Cauda Equina Syndrome
Original Editor - Laurie Fiegle and Tabitha Korona
Top Contributors - Laura Finucane, Tabitha Korona, Scott Buxton, Admin, Laura Ritchie, Thibaut Seys, Laurie Fiegle, Jolien Wauters, Evan Thomas, Kim Jackson, Margo De Mesmaeker, Rachael Lowe, Claire Knott, Lucinda hampton, Naomi O'Reilly, WikiSysop, Simisola Ajeyalemi, Shaimaa Eldib, Jess Bell, Olajumoke Ogunleye, Saud Alghamdi, Garima Gedamkar, Kai A. Sigel, 127.0.0.1, Karen Wilson, Tony Lowe and Candace GohDefinition[edit | edit source]
Cauda equina syndrome is a serious neurological condition affecting the bundle of nerve roots at the lower end of the spinal cord. It is due to a nerve compression that an acute loss of function of the lumbar plexus occurs which stops the sensation and movement.[1] The syndrome is characterized by dull pain in the lower back and upper buttocks and a lack of feeling in the buttocks, genitalia and thigh, together with the disturbance of bowel and bladder function.[2]
Clinically Relevant Anatomy
[edit | edit source]
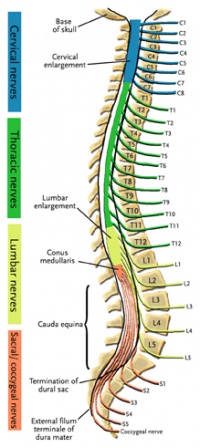
The central nervous system (CNS) includes the brain and spinal cord. The spinal cord allows transmission of signals to and from the brain to allow for movement, sensation, and visceral function. Nerves exiting the spinal cord are divided into sections based on their location of exit, for example, cervical nerves exit the cervical spine and thoracic nerves exit the thoracic spine. The conus medullaris is the distal end of the spinal cord and is usually located at the L1-L2 vertebral level.[3] Nerve roots continue to down the vertebral column after the conus medullaris and are referred to as the cauda equina. The cauda equina includes nerves from lumbar, sacral, and coxxcygeal origins. Being a bundle of nerves, the cauda equina is named for it's resemblance to a horse's tail.
Mechanism of Injury / Pathological Process[edit | edit source]
Cauda equina syndrome can be caused by a number of etiologies but the most common relate to compression of the cauda equina such as a herniated lumbosacral disc, spinal stenosis, and spinal neoplasm. Non-compressive causes include ishemia, infection, and inflammatory conditions. [4]
Ruptured disc, tumor, or fracture can also lead to Cauda equina syndrome. [5]
Clinical Presentation[edit | edit source]
Since the cauda equina nerve roots supply most of the lower extremity (including the pelvic region) sensory and motor innervations, cauda equina syndrome results in multiple motor and sensory signs. [4]
The most common signs and symptoms include bilateral sciatica, saddle region anesthesia, loss of bowel and bladder control, bilateral foot weakness, quadriceps weakness, severe back pain.[6] Other signs and symptoms include decreased sensation between the legs, buttocks, or feet. [5]
Diagnostic Procedures[edit | edit source]
If cauda equina syndrome is expected, medical referral is a necessity to decrease the possibility of permanent damage. Diagnostic procedures used to confirm cauda equina syndrome may include an MRI or myelogram. [7]
Management / Interventions
[edit | edit source]
Cauda equina syndrome is a medical emergency and requires immediate medical referral.
Treatment of cauda equina syndrome is going to vary based on the cause of the symptoms. Surgical decompression may be used if necessary.
The treatment for the cauda equine syndrome consist of surgery for the clearance of the compressed nerve roots. This only takes away the cause but most of the people still have complaints afterwards[8]:
- Bladder and bowel dysfunction
- Muscle weakness or paralysis in lower extremities
- Walking disorders
| [9] |
Treatment goals are[10][11]:
- Maintain mobility and strength in upper limbs
- Improve flexibility in lower back
- Improve core strength
- Improve range of motion and strength in lower limbs
- Improve standing and walking function
- Improve bladder and bowel function
- Improve endurance
Treatment resources[12]:
- Active exercise for upper limbs
- Exercises for ROM in lower limbs
- Functional electrical stimulation
- Electrical stimulation assisted isometric exercise (to prevent limb muscle atrophy)
- Training for daily mobility tasks (transferring, bed mobility and sitting)
- Strengthening lower limbs
- Devices for bracing lower limbs
Initial training speed must be chosen in function of the patient, it must be comfortable. Training intensity varies from 10 – 45 minutes pro session at a frequence of 5 days/week[13].
Most recovery takes place in the first year after the operation. In the second year there can also be recovery, and even in the third year. After that, the chance of further recovery is very small.[14]
Differential Diagnosis
[edit | edit source]
- Conus medullaris syndrome
- Herniated Nucleus Pulposis
- Lumbar Radiculopathy
- Lumbar vertebrae fracture
- Mechanical back pain
- Peripheral neuropathy
- Spinal cord compression
- Spinal tumor
Key Evidence[edit | edit source]
Cauda equina syndrome is a rare but serious disorder. Prevalence in patients with low back pain is about 4 in 10,000. [15]
Resources
[edit | edit source]
For more information regarding the emergency medical treatment of cauda equina syndrome please see the article entitled "Orthopedic pitfalls:cauda equina syndrome." [15]
Case Studies[edit | edit source]
add links to case studies here (case studies should be added on new pages using the case study template)
Recent Related Research (from Pubmed)[edit | edit source]
Failed to load RSS feed from http://eutils.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1jMIPaXSb2LibMy2sXrSt6VzapdO5xrp57LTyoVmfEZisjpQz|charset=UTF-8|short|max=10: Error parsing XML for RSS
References[edit | edit source]
References will automatically be added here, see adding references tutorial.
- ↑ Jun W. et al. Cauda equina syndrome caused by a migrated bullet in dural sac. Turk Neurosurg 2010 Oct;20(4):566-9. [1C]
- ↑ Shi J. et al. Clinical classification of cauda equina syndrome for proper treatment. Acta orthop 2010 Jun;81(3):391-5. [1B]
- ↑ Dutton, M. (2008). Orthopaedic: Examination, evaluation, and intervention (2nd ed.). New York: The McGraw-Hill Companies, Inc.
- ↑ 4.0 4.1 Orendacova J, Cizkova D, Kafka J, Lukacova N, Marsala M, Sulla I, Marsala J, Katsube N. Cauda Equina Syndrome. Progress in Neurobiology 2001;64:613-37.
- ↑ 5.0 5.1 American Academy of Orthopaedic Surgeons, Your Orthopaedic Connection. Cauda Equina Syndrome. http://orthoinfo.aaos.org/topic.cfm?topic=A00362 (accessed 28 May 2009)
- ↑ Shapiro S. Medical Realities of Cauda Equina Syndrome Secondary to Lumbar Disc Herniation. SPINE 2000;25:3, 348-52
- ↑ Ogilvie J. Complications in Spondylolisthesis Surgery. SPINE 2005;30:65 S97-S101
- ↑ Fraser S. et al. Cauda equina syndrome: a literature review of its definition and clinical presentation. Arch Phys Med Rehabil. 2009 Nov;90(11):1964-8. [1A]
- ↑ Bob Spine. Microsurgery for disc herniation with Cauda Equina Syndrome by Robert Hacker. Available from: http://www.youtube.com/watch?v=kbcXBk3sqrU [last accessed 22/02/13]
- ↑ http://www.ehow.com/way_5507093_exercise-therapy-cauda-equina-syndrome.html
- ↑ E. Bizzarini et al. Epidemiology and clinical management of Conus-Cauda Syndrome and flaccid paraplegia in Friuli Venezia Giulia: Data of the Spinal Unit of Udine. Basic Applied Myology 2009;19(4):163-167. [1B]
- ↑ E. Bizzarini et al. Epidemiology and clinical management of Conus-Cauda Syndrome and flaccid paraplegia in Friuli Venezia Giulia: Data of the Spinal Unit of Udine. Basic Applied Myology 2009;19(4):163-167. [1B]
- ↑ E. Bizzarini et al. Epidemiology and clinical management of Conus-Cauda Syndrome and flaccid paraplegia in Friuli Venezia Giulia: Data of the Spinal Unit of Udine. Basic Applied Myology 2009;19(4):163-167. [1B]
- ↑ http://www.cauda.nl/index-eng.htm
- ↑ 15.0 15.1 Small S, Perron A, Brady W. Orthopedic pitfalls: cauda equina syndrome. The American Journal of Emergency Medicine 2005;23:159-63