Breathing Pattern Disorders: Difference between revisions
mNo edit summary |
mNo edit summary |
||
| Line 34: | Line 34: | ||
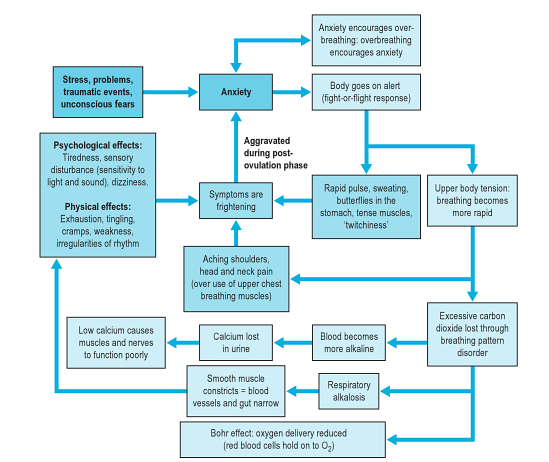
This diagram below (from <ref name="Chaitow">Chaitow, L., Bradley, D. and Gilbert, C. [http://bit.ly/1fe2oIE Recognizing and Treating Breathing Disorders]. Elsevier, 2014</ref>) shows the stress-anxiety-breathing flow chart demonstrating multiple possible effects and influences of breathing pattern disorders. | This diagram below (from <ref name="Chaitow">Chaitow, L., Bradley, D. and Gilbert, C. [http://bit.ly/1fe2oIE Recognizing and Treating Breathing Disorders]. Elsevier, 2014</ref>) shows the stress-anxiety-breathing flow chart demonstrating multiple possible effects and influences of breathing pattern disorders. | ||
[[Image:Breathing-pattern-disorders-flow-chart.png|center|Stress-anxiety-breathing flow chart showing multiple possible effects and influences of breathing pattern disorders]]<br> | |||
== Clinical Presentation == | == Clinical Presentation == | ||
Breathing pattern disorders manifest differently based on the individual. Some people may exhibit high levels of anxiety/fear whereas others have more musculoskeletal symptoms, chronic pain and fatigue.<ref name=":0" /> Over 30 possible symptoms have been described in relation to BPDs/HVS.<ref name=":0" /> | Breathing pattern disorders manifest differently based on the individual. Some people may exhibit high levels of anxiety/fear whereas others have more musculoskeletal symptoms, chronic pain and fatigue.<ref name=":0" /> Over 30 possible symptoms have been described in relation to BPDs/HVS.<ref name=":0" /> | ||
Typical symptoms can include: | Typical symptoms can include: | ||
| Line 146: | Line 146: | ||
[[Category:Chronic Respiratory Disease - Conditions]] | [[Category:Chronic Respiratory Disease - Conditions]] | ||
[[Category:Conditions]] | [[Category:Conditions]] | ||
[[Category:Course Pages]] | |||
Revision as of 19:37, 22 January 2020
Original Editor - Leon Chaitow
Top Contributors - Rachael Lowe, Leon Chaitow, Admin, Kim Jackson, Jess Bell, Ewa Jaraczewska, Wanda van Niekerk, Khloud Shreif, Tarina van der Stockt, Fasuba Ayobami, WikiSysop, Lucinda hampton, 127.0.0.1, Ajay Upadhyay, Marleen Moll, Olajumoke Ogunleye, Evan Thomas, Scott Buxton and Venus Pagare
Topic Expert - Leon Chaitow
Introduction[edit | edit source]
Breathing Pattern Disorders (BPD) or Dysfunctional Breathing are abnormal respiratory patterns, specifically related to over-breathing. They range from simple upper chest breathing to, at the extreme end of the scale, hyperventilation (HVS).[1]
Dysfunctional breathing (DB) is defined as chronic or recurrent changes in the breathing pattern that cannot be attributed to a specific medical diagnosis, causing respiratory and non-respiratory complaints.[1] It is not a disease process, but rather alterations in breathing patterns that interfere with normal respiratory processes. BPD can, however, co-exist with diseases such as COPD or heart disease.[2][3]
BPDs are whole person problems - dysfunctional breathing can destabilise mind, muscles, mood and metabolism.[4] They can play a part in, for instance, premenstrual syndrome,[5] chronic fatigue,[6] neck, back and pelvic pain,[7][8] fibromyalgia[9] [10] and some aspects of anxiety and depression.[1][11]
Clinically Relevant Anatomy[edit | edit source]
The human respiratory system is located in the thorax. The thoracic wall consists of skeletal and muscular components, extending between the 1st rib superiorly and the 12th rib, the costal margin and the xiphoid process inferiorly.[12] The respiratory system can be classified in terms of function and anatomy. Functionally, it is divided into two zones. The conducting zone extends from the nose to the bronchioles and serves as a pathway for conduction of inhaled gases. The respiratory zone is the second area and it is the site for gaseous exchange. It comprises of alveolar duct, alveolar sac and alveoli. Anatomically, it is divided into the upper and lower respiratory tract. The upper respiratory tract starts proximally from the nose and ends at the larynx while the lower respiratory tract continues from the trachea to the alveoli distally.[13]
Epidemiology[edit | edit source]
Around 10% of patients in a population are diagnosed with hyperventilation syndrome.[14] However, many more people have subtle, yet clinically significant, breathing pattern disorders. Dysfunctional breathing is more prevalent in women (14%) than in men (2%).[14]
Little is known about dysfunctional breathing in children. Preliminary data suggest 5.3% or more of children with asthma have dysfunctional breathing and that, unlike in adults, it is associated with poorer asthma control. It is not known what proportion of the general pediatric population is affected.[15]
Etiology[edit | edit source]
Breathing pattern disorders occur when ventilation exceeds metabolic demands, resulting in symptom-producing haemodynamic and chemical changes. Habitual failure to fully exhale - involving an upper chest breathing pattern - may lead to hypocapnia - ie a deficiency of carbon dioxide in the blood. The result is respiratory alkalosis, and eventually hypoxia, or the reduction of oxygen delivery to tissue.[16] [17]
As well as having a marked effect on the biochemistry of the body, BPDs can influence emotions[18], circulation, digestive function as well as musculoskeletal structures involved in the respiratory process. Essentially a sympathetic state and a subtle, yet a fairly constant state of fight-or-flight becomes prevalent. This can cause anxiety, as well as changes in blood pH, muscle tone, pain threshold, and many central and peripheral nervous system symptoms. So despite not being a disease, BPDs are capable of producing symptoms that mimic pathological processes, including gastrointestinal or cardiac problems.[2][3]
Musculoskeletal imbalances often exist in patients with BPDs. These may result from a pre-existing contributing factor or may be caused by the dysfunctional breathing pattern.[19] Types of imbalances include loss or thoracic mobility, overuse/tension in accessory respiratory muscles and dysfunctional postures that affect the movement of the chest wall, as well as exacerbating poor diaphragmatic descent.[19]
This diagram below (from [20]) shows the stress-anxiety-breathing flow chart demonstrating multiple possible effects and influences of breathing pattern disorders.
Clinical Presentation[edit | edit source]
Breathing pattern disorders manifest differently based on the individual. Some people may exhibit high levels of anxiety/fear whereas others have more musculoskeletal symptoms, chronic pain and fatigue.[19] Over 30 possible symptoms have been described in relation to BPDs/HVS.[19]
Typical symptoms can include:
- Frequent sighing and yawning
- Breathing discomfort
- Disturbed sleep
- Erratic heartbeats
- Feeling anxious and uptight
- Pins and needles
- Upset gut/nausea
- Clammy hands
- Chest Pains
- Shattered confidence
- Tired all the time
- Achy muscles and joints
- Dizzy spells or feeling spaced out
- Irritability or hypervigilance
- Feeling of 'air hunger'
- Breathing discomfort
- There may also be a correlation between BPD and low back pain.[21]
Co-existing Problems[edit | edit source]
Asthma and COPD[edit | edit source]
During an acute asthma attack, patients adopt a breathing pattern that is similar to the pattern seen in BPD:
- hyper-inflated
- rapid
- upper chest
- shallow[19]
It is therefore believed that patients with chronic asthma may be more likely to develop BPDs.[19] Thus, after an acute attack, it is important to re-establish abdominal/nose breathing patterns and normalised CO2 levels.[20] Similarly, exercise is commonly considered a trigger for asthma, but in some patients, their breathlessness may actually be due to hyperinflation and the increased respiratory effort from faulty breathing patterns.[19]
Chronic Rhinosinusitis (CRS)[edit | edit source]
Chronic mouth breathing often occurs with CRS and can, therefore, result in a chronic breathing pattern dysfunction. Saline nasal rises and eucalyptus steam inhalations can ease sinus congestion and restore nasal breathing. Because CRS is common in HVS/BPD patients, restoring nose breathing is a high priority in breathing retraining programmes.[20]
Chronic Pain[edit | edit source]
Chronic pain and chronic hyperventilation often co-exist. Pain can cause an increase in respiratory rates generally. Moreover, patients with abdominal or pelvic pain often splint their abdominal muscles, which results in upper chest breathing. When treating patients with chronic pain, it is important to work towards achieving nose/abdominal breathing, as well as promoting relaxation.[20]
Hormonal Influences[edit | edit source]
Progesterone is a respiratory stimulant. As it peaks in the post-ovulation phase, it may drive PaCO2 levels down. These levels further reduce in pregnancy.[20] It has been found that patients with PMS can benefit from breathing retraining and education to reduce any symptoms related to HVS.[20] Similarly, peri/postmenopausal women who cannot take HRT have been shown to benefit from breathing retraining to improve sleep and reduce hot flushes.[20]
Diagnostic Procedures[edit | edit source]
Capnography[edit | edit source]
Capnography is a reliable diagnostic tool for BPDs. It measures the average CO2 partial pressure at the end of exhalation (End Tidal CO2).[22][23]
Nijmegan Questionnaire[edit | edit source]
High scores on the Nijmegan questionnaire have been shown to be both sensitive and specific for detecting people with tendencies consistent with breathing pattern disorders. The sensitivity of the Nijmegen Questionnaire in relation to the clinical diagnosis was 91% and the specificity 95%[24]
Assessment of Breathing Patterns[edit | edit source]
- Breath Holding – Ask the patient to exhale and then hold his/her breath. People are usually able to hold their breath for 25 to 30 seconds.[25] If a patient holds less than 15 seconds, it may indicate low tolerance to carbon dioxide.
- Breathing Hi-Low Test - Patient is either seated or supine – Place your hands on the patient’s chest and stomach. Ask the patient to exhale fully and then inhale normally. Observe where the movement initiates and where the most movement occurs. Look specifically for lateral expansion and upward hand pivot.[25]
- Breathing Wave – Patient lies prone. Ask him/her to breathe normally. The spine should move in a wave-like pattern towards the head. Segments that rise as a group may represent thoracic restrictions.[25]
- Seated Lateral Expansion – Place hands on lower thorax and monitor motion while breathing. Looking for symmetrical lateral expansion.[25]
- Manual Assessment of Respiratory Motion (MARM) - Assess and quantify breathing pattern, in particular, the distribution of breathing motion between the upper and lower parts of the rib cage and abdomen under various conditions. It is a manual technique that once acquired is practical, quick and inexpensive.[26]
- Sniff Test - Assesses bilateral diaphragm function. It is useful in assessing for upper or lower chest pattern dominance. The therapist places his/her hand 3 fingers below the patients xiphoid process. The patient performs a quick sniff. The therapist should feel an outward movement of the abdominal wall. This indicates that both hemi-diaphragms are working. Upper chest breathers usually have no diaphragmatic excursion or they may in-draw their abdominal wall.[25]
- Respiratory Induction Plethysmography (RIP) and Magnetometry
Assessment of the Musculoskeletal System[edit | edit source]
- Observe for elevated and depressed ribs and clavicle with rib palpation techniques.
- Check for muscle tone and length especially in the psoas, quadratus lumborum, latissimus dorsi, upper trapezius, scalene, and sternocleidomastoid.
- Assess for alterations in the mobility of the thoracic and rib articulations.
Assessment of Respiratory Function[edit | edit source]
- Oximetry - to measure oxygen saturation (SpO2)
- Capnography - to measure end-tidal CO2 levels in exhaled air (as described above)
- Peak expiratory flow rate - the highest flow of air out of the lungs from peak inspiration in a fast single forced breath out
- Manual Assessment of Respiratory Motion (MARM)
Outcome Measures[edit | edit source]
- Nijmegen Questionnaire
- Rowley Breathing Self-Efficacy Scale (RoBE)[27]
- Self Evaluation of Breathing Questionnaire )SEBQ)[28]
- Hospital Anxiety and Depression Questionnaire (HAD)[29]
Differential Diagnosis[edit | edit source]
BPDs can often mimic more serious conditions such as cardiac, neurological and gastrointestinal conditions. These must all be ruled out by the medical team.
Management[edit | edit source]
For information on the management of BPDs, click here.
Key Evidence[edit | edit source]
- Breathing pattern disorders and functional movement. Bradley H, Dr Esformes J. Int J Sports Phys Ther. 2014 Feb;9(1):28-39.
- Breathing exercises for dysfunctional breathing/hyperventilation syndrome in children. Barker NJ, Jones M, O'Connell NE, Everard ML.
Cochrane Database Syst Rev. 2013 Dec 18;12:CD010376. - Breathing exercises for dysfunctional breathing/hyperventilation syndrome in adults. Jones M, Harvey A, Marston L, O'Connell NE.
Cochrane Database Syst Rev. 2013 May 31;5:CD009041.
Resources[edit | edit source]
- Low Back Pain and Breathing Pattern Disorders
- Leon Chaitow's website
- Website containing videos to go with the book - Recognizing and Treating Breathing Pattern Disorders[20]
- Clinical interest group for physiotherapists interested in hyperventilation
References[edit | edit source]
- ↑ 1.0 1.1 1.2 Lum L 1987 Hyperventilation syndromes in medicine and psychiatry: a review. J. R Soc Med. 80:229-231.
- ↑ 2.0 2.1 Sueda S et al. 2004 Clinical impact of selective spasm provocation tests Coron Artery Dis 15(8):491–497
- ↑ 3.0 3.1 Ajani A 2007 The mystery of coronary artery spasm Heart, Lung & Circulation 16:10–15
- ↑ Peters, D. Foreword In: Recognizing and Treating Breathing Disorders. Chaitow, L., Bradley, D. and Gilbert, C. Elsevier, 2014
- ↑ Ott H et al 2006 Symptoms of premenstrual syndrome may be caused by hyperventilation Fertility and Sterility 86(4):1001.e17-1001.e19
- ↑ Nixon P, Andrews J. 1996 A study of anaerobic threshold in chronic fatigue syndrome (CFS). Biol Psychol. 43:264
- ↑ Smith M Russell A Hodges, P 2006. Disorders of breathing and continence have a stronger association with back pain than obesity and physical activity. Australian Journal of Physiotherapy 21(52):11-16
- ↑ Haugstad G Haugstad T Kirste U 2006a Posture, movement patterns, and body awareness in women with chronic pelvic pain. J Psychosom Res. 61(5):637-644
- ↑ Naschitz J et al. 2006 Patterns of hypocapnia on tilt in patients with fibromyalgia, chronic fatigue syndrome, nonspecific dizziness, and neurally mediated syncope. Am J Med Sci. 331:295-303
- ↑ Dunnett A et al. 2007 The diagnosis of fibromyalgia in women may be influenced by menstrual cycle phase. Journal of Bodywork and Movement Therapies 11:99-105
- ↑ Han J et al 1996 Influence of breathing therapy on complaints, anxiety and breathing pattern in patients with hyperventilation syndrome and anxiety disorders. J Psychosom Res. 41:481-493
- ↑ Kennedy JW (2012). Clinical Anatomy Series‐Lower Respiratory Tract Anatomy. Scottish Universities Medical Journal.1 (2).p174‐179
- ↑ Patwa A, Shah A. Anatomy and physiology of respiratory system relevant to anaesthesia. Indian J Anaesth 2015;59:533‑41
- ↑ 14.0 14.1 Thomas M1, McKinley RK, Freeman E, Foy C, Price D.The prevalence of dysfunctional breathing in adults in the community with and without asthma. Prim Care Respir J. 2005 Apr;14(2):78-82.
- ↑ Barker, Nicola J et al. Breathing exercises for dysfunctional breathing/hyperventilation syndrome in children. National Library of Medicine. The Cochrane database of systematic reviews12 (2013): CD010376.
- ↑ Biff F. Palmer 2012 Evaluation and Treatment of Respiratory Alkalosis Am J Kidney Dis. 60(5):834-838.
- ↑ Jensen F 2004 Red blood cell pH, the Bohr effect, and other oxygenation-linked phenomena in blood O2 and CO2 transport Acta Physiologica Scandinavica 182(3):215-227
- ↑ van Dixhoorn J 2007. Whole-Body breathing: a systems perspective on respiratory retraining. In: Lehrer P et al . (Eds.) Principles and practice of stress management. Guilford Press. NY pp. 291–332
- ↑ 19.0 19.1 19.2 19.3 19.4 19.5 19.6 Clifton‐Smith T, Rowley J. Breathing pattern disorders and physiotherapy: inspiration for our profession. Phys Ther Rev. 2011; 16: 75–86.
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 20.7 Chaitow, L., Bradley, D. and Gilbert, C. Recognizing and Treating Breathing Disorders. Elsevier, 2014
- ↑ McLaughlin L, Goldsmith CH, Coleman K. Breathing evaluation and retraining as an adjunct to manual therapy Man Ther. 2011 Feb;16(1):51-2.
- ↑ Bradley H, Esformes J. Breathing pattern disorders and functional movement. Int J Sports Phys Ther. 2014 Feb;9(1):28-39.
- ↑ McLaughlin L. Breathing evaluation and retraining in manual therapy. J Bodyw Mov Ther. 2009 Jul;13(3):276-82. doi: 10.1016/j.jbmt.2009.01.005. Epub 2009 Mar 19
- ↑ van Dixhoorn J, Duivenvoorden HJ. Efficacy of Nijmegen Questionnaire in recognition of the hyperventilation syndrome. J Psychosom Res. 1985;29(2):199-206.
- ↑ 25.0 25.1 25.2 25.3 25.4 Chaitow, L. Dysfunctional Breathing Course Videos. Physioplus 2019. https://members.physio-pedia.com/2014/04/01/breathing-disorders/#resource
- ↑ Rosalba Courtney, Jan van Dixhoorn, Marc Cohen; Evaluation of Breathing Pattern: Comparison of a Manual Assessment of Respiratory Motion(MARM) and Respiratory Induction Plethysmography. Appl Psychophysiol Biofeedback (2008) 33:91–100
- ↑ Jade Shaw. Current clinical practices, experiences, and perspectives of healthcare practitioners who attend to dysfunctional breathing: A qualitative studyhttp://unitec.researchbank.ac.nz/bitstream/handle/10652/3589/MOst_Jade%20Shaw.pdf?sequence=1 (Accessed 16th September, 2017)
- ↑ Rosalba Courtney, Kenneth Mark Greenwood, Marc Cohen. Relationships between measures of dysfunctional breathing in a population with concerns about their breathing. Journal of Bodywork & Movement Therapies (2011) 15, 24-34
- ↑ http://www.svri.org/documents/health-and-well-being (Accessed 16th September, 2017)