Meniscal Repair
Original Editor - Rachael Lowe, Jennifer Uytterhaegen
Top Contributors - Rachael Lowe, Laura Ritchie, Admin, Van Horebeek Erika, Scott Cornish, Kim Jackson, David Bayard, Lauren Heydenrych, Yannick Goubert, Evan Thomas, 127.0.0.1, Wendy Walker, George Prudden, Wanda van Niekerk and Mahbubur Rahman David Bayard, Neil De Heyder, Jack Cortvriend, Nicolas Casier
Definition/Description[edit | edit source]
An arthroscopic meniscectomy is a procedure to remove some or all of a meniscus from the tibio-femoral joint of the knee using arthroscopic (aka 'keyhole') surgery. In a complete meniscectomy the meniscus including the meniscal rim is removed. A partial meniscectomy involves partial removal of the meniscus. This may vary from minor trimming of a frayed edge to anything short of removing the rim. This is a minimally invasive procedure often done as day suas an outpatient in a one-day clinic [1] This procedure is performed when a meniscal tear is too large to be corrected by a surgical meniscal repair.[1] When non-operative therapy provides some degree of symptom relief over the long-term, these benefits may wane with continued meniscal degeneration. In such patients, arthroscopic partial meniscectomy can be effective in improving patient quality of life.
Clinically Relevant Anatomy[edit | edit source]
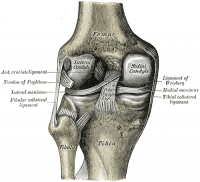
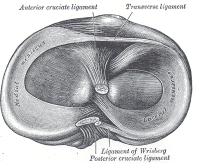
The menisci of the knee are crescent-shaped fibrocartilaginous structures which add to the tibio-femoral joint congruency while also dispersing friction and body weight. A difference exists between the medial and the lateral meniscus: [1]
- The medial meniscus is larger than the lateral meniscus and has a C shape. It blends with the medial collateral ligament [2]
- The lateral meniscus is smaller than the medial meniscus and has an O-shape. This is more mobile than the medial meniscus and blends with the popliteus muscle. [2]
Epidemiology/ Etiology[edit | edit source]
As reported by Majewski, injuries to the menisci are the second most common injury to the knee, with an incidence of 12% to 14% and a prevalence of 61 cases per 100,000 persons[27][32][33]. In his epidemiological study conducted on 17,397 patients in Germany and Switzerland, soccer, followed by skiing, are the sport with an increased risk of meniscal injuries. Among the injuries affecting the knee, he shows that most involve anterior cruciate ligament (ACL) (20.34%), medial meniscus (10.76%) and lateral meniscus (3.66%). He also observes that 85% of patients with meniscal and ACL injuries require arthroscopic treatment [28].
Etiology
For degenerative meniscal tears, this literature review provides strong evidence that age (greater than 60 years), gender (being male), work-related kneeling and squatting, and climbing stairs (greater than 30 flights) are risk factors for meniscal tears. Also, there was strong evidence that sitting greater than 2 hours per day may reduce the risk of degenerative meniscal tears. For acute meniscal tears, there was strong evidence that playing soccer and playing rugby are risk factors[34]. There was also strong evidence that waiting more than 12 months between ACL injury and reconstruction surgery is a risk factor for a tear of the medial meniscus [30] [35].
Clinical Presentation[edit | edit source]
- joint line tenderness and effusion
- symptoms are frequently worsened by flexing and loading the knee, activities such as squatting and kneeling are poorly tolerated
- complaints of 'clicking', 'locking' and 'giving way' are common
- functionally unstable knee [1]
- symptoms are frequently worsened by flexing and loading the knee, activities such as squatting and kneeling are poorly tolerated because of stiffness and pain [3]
Differential Diagnosis[edit | edit source]
Joint line tenderness and effusion. However the joint line tenderness test may be false positive with osteoarthritis, osteochondral defects, collateral ligament injury or fractures. [31]
Effusion may also occur when there are problems with the cruciate ligaments, bones or the articular cartilage.
Symptoms are frequently worsened by flexing and loading the knee, activities such as squatting and kneeling are poorly tolerated. But it’s the same with patients suffering from other pathologies like chondromalacia patellae, fractures and Sinding Larsen Johansson Syndrome.
Complaints of 'clicking', 'locking' and 'giving way' are common. Patients also complain about ‘giving’ way when there are suffering from anterior cruciate ligament injury. The feeling of instability and locking is also common with osteochondritis dessecans.
Diagnostic Procedures[edit | edit source]
1. Joint line tenderness has been reported to be the best common test for meniscal injury [1]
2. McMurray's test positive if a pop or a snap at the joint line occurs while flexing and rotating the patient's knee.
3. Apley's test performed with the patient prone, and with the examiner hyperflexing the knee and rotating the tibial plateau on the femoral condyles.
4. Steinman's test performed on a supine patient by bringing the knee into flexion and rotating.
5. Ege's Test is performed with the patient squatting, an audible and palpable click is heard/felt over the area of the meniscus tear. The patient's feet are turned outwards to detect a medial meniscus tear, and turned inwards to detect a lateral meniscus tear.
6. Thessaly Test : Clinical screening tool for meniscal tears. For more information check this physiopedia page: http://www.physio-pedia.com/Thessaly_test
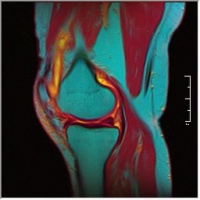
7. MRI: The demonstration of meniscal lesions by MRI has a crucial role in patients with combined injuries as the menisci. The main challenge for MRI is the assessment of the meniscal surfaces. MRI signs of abnormal findings include: [4]
- Grade I: Discrete central degeneration - an intrameniscal lesion of increased signal without connection to articular surface [4]
- Grade II: Extensive central degeneration - a larger intrameniscal area of increased signal intensity, again without connection to articular surface. May be horizontal or linear in orientation [4]
- Grade III: Meniscal tear - increased intrameniscal signal intensity with contour disruption of articular surface. May be associated with displacement of meniscal fragments or superficial step formation [4]
- Grade IV: Complex meniscal tear - multiple disruption of meniscal surfaces
- The presence of tears in the red versus white zones of the meniscus is important since reattachment of meniscal fragments is promising only in the vascularized zone. [4]
| [5] | [6] |
Video: http://www.youtube.com/watch?v=31mbTI4CsUI
http://www.youtube.com/watch?v=BVXDEAYPYCg
File:Knee MRI.jpg T1 Weighted MRI |
Outcome measures[edit | edit source]
WOMET – Western Ontario Meniscal Evaluation Tool
NRS – Numeric Rating Scale for pain
VAS pain – Visual Analogue Scale for pain
KOS – Knee outcome survey
KOOS – Knee injury and osteoarthritis outcome score
IKDC – Internation Knee Documentation Committee[23]
Tegner score
Lysholmscore [29]
Examination[edit | edit source]
Add text here
Medical Management[edit | edit source]
No matter what type of meniscal tear is present the physician will work with the patient to determine what the best course of treatment will be.
Small, degenerative meniscal tears are often treated conservatively with rest, anti-inflammatory measures, activity modification and Physical Therapy. Many times when the inflammation is resolved and the patient is agreeable to reducing the load bearing activity affecting the joint, surgery can be avoided. If a non-surgical approach is taken the patient must understand that it is imperative that he or she maintain good strength in his or her leg and avoid sports or activities that require pivoting or cutting.
If the tear is large or if conservative measures fail to alleviate the associated pain and joint dysfunction than the surgeon may elect to remove the tear surgically with the use of an arthroscope. [18 (2a)]
Indication for surgery
The decision whether a lesion is treated surgically or non-surgically is the first decision made after definitively diagnosing a meniscal tear. This decision is based on patient’s factors (e.g. age, co-morbidities and compliance), tear characteristics (e.g. location of the tear, age of the tear and pattern of the tear) and the fact whether the tear is stable or unstable. When the tear is unstable surgery is necessary. [9(2b)][10(2b)]
A degenerative tear or a non-degenerative tear which is asymptomatic or stable is treated non-surgically. In the other cases, such as non-degenerative tears or tears which are symptomatic the tears are treated surgically. [11(5)]
The second decision concerns whether meniscal repair or meniscectomy is appropriate. If none of the normal surgical treatments seems appropriate total meniscectomy is the last option. The factors that should have been taken in consideration while making decisions should be: 1) the clinical evaluation, 2) related lesions and 3) the exact type, location, and extent of the meniscal tear. [12(2b)]
If meniscal repair is performed combined with an ACL reconstruction the success rate is influenced. Whether the influence is positive or negative is studied in several studies with different conclusions. [13(2b)] [14(3b)] [15(4)] [16(4)]
Tenuta JJ et al. also found that width of the lesion is an important factor no lesion with a width of more than 4 mm healed. [13(2b)]
Surgery
When the meniscal tear is removed the surgeon uses an arthroscopic technique. Two small incisions are made in the front part of the knee below the knee cap. Through one incision a camera is inserted so that the surgeon can see the inside of the knee joint on a monitor. The other incision is used to place a tool into the joint that will clip and remove the torn piece of cartilage. While the camera is inside the joint the surgeon uses this opportunity to examine the rest of the knee to make sure it is otherwise healthy.
Physical Therapy Management[edit | edit source]
Pre-Operative[edit | edit source]
Neuromuscular electrical stimulation (NMES) causes muscle contraction by applying transcutaneous current to terminal branches of the motoneuron. In subjects with knee osteoarthritis, NMES can increase quadriceps strength and improve functional performance, and has been found to be as effective as exercise therapy. NMES has also a beneficial effect on muscle mass. Other benefits of the therapy a a reduction in postoperative muscle atrophy with exercise prehabilitation.[19(3b)]
Pre-operative risk factors
Meniscectomy is a safe procedure in older patients, as age over 65 years did not increase the odds of any of the adverse events studied. However, regardless of age, patients with an increased comorbidity burden and those with a history of smoking are at increased risk of adverse events and/or readmission after the procedure. [6]
Post-Operative[edit | edit source]
After meniscectomy rehabilitation protocol can be aggressive, because in the knee joint anatomical structure should not be protected during the healing phase.
The rehabilitative treatment consists of ice-ultrasound therapy, friction massage, joint mobilization, calf raises, steps-ups, extensor exercise and bicycle ergometry[20(5)] . Exercise on a bicycle ergometer equipped with an adjustable pedal arm demonstrated promising results in patients after partial meniscectomy. [21(3B)] Treatment under water cannot begin until wounds have properly closed in order to prevent increased risk of infection.
In the first week after surgery rehabilitation treatment consists of a progressive loading with crutches. Early objectives after surgery are: control of pain and swelling, maximum knee range of motion (ROM) and a full load walking. There is no load limitation, compatibly with the tolerance of the patient is needed.
In the subsequent 3 weeks the goal is to obtain a normal pace, increasing the knee ROM, depending on the patient’s tolerability.
Intensive muscle strengthening, proprioceptive and balance exercises are carried out by the third week.
The resumption of sport training is allowed when quadriceps’ muscle strength is at least 80% in the operated limb compared to the contralateral limb, while the patient may return to competitions when the quadriceps muscle strength in the operated limb is at least 90% than healthy limb.
Generally, patients return to work after 1 or 2 weeks, to sporting activities after 3 to 6 weeks and to competitions after 5 or 8 weeks, in a sportsman, rehabilitation plays a key role in restoring as soon as possible quadriceps normal strength in both legs before returning to competitions. [20(5)]
The rehabilitation can be split up in 3 phases:
(The patient should perform at least 8 exercises, 12-15 repetitions, 1-2 sets of the following types of exercises)[24(2b)][26(2b)]
• Phase 1: The Acute Phase (1-10 days post-op)
In the first phase, the goals are to decrease inflammation, restore the range of motion and the neuromuscular re-education of quadriceps. Inflammation can be decreased with massages, cryotherapy and electro-stimulation (NMES or IFC). Exercises in the first phase of rehabilitation are: quad Sets Long arc quad, short arc quad, hamstring curls (open chain exercises) and bicycle training, leg presses etc. (Closed chain exercises).
• Phase 2: The Subacute Phase (10 days-4 weeks post-op)
Goals are to restore muscle strength and endurance, re-establish full and pain free ROM, gradual return to functional activities and to minimize gait deviations. More concentric/eccentric exercises for the hip and the knee should be added to the open chain exercises from phase 1. Closed chain exercises in the second phase should be resisted terminal knee extension, partial squats (not complete), step up/down progressions, toe raises, functional and agility training.
• Phase 3: The Advanced Activity Phase (4-7 weeks post-op)
The goals of the third and last phase are to enhance muscle strength and endurance, maintain full ROM and to return to sports or functional activities. Progression to dynamic single leg stance, plyometrics, running, and sport specificity training should be apprehended in this phase [24(2b)] [25(4)] [26(2b)]
The goal of rehabilitation is to restore patient function based on individual needs. It is important to consider:
- the type of surgical procedure
- the post-surgical protocol determined by the surgeon [7]
- which meniscus was repaired
- the type of meniscal tear
- preoperative knee status (including time between injury and surgery)
- decreased range of motion or strength
- the patient's age
- the presence of coexisting knee pathology (particularly ligamentous laxity or articular cartilage degeneration)
- the patient's functional and/or athletic expectations and motivations
Rehabilitation Overview[edit | edit source]
- Control the pain, swelling and inflammation by using: cryotherapy, analgaesics, NSAIDs. [4]
- As rehabilitation progresses, continued use of modalities may be required to control residual pain and swelling. [8]
- Restore range of motion using exercises within the limits that the surgeon has specified [4]
- If a meniscal repair has been performed, extreme flexion and rotation should be limited until the wound in the meniscus has had time to heal (8 to 12 weeks).
- Restore muscle function using specific strengthening exercises including quadriceps, hamstrings, hip. Examples: [4][2]
- for quadriceps: squads, knee extensions
- for hamstrings: leg curl with resistance (eg resistance band)
- for hip: bridging, straight leg raise
- Strengthening around the knee is crucial but it may also be necessary to strengthen the adjacent joints if weight-bearing was restricted pre- or post-operatively.
- While strong muscles around the joint are critical, flexibility exercises of the same muscle groups must be considered and should be included throughout the period of strengthening.
- Optimize neuromuscular coordination and proprioceptive re-education. [4]
- The patient, physical therapist and surgeon will determine the extent of these exercises. [8]
- Progress weight-bearing: weight-bearing and joint stress are necessary to enhance the functionality of the meniscal repair and should be progressed as indicated by the surgeon.[4]
Additional Considerations[edit | edit source]
| [9] |
- Full weight bearing or bearing weight as tolerated immediately after the meniscectomy
- Passive and active range-of-motion exercises begin immediately postoperatively and quadriceps strengthening exercises
- Crutches are usually required for 2-5 days until the patient is able to fully put his/her body weight on the knee without significant discomfort
- Return to full daily activities usually at 4-6 weeks, providing full range of motion has been regained
- Athletes may return to full athletic activities when normal quadriceps muscle tone has recovered and range of motion is full and pain-free
- EMG-B (electromyography-biofeedback) is an effective treatment in improving quadriceps muscle strength after arthroscopic meniscectomy surgery [2]
Key Evidence[edit | edit source]
Raine Sivhonen et al., ‘a protocol for a randomised, placebo surgery controlled trial on the efficacy of arthroscopic partial meniscectomy for patients with degenerative meniscus injury with a novel ‘RCT within-a-cohort’ study design.’, CMAJ, 2014 Oct 7; 186(14): 1057–1064.
Resources[edit | edit source]
Brindle T, Nyland J, Johnson DL. The meniscus: review of basic principles with application to surgery and rehabilitation. J Athl Train. 2001;36(2):160-169.
Clinical Bottom Line[edit | edit source]
add text here
References[edit | edit source]
1 ↑ 1.0 1.1 1.2 1.3 Meserve BB, Cleland JA, Boucher TR. A meta-analysis examining clinical test utilities for assessing meniscal injury. Clin Rehabil. 2008;22(2):143-161.
2 ↑ 2.0 2.1 McKeon B, Bono J, Richmond J, editors. Knee arthroscopy. London:Springer, 2009.
3 ↑ 3.0 3.1 3.2 3.3 Atkinson HDE, Laver JM, Sharp E. Physiotherapy and rehabilitation following soft tissue surgery of the knee. Orthop Trauma. 2010;24(2):129-138.
4 ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 4.9 Teller P, Konig H, Weber U, Hertel P. MRI atlas of orthopedics and traumatology of the knee. London:Springer, 2003.
5 ↑ CRTechnologies. Steinman I Sign Test (CR). Available from: http://www.youtube.com/watch?v=31mbTI4CsUI[last accessed 15/12/12]
6 ↑ CRTechnologies. Ege's Test (CR). Available from: http://www.youtube.com/watch?v=BVXDEAYPYCg[last accessed 15/12/12]
7 ↑ Kohn D, Aagaard H, Verdonk R, Dienst M, Seil R. Postoperative follow-up and rehabilitation after meniscus replacement. Scand J Med Sci Sports. 1999;9(3):177-80.fckLR
8 ↑ 8.0 8.1 Thomson LC, Handoll HH, Cunningham A, Shaw PC. Physiotherapist-led programmes and interventions for rehabilitation of anterior cruciate ligament, medial collateral ligament and meniscal injuries of the knee in adults. Cochrane Database Syst Rev. 2002;(2):CD001354.
9 ↑ MegaElectronicsLtd. Biofeedback rehabilitation after ACL reconstruction (eMotion Biofeedback). Available from: http://www.youtube.com/watch?v=MQYo8B8wKWc[last accessed 15/12/12]
9 ↑ El Ghazaly SA, Rahman AA, Yusry AH, Fathalla MM., Arthroscopic partial meniscectomy is superior to physical rehabilitation in the management of symptomatic unstable meniscal tears. Int Orthop, October 2014.
10 ↑ 9.0 9.1 Simon C et al. Treatment of meniscal tears: An evidence based approach. World Journal of Orthopedics. Juli 2014. 5(3): 233-241 Level of evidence: 2b
11 ↑ DeHaven Ke. Decision-making factors in the treatment of meniscus lesions. Clinical Orthopedics & Related Research 1990; (252) 49-54. Level of evidence: 5 (abstract)
12 ↑ Jensen NC, Riis J, Robersten K, et al. Arthroscopic repair of the ruptured meniscus: one to 6.3 years follow up. Arthroscopy 1994; 10 (2): 211-214. Level of evidence: 2b
13 ↑ 12.0 12.1 Tenuta JJ, Arciera RA. Arthroscopic evaluation of meniscal repairs. Factors that effect healing. Am J Sports Med 1994; 22 (6): 797-802. Level of evidence: 2b
14 ↑ Cannon WD, Jr., Vittori JM. The incidence of healing in arthroscopic meniscal repairs in anterior cruciate ligament-reconstructed knees versus stable knees. Am J Sports Med 1992; 20 (2) 176-181.
15 ↑ 14.0 14.1 Walter RP, Dhadwal AS, Schranz P, Mandalia V. The outcome of all-inside meniscal repair with relation to previous anterior cruciate ligament reconstruction. Elsevier 2014;
16 ↑ Konan S, Rayan F, Haddad FS., Do physical diagnostic tests accurately detect meniscal tears?, Knee Surg Sports Traumatol Arthosco, July 2009. Level of evidence: 4
17 Lim HC, Bae JH, Wang JH, Seok CW, Kim MK. Non-operative treatment of degenerative posterior root tear of the medial meniscus. Knee Surg Sports Traumatol Arthrosc. 2010;18:535–539. [PubMed]
18 Messner K, Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat 1998PubMed]
19 Raymond J wall et al.” Effects of preoperative neuromuscular electrical stimulation on quadriceps strength and functional recovery in total knee arthroplasty. A pilot study” BMC Musculoskeletal Disorders2010. Level of evidence: 3
20 Antonio Frizzereiro et al.’The meniscus tear: state of art of rehabilitation protocols related to surgical procedurs’. Muscles Ligament Tendon Journal. 2012 Oct-Dec.
21 Moffet H, et al. Impact of knee extensor strength deficits on stair ascent performance in patients after medial meniscectomy. Scand J Rehabil Med. 1993 Level of evidence: 3
22 Bryce A. Basques et al. ‘Risk Factors for Short-term Adverse Events and Readmission After Arthroscopic Meniscectomy’ Am J Sports Med January 2015 vol. 43 no. 1 169-175. Level of evidence: 3
23 Physiopedia, ‘Meniscal rupture’
24 Herrlin S et al., Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc. 2007 April.
Level of evidence: 2b
25 Fransen M et al., Exercise for osteoarthritis of the knee., Cochrane Database Syst Rev. 2015 Jan 9
Level of evidence: 4
26 Alexandra Kirkley, M.D. et al., A randomized trial of arthroscopic surgery for osteoarthritis of the knee. The new England journal of medicine. Level of evidence :2b
27 Logerstedt DS, et al. Knee pain and mobility impairments: meniscal and articular cartilage lesions. J Orthop Sports Phys Ther. 2010;40(9):597 Level of evidence: 5
28 Majewski M, Habelt S, Klaus Steinbruck. Epidemiology of athletic knee injuries: A 10-year study. Knee. 2006;13(3):184–188. Epub 2006 Apr 17 Level of evidence:3
29 Reliability, validity, and responsiveness of the Lysholm knee score and Tegner activity scale for patients with meniscal injury of the knee. Briggs KK1, Kocher MS, Rodkey WG, Steadman JR.2006
Level of evidence:3
30 BARBARA A.M. SNOEKER, MSc1 • ERIC W.P. BAKKER, PhD1 • CORNELIA A.T. KEGEL, PhD2 • CEES LUCAS, PhD1 Risk Factors for Meniscal Tears: A Systematic Review Including Meta-analysis.
Level of evidence: 1
31: Konan S, Rayan F, Haddad FS., Do physical diagnostic tests accurately detect meniscal tears?, Knee Surg Sports Traumatol Arthosco, July 2009. Level of evidence: 4
32 Baker BE, Peckham AC, Pupparo F, Sanborn JC. Review of meniscal injury and associated sports. Am J Sports Med. Level of evidence: 3a
33 Hede A, Jensen DB, Blyme P, Sonne-Holm S. Epidemiology of meniscal lesions in the knee. 1,215 open operations in Copenhagen 1982-84. Acta Orthop Scand. 1990. Level of evidence: 3a
34 Meniscal tear as an osteoarthritis risk factor in a largely non-osteoarthritic cohort: a cross-sectional study.Ding C1, Martel-Pelletier J, Pelletier JP, Abram F, Raynauld JP, Cicuttini F, Jones G.Level of evidence :3b
35 Reconstruction of the anterior cruciate ligament: timing of surgery and the incidence of meniscal tears and degenerative change. Church S1, Keating JF. Level of evidence: 3b
- ↑ 1.0 1.1 McKeon B, Bono J, Richmond J, editors. Knee arthroscopy. London:Springer, 2009.
- ↑ 2.0 2.1 2.2 2.3 Atkinson HDE, Laver JM, Sharp E. Physiotherapy and rehabilitation following soft tissue surgery of the knee. Orthop Trauma. 2010;24(2):129-138.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedMeserve - ↑ 4.0 4.1 4.2 4.3 4.4 4.5 4.6 4.7 4.8 Cite error: Invalid
<ref>tag; no text was provided for refs namedTeller - ↑ CRTechnologies. Steinman I Sign Test (CR). Available from: http://www.youtube.com/watch?v=31mbTI4CsUI[last accessed 15/12/12]
- ↑ CRTechnologies. Ege's Test (CR). Available from: http://www.youtube.com/watch?v=BVXDEAYPYCg[last accessed 15/12/12]
- ↑ Kohn D, Aagaard H, Verdonk R, Dienst M, Seil R. Postoperative follow-up and rehabilitation after meniscus replacement. Scand J Med Sci Sports. 1999;9(3):177-80.fckLR
- ↑ 8.0 8.1 Thomson LC, Handoll HH, Cunningham A, Shaw PC. Physiotherapist-led programmes and interventions for rehabilitation of anterior cruciate ligament, medial collateral ligament and meniscal injuries of the knee in adults. Cochrane Database Syst Rev. 2002;(2):CD001354.
- ↑ MegaElectronicsLtd. Biofeedback rehabilitation after ACL reconstruction (eMotion Biofeedback). Available from: http://www.youtube.com/watch?v=MQYo8B8wKWc[last accessed 15/12/12]