Anterior Cruciate Ligament (ACL): Difference between revisions
No edit summary |
Bruno Serra (talk | contribs) m (Removed rogue links on references) |
||
| (41 intermediate revisions by 13 users not shown) | |||
| Line 2: | Line 2: | ||
'''Original Editor '''- [[User:Rachael Lowe|Rachael Lowe]] | '''Original Editor '''- [[User:Rachael Lowe|Rachael Lowe]] | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} [[User:Tarang Jain|Tarang | '''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} [[User:Tarang Jain|Tarang Jai]] | ||
</div> | </div> | ||
== Introduction == | == Introduction == | ||
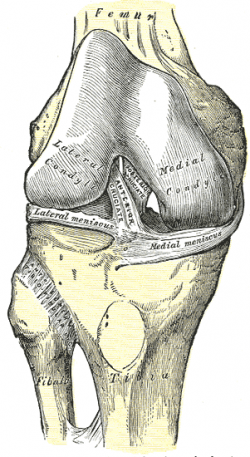
The anterior cruciate ligament (ACL) is a band of dense connective tissue which courses from the femur to the tibia. The ACL is a key structure in the knee joint, as it resists anterior tibial translation and rotational loads. | The anterior cruciate ligament (ACL) is a band of dense connective tissue which courses from the femur to the tibia. It consists of type I (90%) and type III collagen<ref name=":0">Avalos RM, Torres-González EM, Padilla-Medina JR, Monllau JC. ACL ANATOMY: IS THERE STILL SOMETHING TO LEARN?. Revista Española de Cirugía Ortopédica y Traumatología. 2023 Feb 12.</ref>. The length of ACL ranges from 27 to 38 mm and the width from 10 to 12 mm. The cross-section area measures approximately 44 mm sq<ref name=":0" />. It represents an hourglass or bowtie shape. The ACL is a key structure in the knee joint, as it resists anterior tibial translation and internal rotational loads as well as valgus angulation. | ||
{| cellspacing="1" cellpadding="1" width="60%" border="0" align="center" | {| cellspacing="1" cellpadding="1" width="60%" border="0" align="center" | ||
| Line 20: | Line 20: | ||
=== Origin === | === Origin === | ||
Originates from the tibial plateau between and anterior to the intercondylar eminences.<ref name="Purnell">Hassebrock JD, Gulbrandsen MT, Asprey WL, Makovicka JL, Chhabra A. Knee ligament anatomy and biomechanics. Sports medicine and arthroscopy review. 2020 Sep 1;28(3):80-6.</ref>. This femoral attachment of ACL is on posterior part of medial surface of the lateral condyle well posterior to the longitudinal axis of the femoral shaft. The attachment is actually an interdigitation of collagen fibres & rigid bone through the transitional zone of fibrocartilage and mineralized fibrocartilage<ref>Wheeless, C,R. Wheeless' Textbook of Orthopaedics. [http://www.wheelessonline.com/ortho/anatomy_of_acl http://www.wheelessonline.com/ortho/anatomy_of_acl] Accessed 8/1/12.</ref>. | |||
=== Orientation === | === Orientation === | ||
| Line 32: | Line 30: | ||
[[Image:Lat.meniscus.gif|right|300px]] | [[Image:Lat.meniscus.gif|right|300px]] | ||
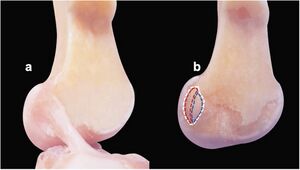
It inserts on the lateral intercondylar ridge (also known as the resident's ridge) and the lateral bifurcate ridge (also known as the cruciate ridge) on the lateral femoral condyle.<ref>Schillhammer CK, Reid III JB, Rister J, Jani SS, Marvil SC, Chen AW, Anderson CG, D'Agostino S, Lubowitz JH. Arthroscopy up to date: anterior cruciate ligament anatomy. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2016 Jan 1;32(1):209-12.</ref> Both the medial and lateral intercondylar tubercles of the tibia serve as the attachment points for the two anteromedial and posterolateral bundles of the ACL.<ref name="Purnell" />.<br> For more detail on the anatomy of the ACL, please see this page: [[Anterior Cruciate Ligament (ACL) - Structure and Biomechanical Properties]] | |||
[[File:Insertion site of ACL on Femur.jpg|300px]] | |||
== Nerve Supply == | == Nerve Supply == | ||
The ACL receives nerve | The ACL receives nerve fibres from the posterior articular branches of the tibial nerve. <ref name="Kennedy">Kennedy JC, Alexander IJ, Hayes KC. Nerve supply of the human knee and its functional importance. Am J Sports Med. 1982 Nov-Dec;10(6):329-35.</ref> These fibres penetrate the posterior joint capsule and run along with the synovial and periligamentous vessels surrounding the ligament to reach as far anterior to the infrapatellar fat pad.<ref name="Kennedy" /> Most of the fibres are associated with the endoligamentous vasculature and have a vasomotor function. The receptors of the nerve fibres mentioned are as follows: | ||
*Ruffini receptors are sensitive to stretching and are located at the surface of the ligament, predominantly on the femoral portion where the deformations are the greatest. <ref name="Haus">Haus J, Halata Z. Innervation of the anterior cruciate ligament. Int Orthop. 1990;14(3):293-6.</ref> | |||
*Vater–Pacini receptors are sensitive to rapid movements and are located at the femoral and tibial ends of the ACL. <ref name="Haus" /> | |||
*Golgi-like tension receptors are located near the attachments of the ACL as well as at its surface, beneath the synovial membrane. <ref name="Kennedy" /> | |||
< | *Free-nerve endings function as nociceptors, but they may also serve as local effectors by releasing neuropeptides with vasoactive function. Thus, they may have a modulatory effect in normal tissue homeostasis or in the late remodelling of grafts. <ref name="Haus" /><ref name="Hogervorst">Hogervorst T, Brand RA. Mechanoreceptors in joint function. J Bone Joint Surg Am. 1998 Sep;80(9):1365-78.</ref> | ||
The mechanoreceptors cited above (Ruffini, Pacini, and Golgi-like receptors) have a proprioceptive function and provide the afferent arc for signalling knee postural changes. Deformations within the ligament influence the output of muscle spindles through the fusimotor system. <ref name="Hogervorst" /> Hence, activation of afferent nerve fibres in the proximal part of the ACL influences motor activity in the muscles around the knee; a phenomenon called the ‘‘ACL reflex.’’ These muscular responses are elicited by stimulation of group II or III fibres (i.e. mechanoreceptors). The ACL reflex is an essential part of normal knee function and is involved in the updating of muscle programs.<ref name="Konishi 2002">Konishi Y, Fukubayashi T, Takeshita D. Possible mechanism of quadriceps femoris weakness in patients with ruptured anterior cruciate ligament. Med Sci Sports Exerc. 2002 Sep;34(9):1414-8. </ref> This becomes even more obvious in patients with a ruptured ACL, where the loss of feedback from mechanoreceptors in the ACL leads to quadriceps femoris weakness.<ref name="Konishi 2002" /> Indeed, this afferent feedback from the ACL has a major influence on the maximal voluntary contraction exertion of the quadriceps femoris. <ref name="Konishi 2003">Konishi Y, Suzuki Y, Hirose N, Fukubayashi T. Effects of lidocaine into knee on QF strength and EMG in patients with ACL lesion. Med Sci Sports Exerc. 2003 Nov;35(11):1805-8.</ref> | |||
== Vascular Supply == | == Vascular Supply == | ||
{| cellspacing="1" cellpadding="1" width="40%" border="0" align="right" class="FCK__ShowTableBorders" | |||
|- | |||
| align="right" | | |||
{{#ev:youtube|RTV5Yo3E7VQ|300}} <ref>Dr. Bertram Zarins, MD. Knee Ligament Anatomy Animation. Available from: http://www.youtube.com/watch?v=RTV5Yo3E7VQ[last accessed 04/10/14]</ref> | |||
|} | |||
The ACL | The major blood supply of the cruciate ligaments arises from the middle genicular artery. Additionally, the inferior genicular arteries and diffusion through the synovial sheath of the ACL also contribute to the overall process.<ref name="Purnell" /> <ref>Markatos K, Kaseta MK, Lallos SN, Korres DS, Efstathopoulos N. The anatomy of the ACL and its importance in ACL reconstruction. European Journal of Orthopaedic Surgery & Traumatology. 2013 Oct;23:747-52.</ref> The AMB and PLB are separated by a connective tissue septum that contains vascular stem cells. This membrane has periligamentous vessels that penetrate the ligament horizontally and connect with a longitudinal network of endoligamentous vessels that supply blood to the ACL.<ref>Irarrázaval S, Albers M, Chao T, Fu FH. Gross, arthroscopic, and radiographic anatomies of the anterior cruciate ligament: foundations for anterior cruciate ligament surgery. Clinics in sports medicine. 2017 Jan 1;36(1):9-23.</ref> The density of blood vessels within the ligaments is not homogeneous.<ref name="Petersen 1999">Petersen W, Tillmann B. Structure and vascularization of the cruciate ligaments of the human knee joint. Anat Embryol (Berl). 1999 Sep;200(3):325-34. </ref> In the ACL, an avascular zone is located within the fibrocartilage of the anterior part where the ligament faces the anterior rim of the intercondylar fossa.<ref name="Petersen 1999" /> The coincidence of poor vascularity and the presence of fibrocartilage is also seen in gliding tendons in areas that are subjected to compressive loads, and the coincidence of these two factors undoubtedly plays a role in the poor healing potential of the ACL. <ref name="Giori">Giori NJ, Beaupré GS, Carter DR. Cellular shape and pressure may mediate mechanical control of tissue composition in tendons. J Orthop Res. 1993 Jul;11(4):581-91. </ref> | ||
== Bundles == | |||
== | {| cellspacing="1" cellpadding="1" width="40%" border="0" align="right" class="FCK__ShowTableBorders" | ||
|- | |||
| align="right" | | |||
{{#ev:youtube|RwwxtD-xT4Y|300}} <ref>Non-Contact ACL Injury, Treatment and Rehabilitation Animation. The Normal Function of the Anterior Cruciate Ligament. Available from: http://www.youtube.com/watch?v=RwwxtD-xT4Y[last accessed 04/10/14]</ref> | |||
|} | |||
For a longer period of time, only two bundles of ACL were identified. However, recent studies suggest that there are three components of the ACL, the smaller anteromedial bundle (AMB), the intermediate bundle and the larger posterolateral bundle (PLB) <ref>MacKay JW, Whitehead H, Toms AP. Radiological evidence for the triple bundle anterior cruciate ligament. Clinical Anatomy. 2014 Oct;27(7):1097-102.</ref>. The AMB and the PMB are distinguished by a tissue sheath in between them and their differing insertion sites.<ref name="Purnell" /> | |||
The | The anteromedial bundle is tight in flexion whereas the posterolateral bundle is stretched in extension. In extension both bundles are parallel. In flexion, the femoral insertion site of the posterolateral bundle moves anteriorly, both bundles are crossed, the anteromedial bundle tightens and the posterolateral bundle loosens. | ||
With the knee extended, resistance to anterior | With the knee extended, resistance to anterior translation of the tibia, [[Lachman Test|Lachmans Test]], is by the bulky posterolateral bundle. With the knee flexed, resistance to anterior translation of the tibia, the [[Anterior Drawer Test of the Knee|Anterior Drawer Test]], is by the anterior medial bundle. | ||
Rupture of the posterolateral bundle | Rupture of the posterolateral bundle causes an increase in hyperextension, anterior translation (extended knee), increase in external and internal rotation (knee extended), and increases in external rotation with the knee in mid-flexion; Rupture of the anteromedial bundle causes anterolateral instability with an increase in anterior translation in flexion, minimal increase in hyperextension, and minimal rotational instability. | ||
For more detail on the ACL bundles, please see this page: [[Anterior Cruciate Ligament (ACL) - Structure and Biomechanical Properties|Anterior Cruciate Ligament (ACL) - Structure and Biomechanical Properties]] | For more detail on the ACL bundles, please see this page: [[Anterior Cruciate Ligament (ACL) - Structure and Biomechanical Properties|Anterior Cruciate Ligament (ACL) - Structure and Biomechanical Properties]] | ||
| Line 72: | Line 78: | ||
== Function == | == Function == | ||
The ACL provides approximately 85% of total restraining force of anterior translation. It also prevents excessive tibial medial and lateral rotation, as well as varus and valgus stresses. To a lesser degree, the ACL checks extension and hyperextension. Together with the posterior cruciate ligament (PCL), the ACL guides the instantaneous center of rotation of the knee, therefore controlling joint kinematics. While the anteromedial bundle is the primary restraint against anterior tibial translation, the posterolateral bundle tends to stabilize the knee near full extension, particularly against rotatory loads<ref>Petersen W, Zantop T. [http://www.ncbi.nlm.nih.gov/pubmed/17075382 Anatomy of the anterior cruciate ligament with regard to its two bundles]. Clin Orthop Relat Res. 2007 Jan;454:35-47</ref>. | The ACL provides approximately 85% of the total restraining force of anterior translation. It also prevents excessive tibial medial and lateral rotation, as well as varus and valgus stresses. To a lesser degree, the ACL checks extension and hyperextension. Together with the posterior cruciate ligament (PCL), the ACL guides the instantaneous center of rotation of the knee, therefore controlling joint kinematics. While the anteromedial bundle is the primary restraint against anterior tibial translation, the posterolateral bundle tends to stabilize the knee near full extension, particularly against rotatory loads<ref>Petersen W, Zantop T. [http://www.ncbi.nlm.nih.gov/pubmed/17075382 Anatomy of the anterior cruciate ligament with regard to its two bundles]. Clin Orthop Relat Res. 2007 Jan;454:35-47</ref>. | ||
==Video== | |||
{{#ev:youtube|LL7l4i-Dp8M}} | |||
== Presentations == | |||
<div class="coursebox"> | |||
{| cellspacing="4" cellpadding="4" width="100%" border="0" class="FCK__ShowTableBorders" | |||
|- | |||
| align="center" | <imagemap> | |||
Image:ACL injury presentation slideshow title.png|200px|border|left| | |||
rect 0 0 830 452 [http://www.slideshare.net/slideshow/embed_code/1609713/] | |||
desc none | |||
</imagemap> | |||
| [http://www.slideshare.net/slideshow/embed_code/1609713/ '''Anterior Cruciate Ligament Injury'''] | |||
This presentation, created by Terdsak Rojsurakitti, Doctor at Managed Care, discusses anatomy, mechanism of injury, surgical options and rehabilitation of ACL tears. [http://www.slideshare.net/slideshow/embed_code/1609713/ Anterior Cruciate Ligament Injury/ View the presentation] | |||
|} | |||
</div> | </div> | ||
== References == | == References == | ||
<references /> | <references /> | ||
[[Category:Anatomy]] [[Category: | [[Category:Anatomy]] [[Category:Knee]] [[Category:Ligaments]] [[Category:Biomechanics]] [[Category:Musculoskeletal/Orthopaedics]] [[Category:Knee - Anatomy]] [[Category:Knee - Ligaments]] | ||
[[Category:Course Pages]] | |||
Latest revision as of 16:10, 23 July 2023
Original Editor - Rachael Lowe
Top Contributors - Laura Ritchie, Admin, Kim Jackson, Rujuta Naik, Evan Thomas, Bruno Serra, Joao Costa, Scott Buxton, George Prudden, WikiSysop, Vidya Acharya, Rucha Gadgil, Ewa Jaraczewska and 127.0.0.1 Tarang Jai
Introduction[edit | edit source]
The anterior cruciate ligament (ACL) is a band of dense connective tissue which courses from the femur to the tibia. It consists of type I (90%) and type III collagen[1]. The length of ACL ranges from 27 to 38 mm and the width from 10 to 12 mm. The cross-section area measures approximately 44 mm sq[1]. It represents an hourglass or bowtie shape. The ACL is a key structure in the knee joint, as it resists anterior tibial translation and internal rotational loads as well as valgus angulation.
|
|
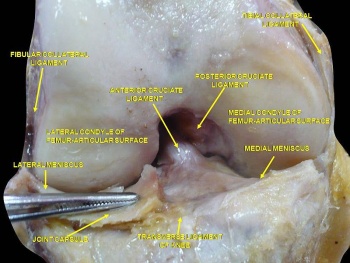
Attachments[edit | edit source]
Origin[edit | edit source]
Originates from the tibial plateau between and anterior to the intercondylar eminences.[2]. This femoral attachment of ACL is on posterior part of medial surface of the lateral condyle well posterior to the longitudinal axis of the femoral shaft. The attachment is actually an interdigitation of collagen fibres & rigid bone through the transitional zone of fibrocartilage and mineralized fibrocartilage[3].
Orientation[edit | edit source]
It runs inferiorly, medially and anteriorly.
Insertion[edit | edit source]
It inserts on the lateral intercondylar ridge (also known as the resident's ridge) and the lateral bifurcate ridge (also known as the cruciate ridge) on the lateral femoral condyle.[4] Both the medial and lateral intercondylar tubercles of the tibia serve as the attachment points for the two anteromedial and posterolateral bundles of the ACL.[2].
For more detail on the anatomy of the ACL, please see this page: Anterior Cruciate Ligament (ACL) - Structure and Biomechanical Properties
Nerve Supply[edit | edit source]
The ACL receives nerve fibres from the posterior articular branches of the tibial nerve. [5] These fibres penetrate the posterior joint capsule and run along with the synovial and periligamentous vessels surrounding the ligament to reach as far anterior to the infrapatellar fat pad.[5] Most of the fibres are associated with the endoligamentous vasculature and have a vasomotor function. The receptors of the nerve fibres mentioned are as follows:
- Ruffini receptors are sensitive to stretching and are located at the surface of the ligament, predominantly on the femoral portion where the deformations are the greatest. [6]
- Vater–Pacini receptors are sensitive to rapid movements and are located at the femoral and tibial ends of the ACL. [6]
- Golgi-like tension receptors are located near the attachments of the ACL as well as at its surface, beneath the synovial membrane. [5]
- Free-nerve endings function as nociceptors, but they may also serve as local effectors by releasing neuropeptides with vasoactive function. Thus, they may have a modulatory effect in normal tissue homeostasis or in the late remodelling of grafts. [6][7]
The mechanoreceptors cited above (Ruffini, Pacini, and Golgi-like receptors) have a proprioceptive function and provide the afferent arc for signalling knee postural changes. Deformations within the ligament influence the output of muscle spindles through the fusimotor system. [7] Hence, activation of afferent nerve fibres in the proximal part of the ACL influences motor activity in the muscles around the knee; a phenomenon called the ‘‘ACL reflex.’’ These muscular responses are elicited by stimulation of group II or III fibres (i.e. mechanoreceptors). The ACL reflex is an essential part of normal knee function and is involved in the updating of muscle programs.[8] This becomes even more obvious in patients with a ruptured ACL, where the loss of feedback from mechanoreceptors in the ACL leads to quadriceps femoris weakness.[8] Indeed, this afferent feedback from the ACL has a major influence on the maximal voluntary contraction exertion of the quadriceps femoris. [9]
Vascular Supply[edit | edit source]
| [10] |
The major blood supply of the cruciate ligaments arises from the middle genicular artery. Additionally, the inferior genicular arteries and diffusion through the synovial sheath of the ACL also contribute to the overall process.[2] [11] The AMB and PLB are separated by a connective tissue septum that contains vascular stem cells. This membrane has periligamentous vessels that penetrate the ligament horizontally and connect with a longitudinal network of endoligamentous vessels that supply blood to the ACL.[12] The density of blood vessels within the ligaments is not homogeneous.[13] In the ACL, an avascular zone is located within the fibrocartilage of the anterior part where the ligament faces the anterior rim of the intercondylar fossa.[13] The coincidence of poor vascularity and the presence of fibrocartilage is also seen in gliding tendons in areas that are subjected to compressive loads, and the coincidence of these two factors undoubtedly plays a role in the poor healing potential of the ACL. [14]
Bundles[edit | edit source]
| [15] |
For a longer period of time, only two bundles of ACL were identified. However, recent studies suggest that there are three components of the ACL, the smaller anteromedial bundle (AMB), the intermediate bundle and the larger posterolateral bundle (PLB) [16]. The AMB and the PMB are distinguished by a tissue sheath in between them and their differing insertion sites.[2]
The anteromedial bundle is tight in flexion whereas the posterolateral bundle is stretched in extension. In extension both bundles are parallel. In flexion, the femoral insertion site of the posterolateral bundle moves anteriorly, both bundles are crossed, the anteromedial bundle tightens and the posterolateral bundle loosens.
With the knee extended, resistance to anterior translation of the tibia, Lachmans Test, is by the bulky posterolateral bundle. With the knee flexed, resistance to anterior translation of the tibia, the Anterior Drawer Test, is by the anterior medial bundle.
Rupture of the posterolateral bundle causes an increase in hyperextension, anterior translation (extended knee), increase in external and internal rotation (knee extended), and increases in external rotation with the knee in mid-flexion; Rupture of the anteromedial bundle causes anterolateral instability with an increase in anterior translation in flexion, minimal increase in hyperextension, and minimal rotational instability.
For more detail on the ACL bundles, please see this page: Anterior Cruciate Ligament (ACL) - Structure and Biomechanical Properties
Function[edit | edit source]
The ACL provides approximately 85% of the total restraining force of anterior translation. It also prevents excessive tibial medial and lateral rotation, as well as varus and valgus stresses. To a lesser degree, the ACL checks extension and hyperextension. Together with the posterior cruciate ligament (PCL), the ACL guides the instantaneous center of rotation of the knee, therefore controlling joint kinematics. While the anteromedial bundle is the primary restraint against anterior tibial translation, the posterolateral bundle tends to stabilize the knee near full extension, particularly against rotatory loads[17].
Video[edit | edit source]
Presentations[edit | edit source]
 |
Anterior Cruciate Ligament Injury
This presentation, created by Terdsak Rojsurakitti, Doctor at Managed Care, discusses anatomy, mechanism of injury, surgical options and rehabilitation of ACL tears. Anterior Cruciate Ligament Injury/ View the presentation |
References[edit | edit source]
- ↑ 1.0 1.1 Avalos RM, Torres-González EM, Padilla-Medina JR, Monllau JC. ACL ANATOMY: IS THERE STILL SOMETHING TO LEARN?. Revista Española de Cirugía Ortopédica y Traumatología. 2023 Feb 12.
- ↑ 2.0 2.1 2.2 2.3 Hassebrock JD, Gulbrandsen MT, Asprey WL, Makovicka JL, Chhabra A. Knee ligament anatomy and biomechanics. Sports medicine and arthroscopy review. 2020 Sep 1;28(3):80-6.
- ↑ Wheeless, C,R. Wheeless' Textbook of Orthopaedics. http://www.wheelessonline.com/ortho/anatomy_of_acl Accessed 8/1/12.
- ↑ Schillhammer CK, Reid III JB, Rister J, Jani SS, Marvil SC, Chen AW, Anderson CG, D'Agostino S, Lubowitz JH. Arthroscopy up to date: anterior cruciate ligament anatomy. Arthroscopy: The Journal of Arthroscopic & Related Surgery. 2016 Jan 1;32(1):209-12.
- ↑ 5.0 5.1 5.2 Kennedy JC, Alexander IJ, Hayes KC. Nerve supply of the human knee and its functional importance. Am J Sports Med. 1982 Nov-Dec;10(6):329-35.
- ↑ 6.0 6.1 6.2 Haus J, Halata Z. Innervation of the anterior cruciate ligament. Int Orthop. 1990;14(3):293-6.
- ↑ 7.0 7.1 Hogervorst T, Brand RA. Mechanoreceptors in joint function. J Bone Joint Surg Am. 1998 Sep;80(9):1365-78.
- ↑ 8.0 8.1 Konishi Y, Fukubayashi T, Takeshita D. Possible mechanism of quadriceps femoris weakness in patients with ruptured anterior cruciate ligament. Med Sci Sports Exerc. 2002 Sep;34(9):1414-8.
- ↑ Konishi Y, Suzuki Y, Hirose N, Fukubayashi T. Effects of lidocaine into knee on QF strength and EMG in patients with ACL lesion. Med Sci Sports Exerc. 2003 Nov;35(11):1805-8.
- ↑ Dr. Bertram Zarins, MD. Knee Ligament Anatomy Animation. Available from: http://www.youtube.com/watch?v=RTV5Yo3E7VQ[last accessed 04/10/14]
- ↑ Markatos K, Kaseta MK, Lallos SN, Korres DS, Efstathopoulos N. The anatomy of the ACL and its importance in ACL reconstruction. European Journal of Orthopaedic Surgery & Traumatology. 2013 Oct;23:747-52.
- ↑ Irarrázaval S, Albers M, Chao T, Fu FH. Gross, arthroscopic, and radiographic anatomies of the anterior cruciate ligament: foundations for anterior cruciate ligament surgery. Clinics in sports medicine. 2017 Jan 1;36(1):9-23.
- ↑ 13.0 13.1 Petersen W, Tillmann B. Structure and vascularization of the cruciate ligaments of the human knee joint. Anat Embryol (Berl). 1999 Sep;200(3):325-34.
- ↑ Giori NJ, Beaupré GS, Carter DR. Cellular shape and pressure may mediate mechanical control of tissue composition in tendons. J Orthop Res. 1993 Jul;11(4):581-91.
- ↑ Non-Contact ACL Injury, Treatment and Rehabilitation Animation. The Normal Function of the Anterior Cruciate Ligament. Available from: http://www.youtube.com/watch?v=RwwxtD-xT4Y[last accessed 04/10/14]
- ↑ MacKay JW, Whitehead H, Toms AP. Radiological evidence for the triple bundle anterior cruciate ligament. Clinical Anatomy. 2014 Oct;27(7):1097-102.
- ↑ Petersen W, Zantop T. Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res. 2007 Jan;454:35-47