoking this can decrease the number of exacerbations, hospital visits and lead to a better quality of life.[11]
Physical Fitness[edit | edit source]
Aerobic exercise and upper & lower limb resistance training have the ability to increase physical fitness, functional tolerance, energy levels, and decrease concern over the shortness of breath, exacerbations, and hospital visits. Specific guidelines are put in place in concern to exercise for individuals with chronic bronchitis and COPD. The Discussion should be held with the treating clinical team before participation in any exercise program begins. [7]
Avoiding Irritants[edit | edit source]
Being aware of possible irritants within the household, workplace, and places of recreation can help reduce risk factors associated with chronic bronchitis and reduce exacerbations. Irritants to be aware of can include dust, chemicals, vapors, air pollution, and smoke. Proper respiratory protective equipment should be made readily available if contact with irritants in the workplace commonly occurs. [12]
Practice Proper Hygiene[edit | edit source]
Practicing good hygiene can reduce the spread of germs, bacteria, and infections. This can help reduce the risk factors associated with bronchitis and help reduce exacerbations of chronic bronchitis.[11]
Education[edit | edit source]
Education can play a vital aspect in the prevention and management of CB. Education about the presenting condition, risk factors associated with it, and treatment can help reduce anxiety associated with the development of any chronic condition, and a proper understanding of the condition and how to manage it can encourage the individual to take a proactive approach to their management program.[6]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 Kim V, Criner GJ. Chronic Bronchitis and Chronic Obstructive Pulmonary Disease. Am J Respir Crit Care Med 2013;187:228-237
- ↑ 2.0 2.1 2.2 British Lung Foundation. COPD: Chronic obstructive pulmonary disease. Available from: http://www.blf.org.uk/Page/chronic-obstructive-pulmonary-disease-COPD (accessed 4 May 2015).
- ↑ 3.0 3.1 3.2 3.3 Widysanto A, Mathew G. Chronic Bronchitis. StatPearls [Internet]. 2020 Aug 23.Available from: https://www.ncbi.nlm.nih.gov/books/NBK482437/?report=reader(accessed 24.5.2021)
- ↑ National Health Services. Chronic Obstructive pulmonary disease. Available from: http://www.nhs.uk/Conditions/Chronic-obstructive-pulmonary-disease/Pages/Introduction.aspx (accessed 4 May 2015)
- ↑ The European Lung Foundation. Spirometry: how to take a lung function test. https://www.youtube.com/watch?v=6kbgZWS5wH0 [last accessed 5/6/15]
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 Hough A. Respiratory Disorders. Physiotherapy In Respiratory And Cardiac Care: An Evidence-Based Approach. Fourth ed. Cenegage Learning; 2014. p77-84.
- ↑ 7.0 7.1 Dressendorfer R, Haykowsky M, Eves N. Exercise for Persons with Chronic Obstructive Pulmonary Disease. Available from: http://www.acsm.org/docs/current-comments/exerciseforpersonswithcopd.pdf. (Accessed 6 May 2015).
- ↑ faisal alg. Postural Drainage. https://www.youtube.com/watch?v=TPZsP1ujg0U. [last accessed 6/5/15]
- ↑ Derriford Hospital NHS Physiotherapy. Active Cycle of Breathing. https://www.youtube.com/watch?v=XvorhwGZGm8. [last accessed 22/9/19]
- ↑ enmurrcp. RT Chest Physiotherapy Demonstration. https://www.youtube.com/watch?v=ErMTXJLE5es. [last accessed 6/6/15]
- ↑ 11.0 11.1 National Health Services. Bronchitis. 14/07/2014; Available from: http://www.nhs.uk/conditions/Bronchitis/Pages/Introduction.aspx. (Accessed 6 May 2015).
- ↑ Mayo Clinic Staff. Diseases and Conditions. COPD Prevention. 2014. Available from: http://www.mayoclinic.org/diseases-conditions/copd/basics/prevention/CON-20032017. Accessed 6 May 2015).