Cervical Myelopathy
Original Editors - Bridgit A Finley and Stefanie Van De Vijver
Top Contributors - Laura Ritchie, Rachael Lowe, Bridgit A Finley, Stefanie Van De Vijver, Kim Jackson, Admin, Evan Thomas, Vidya Acharya, Loes Verspecht, Lise Buelens, Dale Boren, Manisha Shrestha, Bram Van Laer, Lucinda hampton, Simisola Ajeyalemi, Jess Bell, Olajumoke Ogunleye, Aminat Abolade, Naomi O'Reilly, Habibu Salisu Badamasi, Ilke Joukes, Kai A. Sigel, Scott Cornish, WikiSysop, Karen Wilson and Timothy Assi
1. Search strategy
We searched Pubmed, Pedro, Web of Science,... These are the key words we used during our search:
- Spinal cord compression-Cervical spinal cord-Examination
- Cervical myelopathy-Muscle strength-Evaluation
- Cervical myeolopathy-Traction-Prevention
- Physical therapy-Physical management
2. Definition/Description
Cervical myelopathy is the result of spinal cord compression in the cervical spine. Any space occupying lesion within the cervical spine with the potential to compress the spinal cord can result in this degenerative disease.[1][2] (LoE:5, LoR:2b)Cervical myelopathy is predominantly due to pressure on the anterior spinal cord with ischaemia as a result of deformation of the cord by anterior herniated discs, spondylitic spurs or an ossified posterior longitudinal ligament.[3] (LoE:2b)Human histological studies have revealed degeneration of the anterior horns, cavity formation, and demyelination in the severely compressed spinal cord. The spontaneous course of myelopathy is characterized either by long periods of stable disability followed by episodes of deterioration or a linear progressive course. The presentation of a cervical myelopathy varies in accordance to the severity of the spinal cord compression as well as its location.[4] (LoE:5)
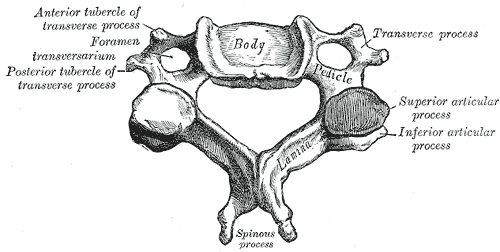
3. Clinically Relevant Anatomy
There are seven cervical vertebrae and eight cervical nerve roots.[2][5] The spinal cord is the extension of the central nervous system outside the cranium. It is encased by the vertebral column and begins at the foramen magnum.[6] The spinal cord is an extremely vital part of the central nervous system, and even a small injury can lead to severe disability.[7]
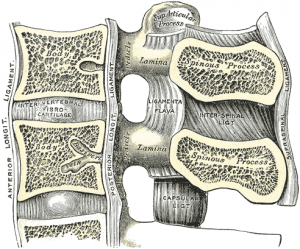
A complex system of ligaments serves to stabilize and protect the cervical spine. For example, ligamentum flavum extends from the anterior surface of the cephalic vertebra to the posterior surface of the caudal vertebra and connects to the ventral aspect of the facet joint capsules. A ligament that is often involved in this condition is the posterior longitudinal ligament. It is situated within the vertebral canal, originating from the body of the axis, where it is continuous with the membrana tectoria, and extends along the posterior surfaces of the bodies of the vertebrae until inserting into the sacrum.[7]
Chronic cervical degeneration is the most common cause of progressive spinal cord and nerve root compression. Spondylotic changes can result in stenosis of the spinal canal, lateral recess, and foramina. Spinal canal stenosis can lead to myelopathy, whereas the latter two can lead to radiculopathy.
Cervical spine myelopathy resulting from sagittal narrowing of the spinal canal and compression of the spinal cord is present in 90% of individuals by the seventh decade of life.[8]
4. Epidemiology /Etiology
Cervical spondylotic myelopathy is the most common disorder of the spinal cord in persons older than 55 years of age.[5][9][10] Radiologic spondylotic changes increase with patient age - 90% of asymptomatic persons older than 70 years have some form of degenerative change in the cervical spine. Both sexes are affected equally. Cervical spondylosis usually starts earlier in men (50 years) than in women (60 years). It causes hospitalization at a rate of 4.04 per 100,000 person-years.[5][11]
The causes of cervical myelopathy can be divided into different categories:
- Static factors: A narrowing of the spinal canal size can result from disc degeneration, spondylosis, stenosis, osteophyte formation at the level of facet joints, segmental ossification of the posterior longitudinal ligament and yellow ligament hypertrophy, calcification or ossification. Patients with a congenitally narrow spinal canal (<13mm) have a higher risk for the development of symptomatic cervical myelopathy.[4][11][12]
- Dynamic factors: Due to mechanical abnormalities of the cervical spine or instability.[4]
- Vascular and cellular factors: Spinal cord ischemia affects oligodendrocytes, which results in demyelination exhibiting features of chronic degenerative disorders. Also glutamatergic toxicity, cell injury and apoptosis may occur.[4]
[[Mechanism of Injury / Pathological Process
]]
The onset is insidious and gradual, which is related to degenerative changes in the cervical spine anatomy. Osteophytic overgrowth, thickening of the ligamentum flavum (dorsally) and of the posterior longitudinal ligament can compress the spinal cord. The intervertebral discs dry out resulting in loss of disc height, which increases compression of the vertebral end plates and osteophytic spurs develop at the margins of the end plates. The degenerative changes encroach on the spinal cord and cause compression.
According to Cook et al[8] cord compression may occur from:
- osteophytes secondary to degeneration of intervertebral joints
- stiffening of connective tissues, such as the ligamentum flavum at the dorsal aspect of the spinal canal, which can impinge on the cord by "buckling" when the spine is extended
- degeneration of the intervertebral discs together with subsequent bony changes
- other connective tissue changes
Cord compression is thought to be a combination of static compression and intermittent dynamic compression from cervical motion (flexion/extension).
5. Characteristics and Clinical Presentation
Cervical spondylotic myelopathy can cause a variety of signs and symptoms. Symptoms are divided into two groups: long-tract and segmental symptoms. Onset is insidious, typically in persons aged 50-60 years.
Early symptoms of this condition are ‘numb, clumsy, painful hands’ and disturbance of fine motor skills.[4] Weakness and numbness occur in a non-specific/non-dermatomal pattern. As spinal cord degeneration progresses, lower motor neuron findings in the upper extremities, such as loss of strength, atrophy of the interosseous muscles and difficulty in fine finger movements, may present. Additional clinical findings may include: neck pain and stiffness (decreased ROM, especially extension), shoulder and scapular pain, paresthesia in one or both arms or hands, signs of radiculopathy, Babinski and Hoffman's sign, ataxia and dexterity loss.[5][13][14] Typical neurological signs of long-tract involvement are exaggerated tendon reflexes (patellar and achilles), presence of pathological reflexes (e.g. clonus, Babinski and Hoffman's sign), spastic quadriplegia, sensory loss and bladder-bowel disturbance.[12]
Once the disorder is diagnosed, complete remission to normality never occurs and spontaneous temporary remission is uncommon. In 75% of the patients, episodic worsening with neurological deterioration occurs, 20% have slow steady progression, and 5% experience rapid onset and progression.[4]
- Distal weakness
- Decreased ROM in the cervical spine, especially extension.
- Clumsy or weak hands
- Pain in shoulder or arms
- Unsteady or clumsy gait
- Increased reflexes in the lower extremities and in the upper extremities below the level of the lesion.
- Numbness and parasthesia in one or both hands
- Radiculopathic signs
6. Differential Diagnosis
- Adhesive Capsulitis
- Brown-Sequard Syndrome
- Carpal Tunnel Syndrome
- Central Cord Syndrome
- Cervical Disc Disease
- Cervical Myofascial Pain
- Cervical Sprain and Strain
- Chronic Pain Syndrome
- Diabetic Neuropathy
- Multiple Sclerosis
- Myofascial Pain
- Neoplastic Brachial Plexopathy
- Osteoporosis
- Spinal Cord Injury
- Radiation-Induced Brachial Plexopathy
- Rheumatoid Arthritis
- Traumatic Brachial Plexopathy
- Tumors
7. Diagnostic Procedures
A detailed and thorough neurological examination is the current standard to diagnose the presence of cervical myelopathy. A magnetic resonance image (MRI) is considered the best imaging method for confirming the presence of cervical stenosis, cord compression, or myelomalacia, elements germane to cervical spine myelopathy.
The diagnosis of CSM is primarily based on the clinical signs found on physical examination and is supported by imaging findings of cervical spondylosis with cord compression.[9] According to Cook et al,[15] selected combinations of the following clinical findings are effective in ruling out and ruling in cervical spine myelopathy. Combinations of three of five or four of five of these tests enable post-test probability of the condition to 94–99%:
- gait deviation
- +ve Hoffmann’s test
- inverted supinator sign
- +ve Babinski test
- age 45 years or older
Other clinical examination tests often used for myelopathy include:[5][9]
- Spurling’s test
- Distraction test
- +ve clonus/Babinski/Hoffman's
- Hyperreflexic biceps
- Hyperreflexic quadriceps
- Hyperreflexic achilles
- Pain constancy
- L’hermitte’s sign
- Romberg test
Although these tests exhibit moderate to substantial reliability among skilled clinicians, they demonstrate low sensitivity and are not appropriate for ruling out myelopathy. One method used to improve the diagnostic accuracy of clinical testing is combining tests into clusters. These often overcome the inherent weakness of stand alone tests.[5][15]
Plain radiographs alone are of little use as an initial diagnostic procedure. MRI of the cervical spine can identify spinal canal stenosis, as well as rule out spinal cord tumors.
An MRI is most useful because it expresses the amount of compression placed on the spinal cord and demonstrates relatively high levels of sensitivity and specificity. [5] [13] Anterior-posterior width reduction, cross-sectional evidence of cord compression, obliteration of the subarachnoid space and signal intensity changes to the cord found on MR imaging are considered the most appropriate parameters for confirmation of a spinal cord compression myelopathy. [5] More than half of patients with cervical spine myelopathy show intramedullary high signal intensity on T2-weighted imaging, mainly in the spinal gray matter. [16] Radiographic cervical spinal cord compression and hyperintense T2 intraparenchymal signal abnormalities (MRI) correlate well with the presence of myelopathic findings on physical examination[17].
8. Outcome Measures
• Neck disability index
• Neck pain and disability scale
• Nurick-score [18]
• Japanese-orthopaedic-association-score (JOA-Score) [18] [19]
• Cooper-myelopathy-scale (CMS) [18]
• European-myelopathy-score (EMS)
'9. Examination
Below we discus some of the tools a physiotherapist can use when a patient with cervical myelopathy walks in. It's important to look at the reflexes, muscle strength, sensitivity, but as a physiotherapist we should also look at the patients wellbeing, activity's and participation. Therefore, we can use some questionnaires. Above, under diagnostic procedures, some clinical examination tests are also described.
9.1 Inspection
- Kyfosis: Debrunner kyphometer, Spinal Mouse and Flexicurve index have the highest reliability[20]. - Posture
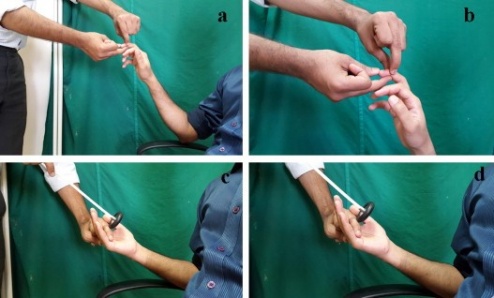
9.2. Muscle testing [21]
All the muscles of the arm can be evaluated with any of these tools: wrist extensors and flexors, elbow extensors and flexors, shoulder ab- and adductors, elevators and extensors, ... - Manual muscle testing - Hand-held dynamometer - Vigorometer - Pinchometer
9. 3. Reflexes
Reflexes are estimated by comparing both sides and there are 2-3 testing attempts [22]
- Hoffman's reflex (http://www.sciencedirect.com.ezproxy.vub.ac.be:2048/science/article/pii/S0303846715001316)
- Finger flexion (http://www.sciencedirect.com.ezproxy.vub.ac.be:2048/science/article/pii/S0303846715001316)
- Plantar reflex
- The Wazir hand myelopathy sign: a reflex of the palmaris longus tendon which is lightly tapped while the patient is holding his hand in supination. [23]
A combination of all the tests would give the best result and has a higher sensitivity and specificity. Like Tejus et al. discussed, the combination of the Hoffman's reflex, finger flexion reflex and plantar reflex, would be a good combination to investigate cervical myelopathy or spinal cord compression.
9.4. Sensation disorders
- You can ask the patient if they have any 'weird' feelings like numbness, tingling and you let them note that on their own anatomical figure [20]
9.5. Questionnaire
- JOACMEC: Japanese orthopedic association cervical myelopathy evaluation questionnaire: This questionnaire consists of 24 items. 13 items question the physical function and 11 items question the heath related quality of life.[24]
- Kobayashi et al. uses 20 items of the JOACMEC in his questionnaire, which is also a successful self-administered questionnaire.[25]
9.6. Gait Analysis
You can use gait analysis as an objective tool, in combination with other parameters, in the evaluation of functionality.[26]
9.7. Combination of tests by Cook et al.
Combinations of three of five or four of five of these tests enable post-test probability of the condition to 94–99%: • gait deviation • +ve Hoffmann’s test • inverted supinator sign • +ve Babinski test • age 45 years or older
9.8.Other clinical examination tests often used for myelopathy include:[24][5][9]
• Spurling’s test • Distraction test • +ve clonus/Babinski/Hoffman's • Hyperreflexic biceps • Hyperreflexic quadriceps • Hyperreflexic achilles • Pain constancy • L’hermitte’s sign • Romberg test
Although these tests exhibit moderate to substantial reliability among skilled clinicians, they demonstrate low sensitivity and are not appropriate for ruling out myelopathy. One method used to improve the diagnostic accuracy of clinical testing is combining tests into clusters. These often overcome the inherent weakness of standalone tests.[5][15]
10. Prevention
Till now, there is very less to find about prevention of cervical myelopathy. Further research should show off if there are strategies to prevent people from cervical myelopathy.
11. Medical management
There is no consensus about the treatment of mild and moderate forms of cervical myelopathy. Surgical treatment has no better results than conservative treatment over two years of follow-up. [27]. Patients with cervical myelopathy that are treated with a conservative approach (anti-inflammatory medication and physical therapy) may have some short term benefit in relief of painful symptoms. Because the condition is degenerative and progressive, slow and continued progressive neurologic deterioration will occur.
Motor training programmes may improve arm and hand functioning at function and/or activity level in cervical spinal cord injured patients[28].
People who have progressive neurologic changes (such as weakness, numbness or falling) with signs of severe spinal cord compression or spinal cord swelling are candidates for surgery. Patients with severe or disabling pain may also be helped with surgery.[29] When myelopathy is caused by factors of a progressive nature, such as spinal cord tumors, surgical treatment is likewise indicated. [30][31].
People who experience better surgical outcomes often have these characteristics:
• The symptom of an electrical sensation that runs down the back and into the limbs
• Younger age
• Shorter duration of symptoms
• Single rather than multiple areas of involvement
• Larger areas available for the cord
The principal aim of surgery for cervical myelopathy is decompression of the spinal cord. The surgical techniques include multilevel discectomies or corpectomies with or without instrumented fusion, laminectomy with or without instrumented fusion or laminoplasty. [4] Surgical decompression is generally considered if the symptoms affect daily life but early surgical intervention is thought to be more effective. Therefore, early detection may be the key to minimize postoperative sequelae. [16]
Final outcomes from the surgery vary. Typically, one-third of patients improve, one-third stay the same, and one-third continue to worsen over time, with respect to their pre-surgical symptoms. [10] [29]
12. Physical therapy management
Patients with mild or severe cervical myelopathy can be treated conservative. Kadaňka et al. found no difference in long term outcome (2 years after the intervention) between patient who received a conservative or surgical treatment.[32] (LOE:1b) Even after 10 years, there were no differences found between the surgery and conservative group.[33] (LOE: 1b) Also in the cochrane review no differences between surgical or conservative treatment were found[34] (LOE: 1a)
Shimomura et al. described that mild forms of cervical myelopathy can be treated non-surgically. The only prognostic factor in which surgery can be recommended is the circumferential spinal cord compression in the maximum compression segment on axial MRI[35] (LOE: 2b)
Rhee JM et al. describes myelopathy as a typically progressive disorder and that there is little of evidence that conservative treatment halts or reverses its progression. So, they recommend not routinely prescribing nonoperative treatment as the primary modality in patients with moderate to severe myelopathy.[36](LOE:2a)
In general, the goals of the treatment are: [4](LoE:5)
• relieve pain
• improve function
• prevent neurological deterioration
• reverse or improve neurological deficits
Cervical myelopathy can be treated symptomatically. Possible therapies include:
- Cervical traction and manipulation of the thoracic spine: useful for the reduction of pain scores and level of disability in patients with mild cervical myelopathy. Other signs and symptoms, such as weakness, headache, dizziness, and hypoesthesia, are positively affected. [37] Clinical Treatment Tool-kitClinical Treatment Tool-kit Cervical traction can be combined with other treatments like electrotherapy and exercises. Joghataei et al. reported a significant increase in grip strength after 10 weeks of this combined treatment. [38] (LOE: 2a)
- Manual therapy techniques: employed to reduce the neck pain with natural apophyseal glides and sustained natural apophyseal glides for cervical extension and rotation.[29] Deep Neck Flexor Stabilisation Protocol Manipulation and mobilizations can be effective when they are combined with exercise therapy. When you use them without exercises, there is only poor evidence that it could be effective.[39](LOE:1a) ([40]LOE: 1a)
- Exercises: The cochrane review did not assess the effects of exercise therapy on neck pain with radicular findings, but they found a lot of evidence for exercises for mechanical neck pain. For example: stretching, strengthening exercises, active range of motion exercises, home exercise programs, ...12 (LOE: 1a)
- Cervical stabilization exercises: when there is anteroposterior instability of the vertebral bodies of a degenerative nature, vertebral segment stabilization of the cervical spine can be performed with a pressure biofeedback unit (PBU), performing 10 repetitions sustained for 10s, beginning with 22mmHg with the intention to progress to 30mmHg. [29]
- Dynamic upper and lower limb exercises (flexion and extension) with the use of the PBU on the neck.[29](LoE:4)
- Proprioceptive neuromuscular facilitation: for the upper and lower limbs.[29]
- Improve posture
- Motor training programmes: may improve arm and hand functioning at function and/or activity level in cervical spinal cord injured patients
- Mobility and proprioception exercises
- Aerobic exercises such as the treadmill [29]
- Balance training e.g. standing on one leg with eyes open and evolving to eyes closed; standing on a stable platform and evolving to an unstable platform with a rocker board [29]
- Core stability exercices [29] Hydrotherapy [29]
| [41] | [42] |
In surgical cases, the physiotherapist still has an important role, both before and after the surgery. In the pre-operative phase, the physiotherapist needs to become thoroughly familiar with the patient's history and about his/her activities of daily living that they are aiming to return to. The physiotherapist will inform the patient about the treatment program and the expectations after the surgery. There are different tests to develop a thorough picture of the patient's baseline pre-operative status such as walking tolerance, Neck Pain and Disability Scale, Neck Disability Index and lung function. Nomura et. al found that the maximum voluntary ventilation should significantly increase after the surgery.[43]
Exercises to improve mobility and proprioception will be given to the patient. The patient starts unencumbered stabilisation exercises and then progresses to more active mobilisation exercises. During the day the patient is encouraged to perform ADLs. On the second day, the intensity of the exercises is increased and are then progressed to include standing and walking exercises. Assuming typical progress with rehabilitation, the patient can go home after the ninth day. At home, physiotherapy continues with active exercises. The physiotherapist has to make sure that the patient can continue his/her ADLs and increases the intensity of it daily. After a straightforward rehabilitation, there are no limitations to the ADLs for the patient. Also important in the rehabilitation is to improve the posture[44]. The main goal is to make the patient able to participate in society again without permanent restrictions due to the surgery.This is in line with the findings of Ogawa et al. who found that dynamic stress after the surgery may improve the functional recovery.[45]
13. Key research
Fouyas, Ioannis P., Patrick FX Statham, and Peter AG Sandercock. "Cochrane review on the role of surgery in cervical spondylotic radiculomyelopathy." Spine 27.7 (2002): 736-747. (LOE: 1a)
Binder, Allan I. "Cervical spondylosis and neck pain." BMJ: British Medical Journal 334.7592 (2007): 527-531. (LOE: 1a)
Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Brontfort G, et al, Cervical Overview Group. Exercises for mechanical neck disorders. Cochrane Database Syst Rev 2005 (LOE: 1a)
14. Resources
Dr. Pablo Pazmino, MD on Cervical Myelopathy
Mayo Clinic information on Spinal Stenosis
Wikipedia on Spinal Stenosis
In this video, Dr. Jeffrey Wang, a professor in the Department of Orthopaedic Surgery of UCLA, reviews Spinal Stenosis
| [46] | [47] |
Case Studies[edit | edit source]
57 Year-old male diagnosed with Cervical Myelopathy
Cervical Spondylotic Myelopathy in a Patient Presenting With Low Back Pain
15. Clinical Bottom Line
Cervical myelopathy is the result of spinal cord compression in the cervical spine and is the most common disorder of the spinal cord in persons older than 55 years of age. Cervical compression in myelopathy is predominantly due to pressure on the anterior spinal cord with ischaemia and to deformation of the cord by anterior herniated discs, spondylitic spurs or an ossified posterior longitudinal ligament. Early symptoms of this condition are ‘numb, clumsy, painful hands’ and disturbance of fine motor skill. The diagnosis of CSM is primarily based on the clinical signs found on physical examination and is supported by imaging findings of cervical spondylosis with cord compression. Once the disorder is diagnosed, complete remission to normality never occurs, and spontaneous remission to normal normality is uncommon. Exercises and techniques that may help relieve symptoms of cervical myelopathy include: cervical traction, manual therapy techniques, proprioceptive neuromuscular facilitation, cervical stabilization exercises and dynamic upper and lower limb exercises.
Presentations[edit | edit source]
 |
Cervical Arthritis, Cervical Spondylotic Myelopathy
This presentation was created by Pablo Pazmino MD. Cervical Arthritis, Cervical Spondylotic Myelopathy/ View the presentation |
16. Recent Related Research (from Pubmed)
1. Kadaňka, Zdeněk, et al. "Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years." European Spine Journal 20.9 (2011): 1533-1538. (LOE:2b)
Kadaňka et al. carried out a 10 year during study, which compared a group of patients with cervical myelopathy who received surgical treatment, or who received a conservative treatment. The patients who took part of this study were all suffering from mild or moderate non-progressive cervical myelopathy. They evaluated the patients with the modified JOA score, timed 10m walk test, score of daily activities and subjective assessment by the patients themselves. By using these tests the authors really focused on the daily activities and important stuff for the patients themselves. For example, the score of daily activities was given by an observation of the patient in a video. This video recorded the patient when they buttoned their shirt, brushed their hair and their teeth, walked, ran, ... After 36 months and after 10 years, there were no major differences between the surgical group and the conservative group. It is a fact that some people get better and some people get worse, in both groups. The authors also mention the importance of prognostic factors to decide whether you choose for surgery or not. These prognostic factors were described in another study: Predictive factors for mild forms of spondylotic cervical myelopathy treated conservatively or surgically (Patients should rather be treated conservatively if they a spinal transverse area larger than 70 mm2, are of older age, and have normal CMCT. Surgery is more suitable for patients with clinically worse status and a lesser transverse area of spinal cord.)
2. Rhee, John M., et al. "Nonoperative management of cervical myelopathy: a systematic review." Spine 38.22S (2013): S55-S67. (LOE:1a)
This review concludes that there is a lack of evidence about the comparison between surgical and conservative treatment for patients with cervical myelopathy. The evidence that we have had a low quality or was suspected on confounding. There also need to become research on non-surgical treatment independently.
17. References
- ↑ Richard K. Root Clinical Infectious Diseases: A Practical Approach, 1999
- ↑ 2.0 2.1 Kong LD, Meng LC, Wang LF, Shen Y, Wang P and Shang ZK. Evaluation of conservative treatment and timing of surgical intervention for mild forms of cervical spondylotic myelopathy. Exp Ther Med. 2013 Sep;6(3):852-856.
- ↑ Dai L, Ni B, Yuan W and Jia L. Radiculopathy after laminectomy for cervical compression myelopathy. J Bone Joint Surg Br. 1998 Sep;80(5):846-9.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 Boos N and Aebi M (Eds). Spinal disorders: Fundamentals of Diagnosis and Treatment. Springer-Verlag Berlin Heidelberg. 2008.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 5.8 5.9 Cook C, Brown C, Isaacs R, Roman M, David S and Richardson W. Clustered clinical findings for diagnosis of cervical spine myelopathy. J Man Manip Ther. 2010 Dec; 18(4): 175–180.
- ↑ Cramer GD and Darby SA. Basic and Clinical Anatomy of the Spine, Spinal Cord, and ANS. 2nd Edition. Elsevier 2008.
- ↑ 7.0 7.1 Selzer ME and Dobkin BH. Spinal Cord Injury (American Academy of Neurology Quality of Life Series). Demos Medical Publishing (New York). 2008
- ↑ 8.0 8.1 Cook C, Roman M, Stewart KM, Leithe LG, Isaacs R. Reliability and diagnostic accuracy of clinical special tests for myelopathy in patients seen for cervical dysfunction. J Orthop Sports Phys Ther. 2009 Mar;39(3):172-8. doi: 10.2519/jospt.2009.2938.
- ↑ 9.0 9.1 9.2 9.3 Amenta PS, Ghobrial GM, Krespan K, Nguyen P, Ali M, Harrop JS. Cervical spondylotic myelopathy in the young adult: a review of the literature and clinical diagnostic criteria in an uncommon demographic. Clin Neurol Neurosurg. 2014. 120:68-72.
- ↑ 10.0 10.1 Kadanka Z, Bednarík J, Vohánka S, Vlach O, Stejskal L, Chaloupka R et al. Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study. Eur Spine J. 2000;9(6):538-44.
- ↑ 11.0 11.1 Koakutsu T,Nakajo J, Morozumi N, Hoshikawa T, Ogawa S, and Ishii Y. Cervical myelopathy due to degenerative spondylolisthesis. Ups J Med Sci. 2011; 116(2): 129–132.
- ↑ 12.0 12.1 Yonenobu K. Cervical radiculopathy and myelopathy: when and what can surgery contribute to treatment? Eur Spine J. 2000; 9(1): 1-7.
- ↑ 13.0 13.1 Harrop JS, Naroji S, Maltenfort M, Anderson DG, Albert T, Ratliff JK et al. Cervical myelopathy: a clinical and radiographic evaluation and correlation to cervical spondylotic myelopathy. Spine (Phila Pa 1976). 2010 Mar 15;35(6):620-624.
- ↑ Park SJ, Kim SB, Kim MK, Lee SH and Oh IH. Clinical features and surgical results of cervical myelopathy caused by soft disc herniation. Korean J Spine. 2013;10(3):138-143.
- ↑ 15.0 15.1 15.2 Chad Cook, Christopher Brown, Robert Isaacs, Matthew Roman, Samuel Davis, and William Richardson. Clustered clinical findings for diagnosis of cervical spine myelopathy. J Man Manip Ther. 2010 December; 18(4): 175–180.
- ↑ 16.0 16.1 Sato T, Horikoshi T, Watanabe A, Uchida M, Ishigame K, Araki T et al. Evaluation of cervical myelopathy using apparent diffusion coefficient measured by diffusion-weighted imaging. AJNR Am J Neuroradiol. 2012; 33(2):388-392.
- ↑ Harrop, James S; Naroji, Swetha; Maltenfort, Mitchell; Anderson, D. Greg; Albert, Todd; Ratliff, John K; Ponnappan, Ravi K; Rihn, Jeffery A; Smith, Harvey E; Hilibrand, Alan; Sharan, Ashwini D; Vaccaro, Alexander. Cervical Myelopathy: A Clinical and Radiographic Evaluation and Correlation to Cervical Spondylotic Myelopathy. Spine 10 February 2010 [epub ahead of print]
- ↑ 18.0 18.1 18.2 Vitzthum H and Dalitz K. Analysis of five specific scores for cervical spondylogenic myelopathy. Eur Spine J. 2007; 16(12): 2096–2103.
- ↑ Tanaka N, Konno S, Takeshita K, Fukui M, Takahashi K, Chiba K et al. An outcome measure for patients with cervical myelopathy: the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): an average score of healthy volunteers. J Orthop Sci. 2014 Jan;19(1):33-48.
- ↑ 20.0 20.1 Barrett, Eva, Karen McCreesh, and Jeremy Lewis. "Reliability and validity of non-radiographic methods of thoracic kyphosis measurement: a systematic review." Manual therapy 19.1 (2014): 10-17.
- ↑ Persson, L. C. G., et al. "Cervical radiculopathy: Pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar A prospective, controlled study." European Spine Journal 6.4 (1997): 256-266.
- ↑ Tejus, M. N., et al. "An evaluation of the finger flexion, Hoffman's and plantar reflexes as markers of cervical spinal cord compression–A comparative clinical study." Clinical neurology and neurosurgery 134 (2015): 12-16.
- ↑ Ross, Michael D. "Cervical myelopathy: diagnosing another great impostor." Perspectives (2014): 31.
- ↑ 24.0 24.1 Fukui, Mitsuru, et al. "An outcome measure for patients with cervical myelopathy: Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): part 1." Journal of Orthopaedic Science 12.3 (2007): 227.
- ↑ Kobayashi, Hiroshi, et al. "Development of a self-administered questionnaire to screen patients for cervical myelopathy." BMC musculoskeletal disorders 11.1 (2010): 268.
- ↑ Siasios, Ioannis D., et al. "The Role of Gait Analysis in the Evaluation of Patients with Cervical Myelopathy: A Literature Review Study." World Neurosurgery 101 (2017): 275-282.
- ↑ Kadanka Z, Bednarík J, Vohánka S, Vlach O, Stejskal L, Chaloupka R, Filipovicová D, Surelová D, Adamová B, Novotný O, Nemec M, Smrcka V, Urbánek I. Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study. Eur Spine J (2000) 9 :538–544
- ↑ Annemie I. F. Spooren, Yvonne J. M. Janssen-Potten, Eric Kerckhofs and Henk A. M. Seelen. Outcome of motor training programmes on arm and hand functioning in patients with cervical spinal cord injury according to different levels of the icf: a systematic review. J Rehabil Med 2009; 41: 497–505
- ↑ 29.0 29.1 29.2 29.3 29.4 29.5 29.6 29.7 29.8 29.9 Almeida GP, Carneiro KK and Marques AP. Manual therapy and therapeutic exercise in patient with symptomatic cervical spondylotic myelopathy: a case report. J Bodyw Mov Ther. 2013 Oct;17(4):504-9.
- ↑ Massimo Leonardi, Norbert Boos , Degenerative disorders of the cervical spine
- ↑ 7 Law MD Jr, Bernhardt M, White AA 3rd.Cervical spondylotic myelopathy: a review of surgical indications and decision making. Yale J Biol Med. 1993 May-Jun;66(3):165-77.
- ↑ Kadaňka, Z., et al. "Conservative treatment versus surgery in spondylotic cervical myelopathy: a prospective randomised study." European Spine Journal 9.6 (2000): 538-544.
- ↑ Kadaňka, Zdeněk, et al. "Cervical spondylotic myelopathy: conservative versus surgical treatment after 10 years." European Spine Journal 20.9 (2011): 1533-1538.
- ↑ Fouyas, Ioannis P., Patrick FX Statham, and Peter AG Sandercock. "Cochrane review on the role of surgery in cervical spondylotic radiculomyelopathy." Spine 27.7 (2002): 736-747.
- ↑ Shimomura, Takatoshi, et al. "Prognostic factors for deterioration of patients with cervical spondylotic myelopathy after nonsurgical treatment." Spine 32.22 (2007): 2474-2479.
- ↑ Rhee, John M., et al. "Nonoperative management of cervical myelopathy: a systematic review." Spine 38.22S (2013): S55-S67.
- ↑ Browder DA, Erhard RE and Piva SR. Intermittent cervical traction and thoracic manipulation for management of mild cervical compressive myelopathy attributed to cervical herniated disc: a case series. J Orthop Sports Phys Ther. 2004;34(11):701-712.
- ↑ Joghataei, Mohammad Taghi, Amir Massoud Arab, and Hossein Khaksar. "The effect of cervical traction combined with conventional therapy on grip strength on patients with cervical radiculopathy." Clinical rehabilitation 18.8 (2004): 879-887.
- ↑ Binder, Allan I. "Cervical spondylosis and neck pain." BMJ: British Medical Journal 334.7592 (2007): 527-531.
- ↑ Kay TM, Gross A, Goldsmith C, Santaguida PL, Hoving J, Brontfort G, et al, Cervical Overview Group. Exercises for mechanical neck disorders. Cochrane Database Syst Rev 2005
- ↑ Rach Rauw. Cervical Traction Techniques. Available from: http://www.youtube.com/watch?v=ouoQd6PPJcI[last accessed 19/02/16]
- ↑ ReligiosoPT. Supine Thoracic Thrust. Available from: http://www.youtube.com/watch?v=Rj4Y5JGNPZs[last accessed 19/02/16]|}
- ↑ Nomura, Takuo, et al. "A subclinical impairment of ventilatory function in cervical spondylotic myelopathy." Archives of physical medicine and rehabilitation 85.7 (2004): 1210-1211.
- ↑ G. Aufdemkampe, J.B. Den Dekker, I. Van Ham, B.C.M. Smits-Engelsman, P. Vaes. Jaarboek fysiotherapie-kinesitherapie 2000. Bohn Stafleu Van Loghum, 275 p
- ↑ Ogawa, Yuto, et al. "Postoperative factors affecting neurological recovery after surgery for cervical spondylotic myelopathy." Journal of Neurosurgery: Spine 5.6 (2006): 483-487.
- ↑ Stanford University. Imaging Patients with Myelopathy. Available from: http://www.youtube.com/watch?v=mJVEtq5GsJk[last accessed 09/03/13]
- ↑ The Gait Guys. A Gait Case of Combined Spinal Myelopathy and Trendelenburg Pathologies. Available from: http://www.youtube.com/watch?v=AYmzQL_NSeI[last accessed 09/03/13]|}
(1) Barrett, Eva, Karen McCreesh, and Jeremy Lewis. "Reliability and validity of non-radiographic methods of thoracic kyphosis measurement: a systematic review." Manual therapy 19.1 (2014): 10-17. (LOE:1a)
(2) Persson, L. C. G., et al. "Cervical radiculopathy: Pain, muscle weakness and sensory loss in patients with cervical radiculopathy treated with surgery, physiotherapy or cervical collar A prospective, controlled study." European Spine Journal 6.4 (1997): 256-266.(LOE:2b)
(3) Tejus, M. N., et al. "An evaluation of the finger flexion, Hoffman's and plantar reflexes as markers of cervical spinal cord compression–A comparative clinical study." Clinical neurology and neurosurgery 134 (2015): 12-16. (LOE: 3b)
(4) Ross, Michael D. "Cervical myelopathy: diagnosing another great impostor." Perspectives (2014): 31. (LOE: 3a)
(5) Fukui, Mitsuru, et al. "An outcome measure for patients with cervical myelopathy: Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): part 1." Journal of Orthopaedic Science 12.3 (2007): 227. (LOE: 3b)
(6) Kobayashi, Hiroshi, et al. "Development of a self-administered questionnaire to screen patients for cervical myelopathy." BMC musculoskeletal disorders 11.1 (2010): 268. (LOE:3b)
(7) Siasios, Ioannis D., et al. "The Role of Gait Analysis in the Evaluation of Patients with Cervical Myelopathy: A Literature Review Study." World Neurosurgery 101 (2017): 275-282. (LOE: 1a)