Bronchitis: Difference between revisions
No edit summary |
(Etiology) |
||
| (14 intermediate revisions by 4 users not shown) | |||
| Line 1: | Line 1: | ||
<div class=" | <div class="editorbox">'''Original Editor '''-[[User:User name|The Open Physio project]] | ||
'''Top Contributors''' -{{Special:Contributors/{{FULLPAGENAME}}}} | |||
'''Original Editor '''- | |||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | |||
</div> | </div> | ||
== | == Introduction == | ||
[[ | Acute bronchitis is an inflammation of the large airways of the [[Lung Anatomy|lung]]. It is a common clinical presentation to an emergency department, urgent care center, and primary care office. About 5% of adults have an episode of acute bronchitis each year. An estimated 90% of these seek medical advice for the same. In the United States, acute bronchitis is among the top ten most common illness among outpatients. <ref name=":2">Singh A, Avula A, Zahn E. Acute Bronchitis. [Updated 2020 Nov 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-Available: https://www.ncbi.nlm.nih.gov/books/NBK448067/<nowiki/>( accessed24.5.2021)</ref> People with acute bronchitis usually complain of acute cough with or without sputum production, and signs of lower respiratory tract infection in the absence of chronic lung disease, such as chronic obstructive pulmonary disease, or an identified cause, such as pneumonia or sinusitis.<ref name=":3">Kinkade S, Long NA. [https://www.aafp.org/afp/2016/1001/p560.html Acute bronchitis. American family physician.] 2016 Oct 1;94(7):560-5.</ref> [[Image:Bronchitis.jpg|right|300px|alt=|frameless]] | ||
== Etiology == | |||
Acute bronchitis is caused by [[Infectious Disease|infection]] of the large airways commonly due to [[Viral Infections|viruses]] and is usually self-limiting.The most commonly identified viruses are rhinovirus, enterovirus, influenza A and B, parainfluenza, coronavirus, human metapneumovirus, and respiratory syncytial virus. <ref name=":3" /> [[Bacterial Infections|Bacterial]] infection is uncommon. Bacteria such as Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Bordetella pertussisare commonly detected in 1% to 10% of cases in people with acute bronchitis.<ref name=":3" /> Approximately 95% of acute bronchitis in healthy adults are secondary to viruses. It can sometimes be caused by allergens, irritants, and bacteria. Irritants include smoke inhalation, polluted air inhalation, dust.<ref name=":2" /> | |||
== | == Epidemiology == | ||
Acute bronchitis can affect people of all ages, but it is commonest in children, especially those under the age of 3 years. It is often associated with the common cold, a sore throat and/or flu.<ref name=":0">Radiopedia Bronchitis Available:https://radiopaedia.org/articles/acute-bronchitis (accessed 24.5.2021)</ref> | |||
== | == Pathophysiology == | ||
Acute bronchitis is the result of acute [[Inflammation Acute and Chronic|inflammation]] of the bronchi secondary to various triggers, most commonly viral infection, allergens, pollutants, etc. Inflammation of the bronchial wall leads to mucosal thickening, epithelial-cell desquamation, and denudation of the basement membrane. At times, a viral upper respiratory infection can progress to infection of the lower respiratory tract resulting in acute bronchitis. | |||
=== Contributory or Predisposing Factors === | === Contributory or Predisposing Factors === | ||
*Bronchiectasis | *[[Bronchiectasis]] | ||
*Cystic Fibrosis | *[[Cystic Fibrosis]] | ||
*Congestive heart failure | *Congestive heart failure | ||
*Some children may be more prone to the contraction of acute bronchitis than others and these include children with respiratory illnesses such as [[asthma]] and children exposed to high levels of airborne pollutants. | |||
Some children may be more prone to the contraction of acute bronchitis than others and these include children with respiratory illnesses such as asthma and children exposed to high levels of airborne pollutants. | |||
== Signs and Symptoms == | == Signs and Symptoms == | ||
| Line 67: | Line 27: | ||
=== General Symptoms === | === General Symptoms === | ||
The main symptom is a hacking cough that may be associated with sputum production. Sputum is usually yellow or clear and different from the green sputum that is more often associated with lower respiratory tract infections. | |||
Patients will often have nasal and sinus infection and describe a runny nose or sinus symptoms which include pain. As well as cough and sputum production, patients may describe other general symptoms including wheezing, shortness of breath, chest pain and headache .<ref name=":0" />. | |||
== Diagnosis == | == Diagnosis == | ||
[[File:Bronchitis2.png|thumb]] | [[File:Bronchitis2.png|thumb]] | ||
Acute bronchitis is a clinical diagnosis based on history, past medical history, lung exam, and other physical findings. Oxygen saturation plays an important role in judging the severity of the disease along with the [[Pulse rate|pulse rate,]] temperature, and respiratory rate. No further workup is needed if vital signs are normal, no exam findings suggestive of [[pneumonia]]. An exception to this rule is elderly patients >75 years old. Also, further workup is needed when pneumonia is suspected, clinical diagnosis is in question or in cases of high suspicion for [[influenza]] or pertussis . | |||
Tests may include: | |||
= | * '''[[Chest X-Rays|Chest X-ray]]''' This test is used to rule out pneumonia. In bronchitis, the x-ray will show no evidence of lung infiltrates or consolidation. Occasionally, chest x-ray shows increased interstitial markings consistent with thickening of bronchial walls.<ref name=":1">Singh A, Avula A, Zahn E. [https://www.ncbi.nlm.nih.gov/books/NBK448067/ Acute Bronchitis.] InStatPearls [Internet] 2019 Jul 29. StatPearls Publishing.</ref> | ||
This allows the doctor to check for signs of inflammation or a bacterial infection | * '''Sputum Culture''' This allows the doctor to check for signs of inflammation or a bacterial infection<ref name=":1" /> | ||
* '''[[Blood Tests]]''' These tests include arterial blood gases to test for levels of oxygen, carbon dioxide and acidity of the blood. Complete blood count and chemistry may be done as a workup for fever. White blood count might be mildly elevated in some cases. Blood chemistry can reflect [[dehydration]] changes.<ref name=":1" /> | |||
These tests include arterial blood gases to test for levels of oxygen, carbon dioxide and acidity of the blood. Complete blood count and chemistry may be done as a workup for fever. White blood count might be mildly elevated in some cases. Blood chemistry can reflect dehydration changes | |||
== Differential Diagnosis == | == Differential Diagnosis == | ||
| Line 162: | Line 47: | ||
* [[Bronchiolitis]] | * [[Bronchiolitis]] | ||
* [[COPD (Chronic Obstructive Pulmonary Disease)|COPD]] | * [[COPD (Chronic Obstructive Pulmonary Disease)|COPD]] | ||
* GERD | * [[Gastroesophageal Reflux Disease|GERD]] | ||
* Viral pharyngitis | * Viral pharyngitis | ||
* [[Heart Failure]] | * [[Heart Failure]] | ||
| Line 168: | Line 53: | ||
== Medical Management == | == Medical Management == | ||
Treatment is focused on patient education and supportive care. [[Antibiotics]] are not needed for the great majority of patients with acute bronchitis but are greatly overused for this condition. Reducing antibiotic use for acute bronchitis is a national and international health care priority<ref>Uptodate Acute Bronchitis Available: https://www.uptodate.com/contents/acute-bronchitis-in-adults/print ( accessed 24.5.2021)</ref> | |||
Treatment is supportive, consisting of analgesia and sometimes bronchodilators.<ref name=":0" />. | |||
== Physiotherapy Management == | == Physiotherapy Management == | ||
The main aim of Physiotherapy is to keep the airways open and functioning properly. Physiotherapists are able to do this using different techniques such as: ( see [[Respiratory Physiotherapy]]) | |||
* '''Postural Drainage''' This can be exercised at an angle of 45º in prone and in side lying. This must first be cleared with the institution as necessary, as well as considering possible contra-indications such as a head injury. | |||
[[Percussion]], shaking and vibrations can be used to mobilize secretions and aid expectoration.<ref>Sutton PP, Pavia D, Bateman JR, Clarke SW. [https://europepmc.org/article/med/7047185 Chest physiotherapy: a review.] European journal of respiratory diseases. 1982 May 1;63(3):188-201.</ref> Once again, precautions and contra-indications are to be observed. | * '''Manual Techniques'''[[Percussion]], shaking and vibrations can be used to mobilize secretions and aid expectoration.<ref>Sutton PP, Pavia D, Bateman JR, Clarke SW. [https://europepmc.org/article/med/7047185 Chest physiotherapy: a review.] European journal of respiratory diseases. 1982 May 1;63(3):188-201.</ref> Once again, precautions and contra-indications are to be observed. | ||
* '''Breathing Exercises'''[[Active Cycle of Breathing Technique]](ACBT) could be used in order to mobilize secretions. Teaching relaxed breathing techniques as well as diaphragmatic breathing to aid oxygenation and prevent respiratory distress. Full thoracic expansion must be emphasized which will aid oxygenation. The patient should be encouraged to aid the mobilization of secretions through coughing and deep breathing during the day. The patient, and family, should be advised that the patient needs to rest and avoid bronchial irritants where possible. This, however, does not exempt the patient from partaking in physiotherapeutic activities. | |||
* '''Education''' Teaching the importance of nose blowing into a tissue and not swallowing the secretions as well as discarding the tissue safely after blowing their nose is important,s as this will prevent the spread of infection. The patient and family/caregiver should be advised that a dry cough may persist afree bronchitis has resolved due to irritation of the respiratory passages. A humidifier at the bedside may be useful in combating the negative after-effects as it will saturate the air that is breathed in. | |||
[[Active Cycle of Breathing Technique]](ACBT) could be used in order to mobilize secretions. Teaching relaxed breathing techniques as well as diaphragmatic breathing to aid oxygenation and prevent respiratory distress. Full thoracic expansion must be emphasized which will aid oxygenation. | * '''Treatment Schedule and Home Advice''' Treatment should be carried out 3 to 4 times a day depending on the severity of the condition. If an upper respiratory tract infection is contracted again, treatment should be started as soon as possible to prevent it from developing into bronchitis or further severe complications. The patient and/or family should be able to recognize early signs and symptoms of acute bronchitis and report them immediately. | ||
The patient should be encouraged to aid the mobilization of secretions through coughing and deep breathing during the day. The patient, and family, should be advised that the patient needs to rest and avoid bronchial irritants where possible. This, however, does not exempt the patient from partaking in physiotherapeutic activities. | |||
Teaching the importance of nose blowing into a tissue and not swallowing the secretions as well as discarding the tissue safely after blowing their nose is important,s as this will prevent the spread of infection. The patient and family/caregiver should be advised that a dry cough may persist afree bronchitis has resolved due to irritation of the respiratory passages. A humidifier at the bedside may be useful in combating the negative after-effects as it will saturate the air that is breathed in. | |||
Treatment should be carried out 3 to 4 times a day depending on the severity of the condition. If an upper respiratory tract infection is contracted again, treatment should be started as soon as possible to prevent it from developing into bronchitis or further severe complications. | |||
The patient and/or family should be able to recognize early signs and symptoms of acute bronchitis and report them immediately. | |||
{| width="100%" cellspacing="1" cellpadding="1" | {| width="100%" cellspacing="1" cellpadding="1" | ||
| Line 239: | Line 77: | ||
<ref>Lord of Phisiotherapy. Postural Drainage. Available from: http://www.youtube.com/watch?v=TPZsP1ujg0U[last accessed 08/02/13]</ref> <ref>enmurrcp. RT Chest Physiotherapy Demonstration. Available from: http://www.youtube.com/watch?v=ErMTXJLE5es[last accessed 08/02/13]</ref> <ref>pbg03. Active Cycle of Breathing Technique . Available from: http://www.youtube.com/watch?v=hq32_LThDE4[last accessed 08/02/13]</ref> | <ref>Lord of Phisiotherapy. Postural Drainage. Available from: http://www.youtube.com/watch?v=TPZsP1ujg0U[last accessed 08/02/13]</ref> <ref>enmurrcp. RT Chest Physiotherapy Demonstration. Available from: http://www.youtube.com/watch?v=ErMTXJLE5es[last accessed 08/02/13]</ref> <ref>pbg03. Active Cycle of Breathing Technique . Available from: http://www.youtube.com/watch?v=hq32_LThDE4[last accessed 08/02/13]</ref> | ||
== Prognosis == | == Prognosis == | ||
Acute bronchitis is self-limiting and resolves with symptomatic treatment in most of the instances. Secondary pneumonia is possible. Rare cases of acute respiratory distress syndrome and respiratory failure have been reported in the literature.<ref name=":2" /> | |||
== Prevention Of Paediatric Bronchitis == | |||
Rare cases of acute respiratory distress syndrome and respiratory failure have | |||
== Prevention == | |||
In paediatric bronchitis as well as other medical conditions, prevention is always better than cure. | |||
Children suffering from bronchitis should always have a balanced diet and healthy eating plan in order to keep their immune system in an optimal condition. This allows it to fight off infection and prevent the development of acute bronchitis, disrupting daily life along with general well-being. | * Hands should be washed regularly to avoid the spreading of any viruses and other infections.<ref>Fleming DM, Elliot AJ. [https://www.tandfonline.com/doi/full/10.1517/14656566.8.4.415 The management of acute bronchitis in children.] Expert Opinion on Pharmacotherapy. 2007 Mar 1;8(4):415-26.</ref> A hand should be placed over the mouth during coughing, and the washing ones' hands after a cough will aid in the removal of any viruses or germs on the hands. If this is not observed, it may lead to the spread of infection. | ||
* If and where possible, exposure to air pollution should be reduced. Smoking near children should be prevented as secondary smoke can damage the bronchial tree and makes it easier for viruses to cause an infection. | |||
* If the child is easily susceptible to contracting infections, contact with people who are already suffering from bronchitis should be avoided. | |||
* Antimicrobial therapy should be administered at the first sign of purulent sputum. | |||
* Children suffering from bronchitis should always have a balanced diet and healthy eating plan in order to keep their immune system in an optimal condition. This allows it to fight off infection and prevent the development of acute bronchitis, disrupting daily life along with general well-being. | |||
== References == | == References == | ||
| Line 262: | Line 95: | ||
[[Category:Glasgow_Caledonian_University_Project]] | [[Category:Glasgow_Caledonian_University_Project]] | ||
[[Category:Acute Respiratory Disorders - Conditions]] | [[Category:Acute Respiratory Disorders - Conditions]] | ||
[[Category:Conditions]] | |||
Latest revision as of 12:15, 4 January 2022
Top Contributors -Tehseen Zahra, Admin, George Prudden, Lucinda hampton, Laura Ritchie, Rachael Lowe, Kim Jackson, Sai Kripa, Tony Lowe, Evan Thomas, Scott Buxton and WikiSysop
Introduction[edit | edit source]
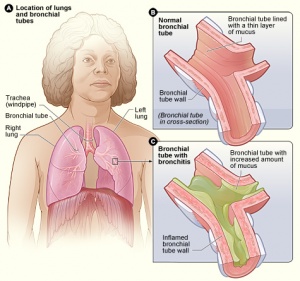
Acute bronchitis is an inflammation of the large airways of the lung. It is a common clinical presentation to an emergency department, urgent care center, and primary care office. About 5% of adults have an episode of acute bronchitis each year. An estimated 90% of these seek medical advice for the same. In the United States, acute bronchitis is among the top ten most common illness among outpatients. [1] People with acute bronchitis usually complain of acute cough with or without sputum production, and signs of lower respiratory tract infection in the absence of chronic lung disease, such as chronic obstructive pulmonary disease, or an identified cause, such as pneumonia or sinusitis.[2]
Etiology[edit | edit source]
Acute bronchitis is caused by infection of the large airways commonly due to viruses and is usually self-limiting.The most commonly identified viruses are rhinovirus, enterovirus, influenza A and B, parainfluenza, coronavirus, human metapneumovirus, and respiratory syncytial virus. [2] Bacterial infection is uncommon. Bacteria such as Mycoplasma pneumoniae, Chlamydophila pneumoniae, and Bordetella pertussisare commonly detected in 1% to 10% of cases in people with acute bronchitis.[2] Approximately 95% of acute bronchitis in healthy adults are secondary to viruses. It can sometimes be caused by allergens, irritants, and bacteria. Irritants include smoke inhalation, polluted air inhalation, dust.[1]
Epidemiology[edit | edit source]
Acute bronchitis can affect people of all ages, but it is commonest in children, especially those under the age of 3 years. It is often associated with the common cold, a sore throat and/or flu.[3]
Pathophysiology[edit | edit source]
Acute bronchitis is the result of acute inflammation of the bronchi secondary to various triggers, most commonly viral infection, allergens, pollutants, etc. Inflammation of the bronchial wall leads to mucosal thickening, epithelial-cell desquamation, and denudation of the basement membrane. At times, a viral upper respiratory infection can progress to infection of the lower respiratory tract resulting in acute bronchitis.
Contributory or Predisposing Factors[edit | edit source]
- Bronchiectasis
- Cystic Fibrosis
- Congestive heart failure
- Some children may be more prone to the contraction of acute bronchitis than others and these include children with respiratory illnesses such as asthma and children exposed to high levels of airborne pollutants.
Signs and Symptoms[edit | edit source]
The signs and symptoms of this disorder will depend on the severity of the disease as well as considering which stage the disease has been diagnosed. This just means that some symptoms may be present in some cases and may be absent in others.
General Symptoms[edit | edit source]
The main symptom is a hacking cough that may be associated with sputum production. Sputum is usually yellow or clear and different from the green sputum that is more often associated with lower respiratory tract infections.
Patients will often have nasal and sinus infection and describe a runny nose or sinus symptoms which include pain. As well as cough and sputum production, patients may describe other general symptoms including wheezing, shortness of breath, chest pain and headache .[3].
Diagnosis[edit | edit source]
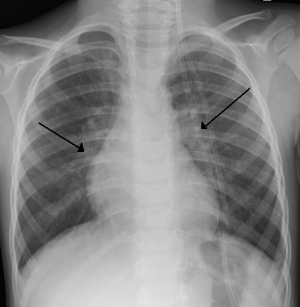
Acute bronchitis is a clinical diagnosis based on history, past medical history, lung exam, and other physical findings. Oxygen saturation plays an important role in judging the severity of the disease along with the pulse rate, temperature, and respiratory rate. No further workup is needed if vital signs are normal, no exam findings suggestive of pneumonia. An exception to this rule is elderly patients >75 years old. Also, further workup is needed when pneumonia is suspected, clinical diagnosis is in question or in cases of high suspicion for influenza or pertussis .
Tests may include:
- Chest X-ray This test is used to rule out pneumonia. In bronchitis, the x-ray will show no evidence of lung infiltrates or consolidation. Occasionally, chest x-ray shows increased interstitial markings consistent with thickening of bronchial walls.[4]
- Sputum Culture This allows the doctor to check for signs of inflammation or a bacterial infection[4]
- Blood Tests These tests include arterial blood gases to test for levels of oxygen, carbon dioxide and acidity of the blood. Complete blood count and chemistry may be done as a workup for fever. White blood count might be mildly elevated in some cases. Blood chemistry can reflect dehydration changes.[4]
Differential Diagnosis[edit | edit source]
Other causes of acute cough should be considered especially when a cough persists for longer than 3 weeks.
- Asthma: Acute asthma is misdiagnosed as acute bronchitis in approximately one-third of the patients who present with acute cough.
- Acute/chronic sinusitis
- Bronchiolitis
- COPD
- GERD
- Viral pharyngitis
- Heart Failure
- Pulmonary Embolism[4]
Medical Management[edit | edit source]
Treatment is focused on patient education and supportive care. Antibiotics are not needed for the great majority of patients with acute bronchitis but are greatly overused for this condition. Reducing antibiotic use for acute bronchitis is a national and international health care priority[5]
Treatment is supportive, consisting of analgesia and sometimes bronchodilators.[3].
Physiotherapy Management[edit | edit source]
The main aim of Physiotherapy is to keep the airways open and functioning properly. Physiotherapists are able to do this using different techniques such as: ( see Respiratory Physiotherapy)
- Postural Drainage This can be exercised at an angle of 45º in prone and in side lying. This must first be cleared with the institution as necessary, as well as considering possible contra-indications such as a head injury.
- Manual TechniquesPercussion, shaking and vibrations can be used to mobilize secretions and aid expectoration.[6] Once again, precautions and contra-indications are to be observed.
- Breathing ExercisesActive Cycle of Breathing Technique(ACBT) could be used in order to mobilize secretions. Teaching relaxed breathing techniques as well as diaphragmatic breathing to aid oxygenation and prevent respiratory distress. Full thoracic expansion must be emphasized which will aid oxygenation. The patient should be encouraged to aid the mobilization of secretions through coughing and deep breathing during the day. The patient, and family, should be advised that the patient needs to rest and avoid bronchial irritants where possible. This, however, does not exempt the patient from partaking in physiotherapeutic activities.
- Education Teaching the importance of nose blowing into a tissue and not swallowing the secretions as well as discarding the tissue safely after blowing their nose is important,s as this will prevent the spread of infection. The patient and family/caregiver should be advised that a dry cough may persist afree bronchitis has resolved due to irritation of the respiratory passages. A humidifier at the bedside may be useful in combating the negative after-effects as it will saturate the air that is breathed in.
- Treatment Schedule and Home Advice Treatment should be carried out 3 to 4 times a day depending on the severity of the condition. If an upper respiratory tract infection is contracted again, treatment should be started as soon as possible to prevent it from developing into bronchitis or further severe complications. The patient and/or family should be able to recognize early signs and symptoms of acute bronchitis and report them immediately.
Prognosis[edit | edit source]
Acute bronchitis is self-limiting and resolves with symptomatic treatment in most of the instances. Secondary pneumonia is possible. Rare cases of acute respiratory distress syndrome and respiratory failure have been reported in the literature.[1]
Prevention Of Paediatric Bronchitis[edit | edit source]
In paediatric bronchitis as well as other medical conditions, prevention is always better than cure.
- Hands should be washed regularly to avoid the spreading of any viruses and other infections.[10] A hand should be placed over the mouth during coughing, and the washing ones' hands after a cough will aid in the removal of any viruses or germs on the hands. If this is not observed, it may lead to the spread of infection.
- If and where possible, exposure to air pollution should be reduced. Smoking near children should be prevented as secondary smoke can damage the bronchial tree and makes it easier for viruses to cause an infection.
- If the child is easily susceptible to contracting infections, contact with people who are already suffering from bronchitis should be avoided.
- Antimicrobial therapy should be administered at the first sign of purulent sputum.
- Children suffering from bronchitis should always have a balanced diet and healthy eating plan in order to keep their immune system in an optimal condition. This allows it to fight off infection and prevent the development of acute bronchitis, disrupting daily life along with general well-being.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Singh A, Avula A, Zahn E. Acute Bronchitis. [Updated 2020 Nov 20]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-Available: https://www.ncbi.nlm.nih.gov/books/NBK448067/( accessed24.5.2021)
- ↑ 2.0 2.1 2.2 Kinkade S, Long NA. Acute bronchitis. American family physician. 2016 Oct 1;94(7):560-5.
- ↑ 3.0 3.1 3.2 Radiopedia Bronchitis Available:https://radiopaedia.org/articles/acute-bronchitis (accessed 24.5.2021)
- ↑ 4.0 4.1 4.2 4.3 Singh A, Avula A, Zahn E. Acute Bronchitis. InStatPearls [Internet] 2019 Jul 29. StatPearls Publishing.
- ↑ Uptodate Acute Bronchitis Available: https://www.uptodate.com/contents/acute-bronchitis-in-adults/print ( accessed 24.5.2021)
- ↑ Sutton PP, Pavia D, Bateman JR, Clarke SW. Chest physiotherapy: a review. European journal of respiratory diseases. 1982 May 1;63(3):188-201.
- ↑ Lord of Phisiotherapy. Postural Drainage. Available from: http://www.youtube.com/watch?v=TPZsP1ujg0U[last accessed 08/02/13]
- ↑ enmurrcp. RT Chest Physiotherapy Demonstration. Available from: http://www.youtube.com/watch?v=ErMTXJLE5es[last accessed 08/02/13]
- ↑ pbg03. Active Cycle of Breathing Technique . Available from: http://www.youtube.com/watch?v=hq32_LThDE4[last accessed 08/02/13]
- ↑ Fleming DM, Elliot AJ. The management of acute bronchitis in children. Expert Opinion on Pharmacotherapy. 2007 Mar 1;8(4):415-26.