Cauda Equina Syndrome: Difference between revisions
No edit summary |
No edit summary |
||
| Line 158: | Line 158: | ||
==== Physical examination ==== | ==== Physical examination ==== | ||
The physical examination should include a full neurological assessment to | The physical examination should include a full neurological assessment to determine dermatomal sensory loss, myotomal weakness and reflex change. Where a patient reports bilateral leg pain, signs of upper motor neuron involvement should be examined (babinski and clonus). For a comprehensive overview of neurological integrity testing the reader is referred to the following book 'Neuromusculoskeletal examination and assessment' <ref>Petty N, editor. Neuromusculoskeletal examination and assessment a handbook for therapists. Fourth edition. Churchill Livingstone. 2011.</ref>. | ||
Where a patient reports sensory changes in the perineal area this should be tested to evaluate any sensory loss. | Where a patient reports sensory changes in the perineal area this should be tested to evaluate any sensory loss. | ||
| Line 164: | Line 164: | ||
A digital rectal examination should be perfomed to assess any loss of anal sphincter tone. This should only be performed by an appropriately trained clinician. | A digital rectal examination should be perfomed to assess any loss of anal sphincter tone. This should only be performed by an appropriately trained clinician. | ||
<br> | |||
<br> | |||
*<br> | |||
* | |||
== Diagnostic Procedures == | == Diagnostic Procedures == | ||
Revision as of 21:28, 20 August 2017
Original Editor - Laurie Fiegle and Tabitha Korona
Top Contributors - Laura Finucane, Tabitha Korona, Scott Buxton, Admin, Laura Ritchie, Thibaut Seys, Laurie Fiegle, Jolien Wauters, Kim Jackson, Evan Thomas, Margo De Mesmaeker, Rachael Lowe, Claire Knott, Lucinda hampton, Naomi O'Reilly, WikiSysop, Simisola Ajeyalemi, Tony Lowe, Candace Goh, Shaimaa Eldib, Jess Bell, Olajumoke Ogunleye, Saud Alghamdi, Garima Gedamkar, Kai A. Sigel, 127.0.0.1 and Karen Wilson
Definition[edit | edit source]
Cauda equina syndrome (CES) is a rare but serious neurological condition affecting the bundle of nerve roots at the lower end of the spinal cord. The CE provides innervation to the lower limbs, and sphincter,controls the function of the bladder and distal bowel and sensation to the skin around the bottom and back passage[1].
CES occurs when the nerves below the spinal cord are compressed causing compromise to the bladder and bowel. The most common cause of CES is a prolapse of a lumbar disc but other conditions such as metastatic spinal cord compression can also cause CES[1].
There is no agreed definition of CES but the British Association of Spinal Surgeons (BASS) present a definition that is useful in clinical practice;
'A patient presenting with acute back pain and/or leg pain...... with a suggestion of a disturbance of their bladder or bowel function and/or saddle sensory disturbance should be suspected of having a CES. Most of these patients will not have critical compression of the cauda equina. However, in the absence of reliably predictive symptoms and signs, there should be a low threshold for investigation with an emergency scan'[2].
Classification[edit | edit source]
4 groups of patients have been classified according to their presentation :[3]
CESS- Suspected
Patients who do not have CES symptoms but who may go on to develop CES. It is important that patients understand the gravity of the condition and the importance of the time frame to seeking urgent medical attention. The use of a *credit card style patient information leaflet or a leaflet explaining what to look for and what to do should they develop symptoms is recommended.
CESI- Incomplete
Patients who present with urinary difficulties with a neurogenic origin, including loss of desire to void, poor stream, needing to strain to empty their bladder, and loss of urinary sensation. These patients could develop CESR and are a medical emergency and should be decompressed urgently.
CESR -Retention
Patients who present with painless urinary retention and overflow incontinence; the bladder is no longer under executive control.
Surgical intervention is necessary and should be carried out as soon as practically possible.
CESC-Complete
Patients who have objective loss of the cauda equina function, absent perineal sensation, a loose anus and paralysed bladder and bowel.
Clinically Relevant Anatomy[edit | edit source]
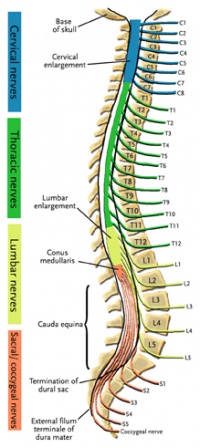
The spinal cord ends around L1, consequently, the caudal nerve roots below the first lumbar root, form the cauda equina. The roots descend at an almost vertical angle to reach their corresponding foramina, gathered around the filum terminale within the spinal theca[5]. The proximal portion of the cauda equina is said to be hypovascular hence more vulnerable if compressed [6]. The cauda equina roots have both a dorsal and ventral root. The ventral root provides motor fibres for the efferent pathway along with sympathetic fibres. The dorsal root is composed of afferent fibres for the transmission of sensation. The functions of those nerves are:
Sensory and motor fibres to the lower limbs.
Sensory innervation to the saddle area
Voluntary control of the external anal and urinary sphincters
Aspects of anatomical features relating to saddle sensation, bladder, bowel and sexual function are discussed below;
The first three sacral nerves, S1,2 and 3 supply multifidus and lateral cutaneous branches to the skin and fascia over the sacrum and part of the gluteal region. The 4th and 5th sacral nerves, S4 and 5, along with posterior primary ramus of the coccygeal nerve supply the skin and fascia around the coccyx. The pelvic splenic nerves to the pelvic viscera composed of parasympathetic fibres, travel in the ventral rami of S2,3 and 4. They then leave these nerves as they exit the anterior sacral foramina and pass to the pre-sacral tissue. Some pass to the pelvic viscera alongside the pelvic sympathetic supply and supply the urogenital organs and distal aspect of the large intestine. Others pass immediately into retroperitoneal tissue and into the mesentry of the sigmoid and descending colon [5]. The pudendal nerve supplies the perineum and arises from S2,3 and 4 with its terminal branches including the dorsal nerve of the penis or clitoris[7].
Epidemiology/Etiology[edit | edit source]
CES occurs as a consequence of compression of the cauda equina and can be caused by a number of pathologies. The prevalence among the general population has been estimated between 1:100 000 and 1:33 000. The most common cause of CES is herniation of a lumbar intervertebral disc[8] and accounts for 2% of all herniated lumbar discs.[9] It commonly affects the discs at the L4/5 and L5/S1 level . However disc prolapse at any lumbar level can cause CES. Patients may be predisposed to CES if they have a congenitally narrow spinal canal or have acquired spinal stenosis. [10]The prevalence among patients with low back pain is approximately four in 10 000[11].
CES affects males and females equally and can occur at any age but primarily in adulthood.
Other pathologies which can cause CES include spinal stenosis, haematoma, trauma [12] tumour, infection, fracture and inflammatory conditions. [1][13][14]
Other rare causes such as abdominal aortic dissection, and complications after surgery, anesthetic procedures, spinal manipulation or epidural injections are possible causes of CES[1].
Clinical Presentation[edit | edit source]
5 characteristic features of CES are consistently described in the literature and should form the basis of questions related to diagnosis[3];
· bilateral neurogenic sciatica
Pain associated with the back and/ or unilateral/bilateral leg symptoms maybe present.
· reduced perineal sensation
Sensation loss in the perineum and saddle region is the most commonly reported symptom.
· altered bladder function leading to painless retention
Bladder dysfunction is the most commonly reported symptom and can range from increased frequency , difficulty in micturation, incontinence and retention.
· loss of anal tone
loss or reduced anal tone may be evident if a patient reports bowel dysfuntion. Bowel dysfunction may include incontinence, inability to control motions, inability to feel when the bowel is full and consequently overflow.
· loss of sexual function
Sexual dysfunction is not widely mentioned in the literature but is an important aspect that should be discussed with patients.
Communication
A Qualitative research study has identified that clear communication plays a pivotal role in identifying Cauda Equina Syndrome patient’s early to facilitate bringing these patients to the surgical team in a timely manner [15]. Through this study it emerged that in order to identify CES patients early in the disease process to facilitate a timely surgical opinion one of the key problems was the use of language that reflected the patient’s own voice. The patient participants emphasised the need for clinicians to use language that they could understand during a clinical consultation, especially in the context of severe pain. A CES cue card for clinicians to use in the clinical consultation to enable the patient to focus on important questions was developed. It enables clinicians to frame the questions as important. The clinical cue card maps against a patient credit card using the same questions. This highlights symptoms to look out for and crucially timely action to take should symptoms develop. The credit card could be used by the patient particularly in an emergency setting to help express the change in embarrassing and sensitive symptoms.
*Follow this link to download the patient credit card
https://macpweb.org/home/index.php?p=396
Differential Diagnoses[edit | edit source]
- Conus medullaris syndrome
- Spinal tumor
- Abscesses[17]
- Central or centerolateral disk prolapsed[18]
- Space-occupying lesions that compress nerve roots have been described as causes of CES.
- Canal stenosis [13]
- Spinal Anesthesia
- Neoplasm [14]
- Ischemia
- Infections
- Inflammatory conditions
- Osteomyelitis
Examination[edit | edit source]
Subjective examination[edit | edit source]
The difficulty with diagnosing serious spinal conditions early and the catastrophic outcomes of delayed diagnosis are widely documented [19][20]. The subjective history is the most important aspect of the examination early in the disease process as the subtle and vague symptoms related to early Cauda Equina Syndrome need to be identified using clear methods of communication. Good communication skills allow us to gain an understanding of the patient’s world by achieving an understanding of what patients perceive is happening to them[21] [21]. The important items to screen within the subjective history are Red Flags. It is well recognized that the presence of Red and Yellow Flags are not mutually exclusive (Gifford, 2000). The clinical reasoning process essentially combines a biopsychosocial assessment alongside this Red Flag screening to get a full true picture of the patient’s story and current clinical presentation. Establishing the history of the present condition in detail is key as timing is of paramount importance in this condition.
- When the back and or leg pain started is significant but precisely when symptoms relating to parasympathetic supply began is vital; one hour, one day, one week, 15 years? There is no way of predicting who will progress from CESS to CESR and how quickly this may happen and so precise recording of the timing of chronology cannot be underestimated.
- Establish if things are changing, better, episodic, worse or the same. Improving pain does not necessarily mean the condition is improving. Checking Red Flags and neurological status is important before this improved status can be assumed. Constant pain and night pain must be viewed along with all Red Flags with caution.
- Establish the pattern of pain through 24 hours. Reference of pain and precise area of pins and needles and numbness must be identified and clearly documented. Aggravating and easing factors should be explored. . Establish if these symptoms have been experienced before or are they different?
- Has an MRI been performed with these current symptoms? This seems so obvious but can help with the clinical reasoning process.
- What treatments have been tried including medication is helpful on a variety of levels. Many medications cause symptoms that masquerade as CES[22]. This does not mean that symptoms can be ignored and attributed to drugs, however, medication could be contributing to the bladder, bowel and sexual dysfunction. Similarly, pain can cause retention.
- Explore the patient’s medication regime and escalation up the analgesic ladder? Is medication being used appropriately and titrated correctly? This can give an indication of the severity of pain and its control. Establish the quality and intensity of pain e.g VAS.
- What is the past medical history status; previous diagnosis of disc pathology or spinal stenosis for instance may be significant. Previous history of serious conditions such as cancer must be noted and may be important. Similarly many co-morbidities could masquerade as CES e.g. Diabetes, Multiple Sclerosis, Benign prostatic hyperplasia, pregnancy.
- Has there been any recent or past spinal surgery and any history of osteoporosis; a retropulsed vertebral insufficiency fracture could cause CES.
If CES/CES risk is suspected the subjective history must explore symptoms in even more detail. Tools and questions to use are covered in the next Research section. It is important that these questions are framed to highlight their gravity. The patient needs to recognise that the next questions are vital and accurate response of the utmost importance.
Physical examination[edit | edit source]
The physical examination should include a full neurological assessment to determine dermatomal sensory loss, myotomal weakness and reflex change. Where a patient reports bilateral leg pain, signs of upper motor neuron involvement should be examined (babinski and clonus). For a comprehensive overview of neurological integrity testing the reader is referred to the following book 'Neuromusculoskeletal examination and assessment' [23].
Where a patient reports sensory changes in the perineal area this should be tested to evaluate any sensory loss.
A digital rectal examination should be perfomed to assess any loss of anal sphincter tone. This should only be performed by an appropriately trained clinician.
Diagnostic Procedures[edit | edit source]
The diagnosis of cauda equina syndrome generally is possible based on medical history and physical examination findings. Radiologic and laboratory studies are used to confirm the diagnosis and for localizing the site of the pathology and the underlying cause.[16]
A physical exam is necessary to assess the strength, reflexes sensation, stability (=a posture / movement where an ideal distribution of body mass is reached. This provides the body with conditions for normal function during stationary positions or movements (sitting ⇒ stand, walk, walk, ...)) , alignment and motion. The physical exam is an essential part of any doctor's visit. Surprisingly, though, there are no absolutes (= assurances that signs are pointing in the direction of CES) in a routine physical examination. If there is a loss of function from the muscles, strength tests are used to confirm.
Electromyography (EMG) may show evidence of acute denervation and could also help in predicting prognosis and monitoring recovery. Performing an EMG of the bilateral external anal sphincter muscles is recommended.[24]
If cauda equina syndrome is expected, medical referral is a necessity to decrease the possibility of permanent damage. Diagnostic procedures used to confirm cauda equina syndrome may include an MRI or myelogram[25]. For diagnosis of cauda equine syndrome, one or more of the following must be present[18][26]
- Bladder and/or bowel dysfunction
- Reduced sensation in saddle area
- Sexual dysfunction
- Possible neurological deficit in the lower limb (motor/sensory loss, reflex change)
While MRI, coupled with patient history and examination, remains the diagnostic gold standard, it comes at a high cost with many patients demonstrating no concordant pathology.[27]
Medical Management[edit | edit source]
Any patient with urinary dysfunction must be studied on an emergent basis, particularly if the patient has suffered an acute change. The burden to the patient in the setting of missed or delayed diagnosis of cauda equina syndrome may be devastating because the patients can lose bowel, bladder, and sexual function, which can negatively affect patient health and quality of life. By operating <48 hours of cauda equina syndrome onset and communicating with the patient the potential outcome, a greater chance exists that one can reduce the considerable financial burden to institutions and have a less adverse outcome in court.[28] [2A]
Once CES is diagnosed, emergent surgical decompression is recommended to avoid potential permanent neurological damage[11].[1A]
Time from symptom onset to surgery is not correlated with persistence of major symptoms. [9] [2A]
The emergent surgical decompression must take place as soon as possible in order to reduce or eliminate pressure on the nerve. It is recommended to perform the decompression within 24-48 hours after the appearance of the first symptoms of compression so that there is a maximum potential for improvement of sensory and motor deficits as well as bladder and bowel functioning[29]. [1A]
The role of surgery is to relieve pressure from the nerves in the cauda equina region and to remove the offending elements[29]. [1A]
Surgical strategy is usually focused on the underlying causes. Generally, spine posterior decompression is often adequate - unless there is a lesion such as vertebrae destruction, neoplasm or large abscess in the anterior spine. Multiple surgical approaches of decompression are recommended such as discectomy, microdiscectomy, microscopic decompression, fenestrations, laminectomy, hemisemilaminotomy, distraction laminoplasty, multilevel laminectomies, neurolysis of CE, and intradural exploration of the nerve roots[11].[1A]
The surgical decompression takes away the cause of pain but most individuals still have complaints afterwards:
- Bladder and bowel dysfunction
- Muscle weakness or paralysis in lower extremities - Walking disorders[18] [1A]
Most recovery takes place in the first year after the operation; however, there can be recovery up to the third year post-operation. After this time period, recovery is very minimal[30]. [3A]
When there is a CES secondary to L5 giant cell tumour (GCT), these patiënts can be treated with denosumab and without surgery. The usage of denosumab allows potential neurological recovery without any surgical intervention. If surgery is not contraindicated, more time is obtained to prepare the patient preoperatively to attain safer surgery and to achieve complete tumour clearance.[31] [4]
Physical Therapy management[edit | edit source]
The ultimate goals of physical management are to ensure maximum neurological recovery and independence, a pain-free and flexible spine, maintenance of mobility and strength in lower limbs, of core strength, improvement of standing and walking function, improvement of bladder, bowel and sexual function, improvement of endurance and safe functioning of the various systems of the body with minimal or no inconvenience to patients and prevention or minimization of complications[18]. [1A] It is equally important for patients to regain assertiveness, take control of their own lives, and return to activities of their choice. The importance of on-going support to maintain health and independence following discharge should be strongly emphasized[29][30].[1A][3A]
Locomotion training as a therapeutic exercise was initially recognized in spinal cord injury patients, beginning with Body-weight Supported Treadmill Training (BWSTT) and Knee Ankle Foot Orthosis (KAFOs) personalized in soft-cast for the stabilization of the limbs. They have experienced Patterned Electrical Stimulation (PES) assisted isometric exercise to prevent limb muscle atrophy. It is known that PES-assisted isometric exercise reduces the degree of lower limb muscle atrophy in individuals with recent motor complete spinal cord injury, but not to the same extent as a comparable program of FES assisted exercise[32].[1B]
The principles of using electrical stimulation of peripheral nerves or nerve roots for restoring useful bladder, bowel, and sexual function after damage or disease of the central nervous system are described. Activation of somatic or parasympathetic efferent nerves can produce contraction of striated or smooth muscle in the bladder, rectum, and sphincters. Activation of afferent nerves can produce reflex activation of somatic muscle and reflex inhibition or activation of smooth muscle in these organs. In clinical practice these techniques have been used to produce effective emptying of the bladder and bowel in patients with spinal cord injury and to improve continence of urine and feces[33].[1A]
The use of manual therapy in conjunction with exercise is of potential benefit for patients suffering from low back pain. Utilization of manual therapy in a management program is associated with improvements in pain and disability. It is noteworthy to mention, however, that the manual therapy used in these studies was not of uniform technique nor applied only to one region. The techniques used in these studies were varied, and included both thrust and non-thrust manipulation/mobilization. Successful results were reported with techniques described as follows: flexion distraction manipulations, sidelying lumbar rotation thrust, posterior-to-anterior mobilizations, sidelying translatoric side bending manipulations, thoracic thrusts and neural mobilizations[34].[1A]
Individualized exercises often include components of unweighted walking or cycling, spinal mobility and lumbar flexion exercises, hip mobility exercises, hip strengthening, and core strengthening[34].[1A]
After surgery, there is also a need for recovery. Adjuvant radiotherapy and chemotherapy were performed in a case and showed 1-year after the operation no more problems. The craniospinal MRI was normal, and no recurrence was observed.[35] [5]
Site-specific radiotherapy was initiated with Bevacizumab in combination with vinorelbine. Upon completion of radiotherapy a radiographic response in both the brain and spine was confirmed. Also, the headaches, diplopia and incontinence significantly improved, and the patient was able to resume walking without assistance and became independent in her daily activities. [36] [5]
Key Evidence[edit | edit source]
Cauda equina syndrome is rare and is estimated to account for fewer than 1 in 2000 of patients with severe low back pain[18]
The annual incidence rate of cauda equina lesions has been estimated at 3.4 per million and the period prevalence at 8.9 per 100,000[8]
It is a disease of low incidence in the population, at around 1 case per 33000 to 1 case per 100000 inhabitants.[13]
It’s accounting for a reported incidence of 1-5% of spinal pathology in the literature[37].
Resources[edit | edit source]
• http://orthoinfo.aaos.org/topic.cfm?topic=A00362
• http://www.spine-health.com/conditions/lower-back-pain/cauda-equina-syndrome
• http://mayfieldclinic.com/PE-CaudaEquina.htm
• https://www.spineuniverse.com/conditions/back-pain/low-back-pain/cauda-equina-syndrome
• http://www.emedicinehealth.com/cauda_equina_syndrome/article_em.htm
• http://www.livestrong.com/article/228836-bowel-bladder-complications-from-a-lumbar-herniated-disc/
• http://www.aans.org/Patient%20Information/Conditions%20and%20Treatments/Cauda%20Equina%20Syndrome.aspx
• http://www.medicinenet.com/cauda_equina_syndrome/article.htm
• http://www.caudaequina.org/definition.html
• https://radiopaedia.org/articles/cauda-equina-syndrome
• http://www.emdocs.net/cauda-equina-syndrome/
• http://www.oapublishinglondon.com/article/1456#
• http://emedicine.medscape.com/article/1148690-clinical - b3
Clinical Bottom Line[edit | edit source]
Cauda equina syndrome is an uncommon but serious neurological condition affecting the bundle of nerve roots at the lower end of the spinal cord. It is due to a nerve compression that an acute loss of function of the lumbar plexus occurs which stops the sensation and movement. Cauda equina syndrome can be caused by a number of etiologies but the most common relate to compression of the cauda equina such as a herniated lumbosacral disc, spinal stenosis, hematoma, trauma, and spinal neoplasm. Ruptured disc, tumor, or fracture can also lead to cauda equina syndrome. Non-compressive causes include ischemia, infection, and inflammatory conditions. But there are a portion of cases that can’t be identified. The diagnosis of cauda equina syndrome generally is possible on the basis of medical history and physical examination findings. Diagnostic procedures used to confirm cauda equina syndrome may include an MRI or myelogram. Once CES is diagnosed, emergent surgical decompression is recommended to avoid potential permanent neurological damage. The emergent surgical decompression must take place as soon as possible in order to reduce or eliminate pressure on the nerve. They have experienced Patterned Electrical Stimulation (PES) assisted isometric exercise to prevent limb muscle atrophy. They use electrical stimulation of peripheral nerves or nerve roots for restoring useful bladder, bowel, and sexual function after damage or disease of the central nervous system. Utilization of manual therapy in a management program is associated with improvements in pain and disability. Individualized exercises often include components of unweighted walking or cycling, spinal mobility and lumbar flexion exercises, hip mobility exercises, hip strengthening, and core strengthening.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Fraser s, Roberts L, Murphy E. Cauda Equina Syndrome: A Literature Review of Its Definition and Clinical Presentation. Archives of Physical Medicine and Rehabilitation 2009 90(11), pp.1964–1968.
- ↑ Germon T, Ahuja,S, Casey A, Rai A. British Association of Spine Surgeons standards of care for cauda equina syndrome. The Spine Journal 2015 15 (3), pS2-S4.
- ↑ 3.0 3.1 Todd, N V; Dickson, R A . Standards of care in cauda equina syndrome. British Journal of Neurosurgery. 2016, 30 (5), p518-522.
- ↑ CES UK. Presentation - A Neurological Perspective of Cauda Equina Syndrome . Available from: http://www.youtube.com/watch?v=MLnY_esmmhE [last accessed 20/04/14]
- ↑ 5.0 5.1 Standring, S (ED IN CHIEF) Grays Anatomy, the anatomical basis of clinical practice 40th edition Churchill Livingstone Elsevier, 2008.
- ↑ Parke WW, Gammell K, Rothman RH. Arterial vascularization of the cauda equina. J Bone Joint Surg Am 1981; 63: 53–62.
- ↑ Brash J Jamieson E,(ed) Cunninghams Text book of Anatomy 7th edition. Oxford Medical Publications. 1937.
- ↑ 8.0 8.1 Boek: Dutton, M. (2008). Orthopaedic: Examination, evaluation, and intervention (2nd ed.). New York: The McGraw-Hill Companies, Inc.
- ↑ 9.0 9.1 Bydon, Mohamad, et al. "Time to Surgery and Outcomes in Cauda Equina Syndrome: An Analysis of 45 Cases." World neurosurgery 87 (2016):110-115.[Level Of Evidence: 2A]
- ↑ Dhokia R, Eames N. Cauda Equina Syndrome: A review of the current position. Hard Tissue 2014 Apr 18;3(1):7. [Level Of Evidence 3A]
- ↑ 11.0 11.1 11.2 MA Bin, WU Hong, JIA Lian-shun, YUAN Wen, SHI Guo-dong and SHI Jian-gang, Cauda equina syndrome: a review of clinical progress, Chinese Medical Journal, 2009 [1A]
- ↑ Song H. et al. Early surgery predicts a better prognosis of urinary function in cauda equine syndrome with retention: a systematic review and meta-analysis. Int J Clin Exp Med 2016;9(2):544-551. [Level Of Evidence: 1A]
- ↑ 13.0 13.1 13.2 Fuso FAF, Dias ALN, Letaif OB, Cristante AF, Marcon RM, Barros Filho TEP. Epidemiological study of cauda equina syndrome. Acta Ortop Bras. [online]. 2013;21(3):159- 62. [Level Of Evidence: 4]
- ↑ 14.0 14.1 14.2 Panos G. Et al. Differential diagnosis and treatment of acute cauda equina syndrome in the human immunodeficiency virus positive patient: a case report and review of the literature. Journal of medical case report 2016; 10:165. [Level Of Evidence: 3A]
- ↑ Greenhalgh S, Truman C, Webster V , Selfe J. 2016 Development of a toolkit for early identificationof cauda equina syndrome. Primary Health Care Research & Development. 2016;17:559-567.
- ↑ 16.0 16.1 Ahad A. Et al. The accurancy of clinical symptoms in detecting cauda equina syndrome in patients undergoing acute MRI of the spine. The neuroradiology journal. 2015; 28(4): 438-442. [Level Of Evidence: 2B]
- ↑ 17.0 17.1 Alex Gitelman, MD, Shuriz Hishmeh, MD, Brian N. Morelli, Cauda Equina Syndrome: A Comprehensive Review, The American Journal of Orthopedics®, 2008. [3A]
- ↑ 18.0 18.1 18.2 18.3 18.4 Stuart Fraser, Lisa Roberts, Eve Murphy, Cauda Equina Syndrome: A Literature Review of Its Definition and Clinical Presentation, Archives of Physical Medicine and Rehabilitation, Volume 90, Issue 11, Pages 1964-1968, November 2009 [1A]
- ↑ Levack P, Graham J, Collie, D, et al. 2002. Don’t wait for a sensory level-listen to the symptoms: a prospective audit of the delays in diagnosis of malignant cord compression. Clin. Oncol. 2002;14: 472–480.
- ↑ Markham D E.2004. Cauda equina syndrome: diagnosis, delay and litigation risk. Journal of Orthopaedic Medicine. 2004; 26: 102–105
- ↑ 21.0 21.1 Swain J. Interpersonal communication. In: French, Sally, Sim, Julius (Eds.), Physiotherapy a Psychosocial Approach, 3rd ed. Edinburgh, pp. 205–219. 2004.
- ↑ Woods E, Greenhalgh S, Selfe J (2015) Cauda Equina Syndrome and the challenge of diagnosis for physiotherapists: a review Physiotherapy Practice and Research. 2015;36:81-86
- ↑ Petty N, editor. Neuromusculoskeletal examination and assessment a handbook for therapists. Fourth edition. Churchill Livingstone. 2011.
- ↑ Podnar S. Utility of sphincter electromyography and sacral reflex studies in women with cauda equina lesions. Neurourology and urodynamics. 2014; 33:426-430 [Level Of Evidence 4]
- ↑ Ogilvie J. Complications in Spondylolisthesis Surgery. SPINE 2005;30:65 S97-S101
- ↑ Shi J. et al. Clinical classification of cauda equina syndrome for proper treatment. Acta orthop 2010 Jun;81(3):391-5. [1B]
- ↑ Fairbank J. Et al. Does patient history and physical examination predict MRI proven cauda equina syndrome? Evidence based spine care journal 2011; 2(4): 27-33. [Level Of Evidence: 1]
- ↑ Daniels, Eldra W., et al. "Review of medicolegal cases for cauda equina syndrome: what factors lead to an adverse outcome for the provider?." Orthopedics 35.3 (2012): e414-e419.[Level Of Evidence: 2A]
- ↑ 29.0 29.1 29.2 A. Gardner, E. Gardner and T. Morley, Cauda equina syndrome: a review of the current clinical and medico-legal position, Eur Spine J. 2011 May; 20(5): 690–697. [1A]
- ↑ 30.0 30.1 Wagih E.M., Management of Traumatic Spinal Cord Injuries: current standard of care revisited, ACNR, Volume 10 Nr.1, March/April 2010 [3A]
- ↑ Randhawa, Simret Singh, et al. "Neurological Recovery in Two Patients with Cauda Equina Syndrome Secondary to L5 Lumbar Spine Giant Cell Tumour after Treatment with Denosumab without Surgery." Asian Spine Journal 10.5 (2016): 945-949.[Level Of Evidence: 4]
- ↑ Emiliana B., Agostino Z., Cristina M., Epidemiology and clinical management of Conus-Cauda Syndrome and flaccid paraplegia in Friuli Venezia Giulia: Data of the Spinal Unit of Udine, Basic Applied Myology 19 (4): 163-167, 2009 [1B]
- ↑ Creasey GH., Craggs MD., Functional electrical stimulation for bladder, bowel and sexual function, Spinal Cord Injuries, 2012;109:247-57 [1A]
- ↑ 34.0 34.1 Karen M.B., Julie M.W., Timothy W.F., Lumbar spinal stenosis-diagnosis and management of the aging spine, Manual Therapy 16, 2011 (308-317) [1A]
- ↑ Kotil, Kadir, Bekir Mahmut Kilinc, and Turgay Bilge. "Spinal metastasis of occult lung carcinoma causing cauda equina syndrome." Journal of clinical neuroscience 14.4 (2007): 372-375.[Level Of Evidence 5]
- ↑ Le Rhun, Emilie, et al. "Prolonged Response and Restoration of Functional Independence with Bevacizumab plus Vinorelbine as Third-Line Treatment for Breast Cancer-Related Leptomeningeal Metastases." Case reports in oncology 8.1 (2015): 72-77.[Level Of Evidence 5]
- ↑ J. G. Kennedy, K. E. Soffe, A. McGrath, M. M. Stephens, Predictors of outcome in cauda equina syndrome, Eur Spine J, 12 april 1999. [2B]