Brachial Plexus Injury: Difference between revisions
No edit summary |
(pain management) |
||
| Line 223: | Line 223: | ||
The video clips below are examples of use of allografts and autografts. These complex procedures will need intensive physiotherapy after to resore the arm to the most optical outcome. | The video clips below are examples of use of allografts and autografts. These complex procedures will need intensive physiotherapy after to resore the arm to the most optical outcome. | ||
{{#ev:youtube|https://www.youtube.com/watch?v=6YzHsisOFtw|width}}<ref>Hand surgery internation 2015. BP surgery in 3 minutes. Available from: https://www.youtube.com/watch?v=6YzHsisOFtw (last accessed 11.4.2019)</ref> | {{#ev:youtube|https://www.youtube.com/watch?v=6YzHsisOFtw|width}}<ref>Hand surgery internation 2015. BP surgery in 3 minutes. Available from: https://www.youtube.com/watch?v=6YzHsisOFtw (last accessed 11.4.2019)</ref> | ||
{{#ev:youtube|https://www.youtube.com/watch?v=A8h3LgbVTMU|width}}<ref>Phoenics Children's Hospital. Dylan's story. Available from: https://www.youtube.com/watch?v=A8h3LgbVTMU (last accessed 11.4.2019)</ref> | {{#ev:youtube|https://www.youtube.com/watch?v=A8h3LgbVTMU|width}}<ref>Phoenics Children's Hospital. Dylan's story. Available from: https://www.youtube.com/watch?v=A8h3LgbVTMU (last accessed 11.4.2019)</ref> | ||
[[File:Fun fact.jpg|frameless|100x100px]] Funny Fact........What are | |||
==== Medical Management ==== | |||
Pain management is often diffucult. Significant pain occurs with root avulsions, causing neuropathic pain. Severe pain will also exhaust the client and if no treated will hinder the physiotherapy rehabilitation. This is when drugs should be used eg. NSAIDs and opioid drugs during the first stages (but with neuropathic chronic pain). Neuropathic pain requires careful use of anti epileptic drugs (gabapentin and carbamazepine) or antidepressants such as amitriptyline. Still however less than a third of clients reports significant pain relief with this approach.<ref name=":2">Sakellariou VI, Badilas NK, Stavropoulos NA, Mazis G, Kotoulas HK, Kyriakopoulos S, Tagkalegkas I, Sofianos IP. Treatment options for brachial plexus injuries. ISRN orthopedics. 2014 Apr 14;2014. (last accessed 12.3.2019)</ref> | |||
Physiotherapy may offer an additional source of pain relief with use of TENS, biofeedback, acupuncture and pain education. <ref name=":2" /> | |||
Dorsal Root Entry Zone (DREZ) operation is an option for persistant pain. The operation aims to destroy the nerve signal transmission from the secondary central sensory centrally. | |||
==== Phychological Management ==== | |||
* Psychological problems and a lack of cooperation by the patient may limit rehabilitation effects and increase disability.[[Brachial plexus|[8]]] | |||
* | |||
[[File:Fun fact.jpg|frameless|100x100px]] Funny Fact........What are armies for? To hang your handy's from! | |||
== Resources == | == Resources == | ||
Revision as of 07:36, 12 March 2019
Top Contributors - Aarti Sareen, Lucinda hampton, Kapil Narale, Garima Gedamkar, Kim Jackson, Vidya Acharya, Naomi O'Reilly, Mande Jooste, WikiSysop, Admin, Laura Ritchie, Meaghan Rieke, Wendy Walker and Evan Thomas
Introduction[edit | edit source]
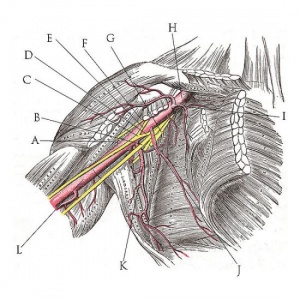
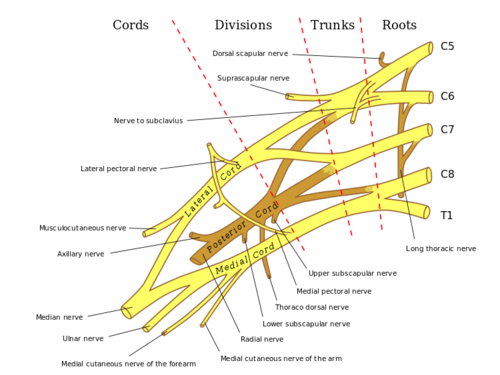
Brachial plexus is the network of nerves which runs through the cervical spine, neck, axilla and then into arm or it is a network of nerves passing through the cervico axillary canal to reach axilla and innervates brachium (upper arm), antebrachium (forearm) and hand.It is a somatic nerve plexus formed by intercommunications among the ventral rami (roots) of the lower 4 cervical nerves (C5-C8) and the first thoracic nerve (T1).
Function[edit | edit source]
The brachial plexus is responsible for cutaneous and muscular innervation of the entire upper limb, with two exceptions: the trapezius muscle innervated by the spinal accessory nerve (CN XI) and an area of skin near the axilla innervated by the intercostobrachial nerve.
Clinical Anatomy[edit | edit source]
The plexus consists of roots, trunks, divisions,cords and branches.
1. ROOTS: These are consititued by the anterior primary rami of spinal nerves C5,6,7,8 and T1 with contributions from the anterior primary rami of C4 and T2. The origin of the plexus may shift one segment either upward or downward resulting in a PRE FIXED PLEUS or POST FIXED PLEXUS respectively. In a prefixed plexus, the contribution by C4 is large and in that from T2 is often absent. In a post fixed plexus, the contribution by T1 is large, T2 is always present, C4 is absent, and C5 is reduced in size.[1] The roots join to form trunks as follows:
2.TRUNKS: Upper trunk is formed by C5 & C6
Middle trunk is formed by C7
Lower trunk is formed by C8 & T1
3. DIVISIONS OF THE TRUNKS: Each trunk divides into ventral and dorsal divisions (which ultimately supply the anterior and posterior aspects of the limb). These divisions join to form cords.
4. CORDS: it forms 3 cords
- The Posterior Cord is formed from the three posterior divisions of the trunks (C5-C8,T1)
- The Lateral Cord is the anterior divisions from the upper and middle trunks (C5-C7)
- The Medial Cord is simply a continuation of the anterior division of the lower trunk (C8,T1)
5. BRANCHES: The specific branches of each cord can be seen at this page
Mechanism of injury[edit | edit source]
Injury to brachial plexus can occur in many ways. These include the contact sports, road traffic accident, motorvehicle accident or during birth. Grossly, it can be divided into
- Traumatic e.g motor vehicle accident, contact sports
- Non traumatic e.g.obstetric palsy and Parsonage-Turner Syndrome
The network of nerves is fragile and can be damaged by pressure, stretching, or cutting. Stretching can occur when the head and neck are forced away from the shoulder, such as might happen in a fall from a motorcycle. If severe enough, the nerves can actually avulse, or tear out of their roots in the neck. Pressure could occur from crushing of the brachial plexus between the collarbone and first rib, or swelling in this area from injured muscles or other structures[2]. The former examples of events are caused by one of two mechanisms that remain constant during the injury.[3]. The two mechanisms that can occur are traction and heavy impact[4]. These two methods disturb the nerves of the brachial plexus and cause the injury[5].
TRACTION: Traction, also known as stretch injury, is one of the mechanisms that cause brachial plexus injury. The nerves of the brachial plexus are damaged due to the forced pull by the widening of the shoulder and neck.Traction occurs from severe movement and causes a pull or tension among the nerves. There are two types of traction: downward traction and upward traction. In downward traction there is tension of the arm which forces the angle of the neck and shoulder to become broader. This tension is forced and can cause lesions of the upper roots and trunk of the nerves of the brachial plexus. Upward traction also results in the broadening of the neck and shoulder angle but this time the nerves of T1 and C8 are torn away.[6]
IMPACT: Heavy impact to the shoulder is the second common mechanism to causing injury to the brachial plexus. Depending on the severity of the impact, lesions can occur at all nerves in the brachial plexus. The location of impact also affects the severity of the injury and depending on the location the nerves of the brachial plexus may be ruptured or avulsed. Some forms of impact that affect the injury to the brachial plexus are shoulder dislocation, clavicle fractures, hyperextension of the arm and sometimes delivery at birth.[7] During the delivery of a baby, the shoulder of the baby may graze against the pelvic bone of the mother. During this process, the brachial plexus can receive damage resulting in injury.This is very low compared to the other identified brachial plexus injuries.[8]
Classification of injuries[edit | edit source]
The various classifications of brachial plexus injury are as follows:
- Leffert classification of brachial plexus injury
- Millesi classification of brachial plexus injury
- Classification on anatomical location of injury
1. Leffert classification of brachial plexus injury[9]: It is based on etiology and level of injury and is as follows
- I Open (usually from stabbing)
- II Closed (usually from motorcycle accident)
- IIa Supraclavicular
- preganglionic:
- avulsion of nerve roots, usually from high speed injuries with other injuries and LOC;
- no proximal stump, no neuroma formation (neg Tinel's)
- pseudomeningocele, denervation of neck muscles are common
- horner's sign (ptosis, miosis, anhydrosis)
- postgangionic:
- roots remain intact;
- usually from traction injuries;
- there are proximal stump and neuroma formation (pos Tinel's)
- deep dorsal neck muscles are intact, and pseudomeningoceles will not develop;
- Infraclavicular Lesion:
- usually involves branches from the trunks (supraclavicular);
- function is affected based on trunk involved;
- preganglionic:
- III Radiation induced
- IV Obstetric
- IVa Erb's (upper root) - waiter's tip hand;
- IVb Klumpke (lower root)
2. Millesi classification of brachial plexus injury[10]: It is mainly divided into 4
I: supraganglionic/preganglionic.
II: infraganglionic/postganglionic
III: trunk.
IV: cord.
3. Classification on anatomical location of injury[11][12]:
- Upper plexus palsy (Erb’s palsy in the OBPI cases) involves C5-C6+/-C7roots.
- Lower plexus palsy (Klumpke’s palsy) involves C8-T1 roots (and sometimes also C7)
- Total plexus lesions involve all nerve roots C5-T1
- Some authors have included a fourth type,an intermediate type that primarily involves the C7 root.[13][14]
Injuries[edit | edit source]
Injuries to roots, trunks and cords of the brachial plexus produce characteristic defects which are as follow[1]
ERB'S PARALYSIS:[edit | edit source]
Site of injury: The region of the upper trunk of the brachial plexus is called Erb's point. Six nerves meet here. Injury to the upper trunk causes Erb's Paralysis.
Causes of injury: Undue separation of the head from the shoulder, which is commanly encountered in 1)birth injury 2) fall on shoulder, and 3)during anaesthesia
Nerve roots involved: Mainly C5 and partly C6.
Muscles paralysed: Mainly biceps, deltoid,brachilais and brachioradialis.Partly supraspinatus, infraspinatus and supinator
Deformity
Arm: Hangs by the side, it is adducted and medially rotated
Forearm: Extended and pronated
The deformity is known as "Policeman's tip hand" or "Porter's tip hand".
Disability:
- Abduction and lateral rotation of the arm (shoulder).
- Flexion and supination of forearm.
- Biceps and supinator jerks are lost.
- Sensations are lost over a small area over the lower part of the deltoid.
For more information on Erb's paralysis see this page
KLUMPKE'S PARALYSIS:[edit | edit source]
Site of injury: Lower trunk of the brachial plexus.
Cause of injury: Undue abduction of the arm, as in clutching something with the hand after a fall from a height, or sometimes in birth injury.
Nerve roots involved: Mainly T1 and partly C8.
Muscles paralysed:
- Intrinsic muscles of the hand (T1)
- Ulnar flexors of the wrist and fingers (C8).
Deformity: (position of the hand): claw hand due to the unopposed action of the long flexors and extensors of the fingers. in a claw hand there is hyperextension at the metacarphalangeal joints and flexion at the interphalangeal joints.
Disability:
- Claw hand
- Cutaneous anaesthesia and analgesia in a narrow zone along the ulnar border of the forearm and hand.
- Horner's syndrome: ptosis, miosis, anhydrosis, enophthalmos and loss of ciliospinal reflex- may be associated. This is because of injury to sympathetic fibres to the head and neck that leave the spinal cord through nerve T1.
- Vasomotor changes: The skin areas with sensory loss is warner due to arteriolar dilation. it is also drier due to the absence of sweating as there is loss of sympathetic activity.
- Tropic changes: Long standing case of paralysis leads to dry and scaly skin.The nails crack easily with atrophy of the pulp of fingers.
For more information on Klupmke's paralysis see this pgae
INJURY TO LATERAL CORD:[edit | edit source]
Cause: Dislocation of humerus associated with others
Nerve involved: musculocutaneous, lateral root of median.
Muscles paralysed:
- Biceps and coracobrachialis
- All muscles supplied by the median nerve,except those of hand.
Deformity and disability:
- Midprone forearm
- Loss of flexion of forearm
- Loss of flexion of the wrist
- Sensory loss on the radial side of the forearm
- Vasomotor and trophic changes.
INJURY TO MEDIAL CORD:[edit | edit source]
Cause: Subcoracoid dislocation of humerus
Nerves involved: Ulnar, Medial root of median
Muscles paralysed:
- Muscles supplied bye ulnar nerve
- Five muscles of the hand supplied bye the median nerve.
Deformity and disability
- Claw hand
- Sensory loss on the ulnar side of the forearm and hand
- Vasomotor and tropic changes as a bone.
Physiotherapy treatment [edit | edit source]
[edit | edit source]
Physiotherapy treatment for BP injury varies significantly according to the type and severity of the injury. In mild cases physiotherapy and rehabilitation will assist recovery, in more severe cases surgery and bracing may be needed.[16] Always the goal stays constant ie to return to previous level of function and preventing potential disability.
Physiotherapists treatment is aimed at
- Development of strength, flexibility, stamina and co-ordination
- Maintaining ROM via passive movements, exercise therapy, splinting and positioning and protection of denervated dermatomes.[17]
- Functional training and adoption adaptive devices if needed.[18]
- Pain control via acupuncture and TENS
- Managing chronic oedema via education, compression garments and massage therapy.[17]
The video clips below highlight the scope of treatment that may be undertaken due to the variance of injuries.
The following video shows treatment methods that may be employed after a Vespa scooter accident.
The next video is a treatment approach for an infant with a traction injury to the brachial plexus.
The next video shows treatment that may occur following a simple over stretching of the brachial plexus.
The next video is demonstrating BP neuromobility stretches could be used in the rehabilitation of eg sporting BP injuries. Neuromobilty places an important role in eliminating pain and restoring function.
Physiotherapy following surgery for Brachial Plexus injury[edit | edit source]
Surgery is an option for severe brachial plexus injuries, and to be viable should occur within certain timeframes. Surgery aims to regain function by surgical repair. This can take the from of nerve grafts, nerve transfers or both, and possible musculoskeletal reconstructions.[18]
Physiotherapists are crucial in the rehabilitive phase post surgery in the resoring of function via strength, co-ordination, flexibility, ROM, power and use of splinting if needed. The client needs to be aware that the rehabilitation phase will be year(s) not weeks.[18]
The video clips below are examples of use of allografts and autografts. These complex procedures will need intensive physiotherapy after to resore the arm to the most optical outcome.
Medical Management[edit | edit source]
Pain management is often diffucult. Significant pain occurs with root avulsions, causing neuropathic pain. Severe pain will also exhaust the client and if no treated will hinder the physiotherapy rehabilitation. This is when drugs should be used eg. NSAIDs and opioid drugs during the first stages (but with neuropathic chronic pain). Neuropathic pain requires careful use of anti epileptic drugs (gabapentin and carbamazepine) or antidepressants such as amitriptyline. Still however less than a third of clients reports significant pain relief with this approach.[25]
Physiotherapy may offer an additional source of pain relief with use of TENS, biofeedback, acupuncture and pain education. [25]
Dorsal Root Entry Zone (DREZ) operation is an option for persistant pain. The operation aims to destroy the nerve signal transmission from the secondary central sensory centrally.
Phychological Management[edit | edit source]
- Psychological problems and a lack of cooperation by the patient may limit rehabilitation effects and increase disability.[8]
 Funny Fact........What are armies for? To hang your handy's from!
Funny Fact........What are armies for? To hang your handy's from!
Resources[edit | edit source]
http://brachialplexussurgery.com/
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ 1.0 1.1 B.D Chaurasia.Human Anatomy.Vol.1.Fourth Edition.
- ↑ American Society of Surgery of Hand. Available from www.assh.org/Public/HandConditions/Documents/Web_Version_PDF/BrachPlex.pdf
- ↑ Midha, Rajiv, MD. "Neurosurgery." Epidemiology of Brachial Plexus Injuries in a Multitrauma Po... :. Congress of Neurological Surgeons, June 1997. Web. 29 Jan. 2013.
- ↑ Narakas, A.O. "The Treatment of Brachial Plexus Injuries." Link.springer.com. International Orthopaedics, June 1985. Web. 28 Jan. 2013.
- ↑ Hems, TE.; Mahmood, F. (Jun 2012). "Injuries of the terminal branches of the infraclavicular brachial plexus: patterns of injury, management and outcome.". J Bone Joint Surg Br 94 (6): 799–804.
- ↑ Coene, L.N.J.E.M. "Mechanisms of Brachial Plexus Lesions." ScienceDirect.com. Clinical Neurology and Neurosurgery, 25 Mar. 2003. Web. 29 Jan. 2013.
- ↑ Jeyaseelan, L.; Singh, VK.; Ghosh, S.; Sinisi, M.; Fox, M. (Jan 2013). "Iatropathic brachial plexus injury: A complication of delayed fixation of clavicle fractures.". Bone Joint J 95–B (1): 106–10.
- ↑ Joyner, Benny, Mary Ann Soto, and Henry M. Adam. "Brachial Plexus Injury." Brachial Plexus Injury. Pediatrics in Review, 1 June 2006. Web. 29 Jan. 2013.
- ↑ Clifford R. Wheeless.Wheeless' Textbook of Orthopaedics.Duke's Orthopaedics.
- ↑ Andrew Hodges.A-Z of Plastic Surgery.Oxford University Press.
- ↑ Dodds SD et al.Perinatal Brachial Plexus Palsy. Curr Op Pediat 12: 40-47, 2000.
- ↑ Kay SPJ. Obstetrical Brachial Palsy. Br J Plastic Surg 51: 43-50, 1998.
- ↑ Al-qattan MM. Self-mutilation in Children with Obstetric Brachial Pexus Palsy. J Hand Surg Br 24B; 5: 547-549, 1999
- ↑ Shenaq SM et al. Brachial Plexus Birth Injuries and Current Management. Clin Plast Surg 25; 4: 527-536, 1998
- ↑ Hospital for special surgery. What is a brachial plexus injury. Available from: https://www.youtube.com/watch?v=BnAJNnhC5EY (last accessed 10.3.2019)
- ↑ Richmond Rehab. The Brachial plexus. Available from: https://www.richmondrehab.com.au/blog/category/the-brachial-plexus (last accessed 10.3.2019)
- ↑ 17.0 17.1 Sakellariou VI, Badilas NK, Stavropoulos NA, Mazis G, Kotoulas HK, Kyriakopoulos S, et al. Treatment options for brachial plexus injuries. ISRN Orthop. 2014:314137. doi: 10.1155/2014/314137. Available from: Sakellariou VI, Badilas NK, Stavropoulos NA, Mazis G, Kotoulas HK, Kyriakopoulos S, et al. Treatment options for brachial plexus injuries. ISRN Orthop. 2014:314137. doi: 10.1155/2014/314137.(last accessed 11.3.2019)
- ↑ 18.0 18.1 18.2 Ausmed. Brachial Plexus Injuries. Available at: https://www.ausmed.com/cpd/articles/brachial-plexus-injuries (last accessed 10.3.2019)
- ↑ Mayo clinic. Treatment of Brachial plexus injuries. Available from: https://www.youtube.com/watch?v=KwgHgg3Vfx4 (last accessed 10.3.2019)
- ↑ rAnn and Robert H. Lurie. Childrens hospital of Chicago. Available from: https://www.youtube.com/watch?v=bvKrUEehkKc (last accessed 10.3.2019)
- ↑ Ask Dr Jo. Bracial plexus injury stretches and exercise. Available from: https://www.youtube.com/watch?v=oVWfYUk4vOA (last accessed 10.3.2019)
- ↑ COR. Brachial plexus neuromobility. Available from: https://www.youtube.com/watch?v=F3tKQG8IUrI (last accessed 10.3.2019)
- ↑ Hand surgery internation 2015. BP surgery in 3 minutes. Available from: https://www.youtube.com/watch?v=6YzHsisOFtw (last accessed 11.4.2019)
- ↑ Phoenics Children's Hospital. Dylan's story. Available from: https://www.youtube.com/watch?v=A8h3LgbVTMU (last accessed 11.4.2019)
- ↑ 25.0 25.1 Sakellariou VI, Badilas NK, Stavropoulos NA, Mazis G, Kotoulas HK, Kyriakopoulos S, Tagkalegkas I, Sofianos IP. Treatment options for brachial plexus injuries. ISRN orthopedics. 2014 Apr 14;2014. (last accessed 12.3.2019)