Age-related Hyperkyphosis: Difference between revisions
No edit summary |
No edit summary |
||
| Line 2: | Line 2: | ||
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} |
'''Top Contributors''' - {{Special:Contributors/{{FULLPAGENAME}}}} | ||
</div> | </div> | ||
== Definition/Description | == Definition/Description == | ||
An age-related hyperkyphosis can be described as an exaggerated | An age-related hyperkyphosis affects 20-40% of older adults and can be described as an exaggerated anterior curvature of the thoracic spine that is associated with aging (increasing incidence 6-11% for every 10 years of increasing age).<ref name="Jang et al.">Jang et al., H. (2015). Effect of thorax correction exercises on flexed posture and chest function in older women wih age-related hyperkyphosis. J. Phys. Ther. Sci. , 27, 1161-1164.</ref><br>General causes of age-related hyperkyphosis that have been reported are poor posture, dehydration of the intervertebral discs and reduced back extensor muscle strength. | ||
<br> | Age-related hyperkyphosis can:<br>- lead to mobility impairments of the rib cage (connected to thoracic spine) which can result in pulmonary difficulties<br>- increase biomechanical stress on the spine which can result in increasing risk of development vertebral compression fractures<br>- increase risk of falling and fractures due to poor gait<br>- have an impact on the basic functioning and daily living, which affects the quality of life.<ref name="Katzman et al.">Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.</ref><ref name="Bansal et al.">Bansal et al., S. (2014). Exercise for Improving Age-Related Hyperkyphotic Posture: A systematic Review. Arch Phys Med Rehabil , 95 (1), 129-140.</ref><br> | ||
== Clinically Relevant Anatomy | == Clinically Relevant Anatomy<br> == | ||
< | The spine consists of vertebrae, intervertebral disks and spinal cord and has different regions and curves:<br>• Cervical spine: it contains 7 vertebrae (C1-C7) and has a lordotic curve. This region has the greatest mobility.<br>• Thoracic spine: it contains 12 vertebrae (T1-T12) which are connected with the ribs. And the thoracic spine has a kyphotic curve. <br>• Lumbar spine: it contains 5 vertebrae (L1-L5) which are the largest and strongest. The lumbar spine has a lordotic curve.<br>• Sacrum/coccyx: the sacrum contains 5 fused vertebrae (S1-S5) and the coccyx 4 (sometimes 5) fused vertebrae. They have a kyphotic curve. | ||
Hyperkyphosis is most common in the thoracic spine. The thoracic spine is relatively stiff compared to the rest of the spine, because of the rib cage, ligaments and thin, rigid intervertebral discs.<ref name="Mulligan et al.">Mulligan et al., B. (2015). The Mulligan Concept of Manual Therapy: Textbook of Techniques. Chatswood, NSW, Australia: Elsevier.</ref><br>The thoracic spine has frontal orientated facet joints which allow flexion and extension but these movements are small because of the limitation of the rib cage. Lateralflexion and rotation needs translation in these joints. The rotation in the thoracic spine decreases with flexion, so hyperkyphosis limits the 3D movement. <br>There are ligaments between the ribs and vertebrae and these ligaments limits the rotation of the thorax but only in the transverse plane. Hyperkyphosis changes the posture, plane. More flexion (more hyperkyphosis) results in more instability. <br>So the ranges and patterns of coupled motion of the thorax appear to be strongly influenced by the posture from which the movement is initiated.<ref name="Edmondston et al.">Edmondston et al., S. (2007). Influence of posture on the range of axial rotation and coupled lateral flexion of the thoracic spine. Manipulative Phys Ther , 30 (3), 193-9.</ref><br>[[Image:Vertebra.jpg]]<br> | |||
== Epidemiology /Etiology == | |||
Thoracic kyphosis varies in life between 20-29 degrees. After the age of 40 the kyphosis angle begins to increase. Usually more rapidly in women than men, the angle varies between 43 to 52 degrees in women aged 55-60 years to 52 degrees in women between 76-80 years of age.<br>Incidence and prevalence of hyperkyphosis vary between 20% to 40% among both men and women. | |||
<ref name="Katzman et al.">Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.</ref> | |||
<br>Exaggeration of the normal thoracic curvature can be associated with a variety of conditions and psychosocial factors such as depression, insecurity, despondency and anxiety. | |||
<ref name="Fon et al.">Fon et al., G. (1980). Thoracic kyphosis: range in normal subjects. AJR Am J Roentgenol , 134 (5), 979-83.</ref><ref name="Lewis et al.">Lewis et al., J. (2010). Clinical measurement of the thoracic kyphosis. A study of the intra-rater reliability in subjects with and without shoulder pain. BMC Musculoskeletal Disorders , 1 (11), 39.</ref> | |||
<br>Different causes can lead to a thoracal hyperkyphosis, such as the gradual changes in structure and mechanics of connective tissue which in time results in a loss of elasticity and mobility, this causes the inability to counteract gravitation that pulls the body forward. | |||
<ref name="Hinman et al.">Hinman et al., M. (2004). Comparison of thoracic kyphosis and postural stiffness in younger and older women. Spine J , 4 (4), 413-7.</ref><ref name="Katzman et al.">Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.</ref> | |||
<br>Hyperkyphosis may develop further with muscle weakness (often because of a weakening spinal extensor muscle) | |||
<ref name="Hinman et al.">Hinman et al., M. (2004). Comparison of thoracic kyphosis and postural stiffness in younger and older women. Spine J , 4 (4), 413-7.</ref> | |||
, degenerative disc disease, low bone mineral density which in time can lead to vertebral fractures and an even worsening hyperkyphosis. Initial fractures due to a fall can precipitate the development of a hyperkyphosis. | |||
<ref name="Katzman et al.">Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.</ref> | |||
<br>Deficits in the somatosensory, visual and vestibular systems contribute to the loss of upright postural control. Due to a declining proprioceptive and vibratory input from the joints in the lower extremities, this results in a perception of erect vertical alignment that is impaired. | |||
<ref name="Katzman et al.">Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.</ref> | |||
<br>Mortality rate of Hyperkyphosis increases with the hyperkyphotic posture. With hyperkyposis, a loss of vital capacity is associated, and severe hyperkyphosis is predictive of pulmonary death among community dwelling women. | |||
<ref name="Katzman et al.">Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.</ref> | |||
<br> | |||
== Characteristics/Clinical Presentation | == Characteristics/Clinical Presentation == | ||
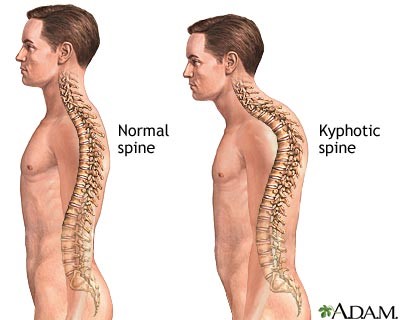
Thoracal Hyperkyphosis is recognizable by different symptoms, the main one being an increase in the anterior curvature of the thoracic spine (more prominent upper back). This can come over time and isn’t always detected by the patient, but rather by his friends and family. When a person has a sudden increase of rounded back, it is necessary to go see a doctor. Sudden changes in the spine curve can be associated with other health problems. | |||
Along with this physical characteristic, people with Hyperkyphosis tend to have more difficulty rising from a chair without their arms, have a poorer balance (they have the feeling that they might fall), slower gait velocity, wider base of support with stance and gait (to avoid falling) and decreased stair climbing speed.<ref name="Katzman et al.">Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.</ref><br>In severe cases of Hyperkyphosis, people can have trouble breathing, because of the loss of vital capacity of the lungs.<ref name="Katzman et al.">Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.</ref><br> | |||
[[Image:Kyphotic_spine.jpg]]<br> | |||
== Differential diagnosis<br> == | == Differential diagnosis<br> == | ||
== Diagnostic Procedures<ref name=" | •[http://www.physio-pedia.com/Osteoporosis Osteoporosis]<br>• Vertebrale fracture <br>• Muscle imbalance caused by neuromuscular disease<br>• [http://www.physio-pedia.com/Ankylosing_Spondylitis ankylosing spondylitis]<br> | ||
== Diagnostic Procedures == | |||
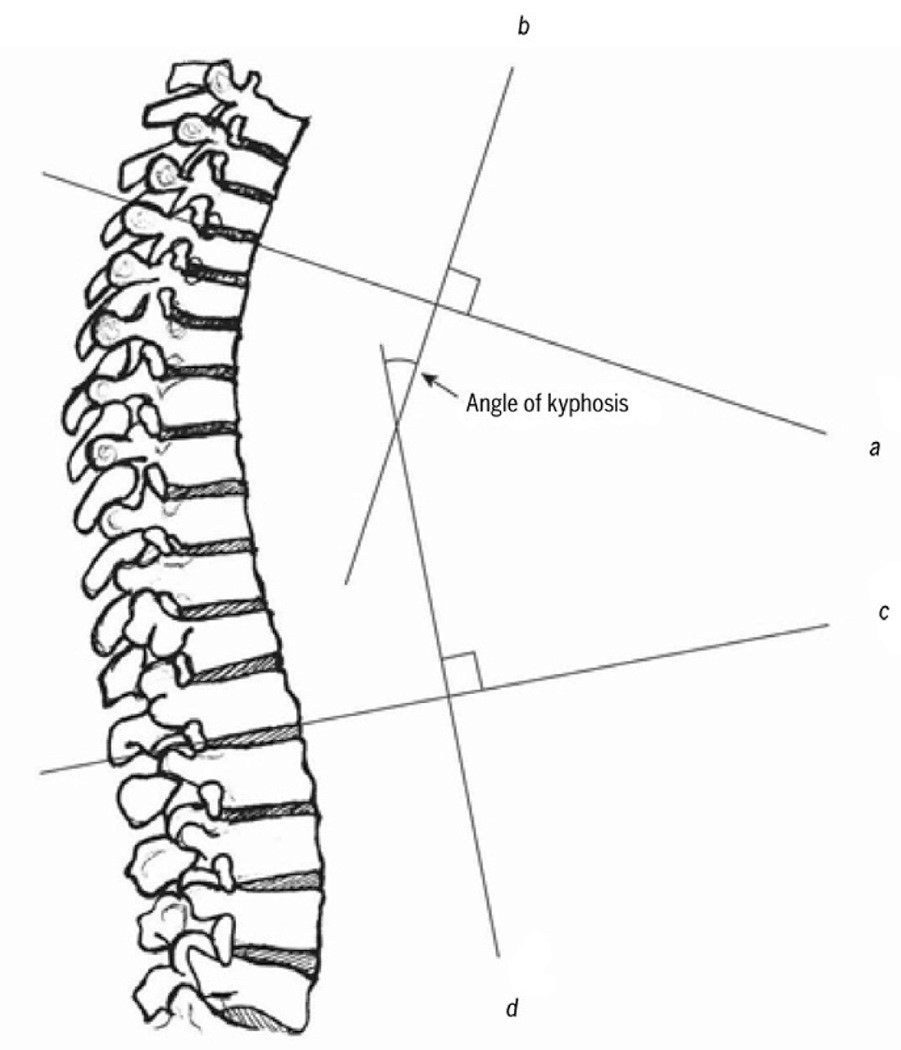
There are different validated diagnostic procedures for measuring hyperkyfosis:<br><br>''Radiologic measurements'' <br>• The most validated method is an orthopedic technique for assessment of thoracic kyphosis assessed from standing lateral spine radiographs. Elderly subjects can also do this in the supine position for more comfort. From these radiographs the Cobb’s angle of kyphosis can be calculated from perpendicular lines drawn on a standard thoracic spine radiograph: a line extends through the superior endplate of the vertebral body, marking the beginning of the thoracic curve (usually at T3/T4), and the inferior endplate of the vertebral body, marking the end of the thoracic curve (usually at T12).<ref name="Mulligan et al.">Mulligan et al., B. (2015). The Mulligan Concept of Manual Therapy: Textbook of Techniques. Chatswood, NSW, Australia: Elsevier.</ref> When the angle is between 20-40° we consider it as a normal kyphosis, higher angles are considered as hyperkyphosis. However, there can be an overestimation of the kyphosis in the presence of vertebral body end-plate deformation or fracture. In this case there is an alternative method for measuring the Cobb’s angle. In this alternative method the cobbs angle is measured by extending lines from the mid-points of the superior and inferior end-plates of T4 and T9.<ref name="Goh et al. ">Goh et al. (2000). A comparison of three methods for measuring thoracic kyphosis: implications for clinical studies. Rheumatology , 310-315.</ref><br> | |||
[[Image:Cobbs_angle.jpg]]<br> | |||
<br>''Standing clinical measurement ''<br>• The kyphometer measures the angle of kyphosis, the arms of the device are placed at the top and bottom of the thoracic curve (spinous processes of T2/T3 superiorly, and T1/T12 inferiorly). Using a mathematical formula we can strongly correlated with the radiologic measured thoracic Cobb’s angle.<ref name="Korovessis et al.">Korovessis et al. (2001). Prediction of thoracic kyphosis using the Debrunner kyphometer. J Spinal Disord , 67-72.</ref><br>• The flexicurve ruler is a flexible ruler that is aligned over the C7 spinous process to the L5–S1; the ruler is molded to the curvature of the spine. The kyphosis index is calculated as the width divided by the length of the thoracic curve, multiplied by 100. A kyphosis index value greater than 13 is defined as hyperkyphotic.<ref name="Teixeira et al. ">Teixeira et al. (2007). Reliability and validity of thoracic kyphosis measurements using the flexicurve method. Brazilian Journal of Physical Therapy , 199-204.</ref><br><br>There is reasonable correlation (ICC = 0.68) between a radiologic and standing clinical measurement of kyphosis.<ref name="Kado et al. 2006">Kado et al. (2006). Comparing a supine radiologic versus standing clinical measurement of kyphosis in older women: the Fracture Intervention Trial. Spine , 463-467.</ref><br><br> | |||
== Outcome Measures == | == Outcome Measures == | ||
• Scoliosis Research Society Outcomes Instrument (SRS-22) | |||
The SRS -22 scores function, pain, self-image, mental health, and satisfaction with management. There are findings that associate more hyperkyphosis with increased pain, lower self-image, and decreased general function and overall activity. The r values for this analysis of kyphosis (0.40–0.66) were significantly greater than those reported for scoliosis magnitude versus SRS questionnaire scores (0.16–0.26). Therefore the SRS outcomes instrument may be even better suited for the evaluation of hyperkyphosis patients. <ref name="Petcharaporn et al.">Petcharaporn et al. (2007). The Relationship Between Thoracic Hyperkyphosis and the Scoliosis Research Society Outcomes Instrument. Spine , 226-231.</ref><br><br>• [http://www.physio-pedia.com/Neck_Pain_and_Disability_Scale Neck Pain and Disability Scale]<br> | |||
== Examination<br> == | |||
An estimation of a hyperkyphotic posture can be made by <br>• qualitative visual assessment: <br> the therapist should evaluate the anterior curvature of the spine, keeping in mind that changes in thoracic curvature can be caused by a modified posture in other regions (e.g. lumbar spine)<br>• and: measuring the occiput to wall distance (if greater than 0cm)<br>• and: measurement of the number of 1.5-cm blocks needed to support the head. <br>There are no studies comparing these measures to the gold-standard radiograph.<ref name="Kado et al. 2009">Kado DM. (2009). The rehabilitation of hyperkyphotic posture in the elderly. Eur J Phys Rehabil Med , 583-93</ref><br> | |||
== Medical Management<br> == | |||
There are no medications that will cure the hyperkyphosis.<br>Pharmacological treatment is focussed on anti-resportive or bone-building medcation because many patients with age-related hyperkyphosis have low bone density or spine fractures.<ref name="Katzman et al.">Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.</ref><br>There are 2 surgical options: vertebroplasty and kyphoplasty.<ref name="Goh et al.">Goh et al. (2000). A comparison of three methods for measuring thoracic kyphosis: implications for clinical studies. Rheumatology , 310-315.</ref> These options mainly help relieve pain and decrease physical disability, but in some cases, surgery can reduce the kyphosis angle. <br><br>''Kyphoplasty: ''<br>Kyphoplasty is a surgical prodecure that is used to reduce the pain in patients that have spinal fractures. This surgery can correct spine deformation like hyperkyphosis. <ref name="Pradhan et al.">Pradhan et al., B. (2006). Kyphoplasty reduction of osteoporotic vertebral compression fractures: correction of local kyphosis versus overall sagittal alignment. Spine , 15 (31(4)), 435-41.</ref> <ref name="Goh et al.">Goh et al. (2000). A comparison of three methods for measuring thoracic kyphosis: implications for clinical studies. Rheumatology , 310-315.</ref><br>The produce involves injecting a balloon in the fractured vertebrae, which will be inflated so that it pushes the broken parts to back their initial place. When the balloon is removed, a cement gel is injected to harden and stabilize the bone. <ref name="Hulme et al.">Hulme et al., P. (2006). Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine , 31 (17), 1983-2001.</ref> <ref name="Wardlaw et al.">Wardlaw et al., D. (2009). Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet , 373 (9668), 1016-24.</ref><br>The balloon is injected with a tube and the incision is made in the back, the tube passes from the back to the fractured spine.<ref name="Hulme et al.">Hulme et al., P. (2006). Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine , 31 (17), 1983-2001.</ref><br>The risk of this surgery is that the cement can leak, and potentially damage the spinal cord.<ref name="Pradhan et al.">Pradhan et al., B. (2006). Kyphoplasty reduction of osteoporotic vertebral compression fractures: correction of local kyphosis versus overall sagittal alignment. Spine , 15 (31(4)), 435-41.</ref><br><br>''Vertebroplasty: ''<br>This surgery can also reduce the pain in a spine fractured patient, you can also use this surgery for reducing spine deformation. Vertebroplasty is a surgery where you inject with needle an acrylic bone cement directly into the vertebral fracture.<ref name="Pradhan et al.">Pradhan et al., B. (2006). Kyphoplasty reduction of osteoporotic vertebral compression fractures: correction of local kyphosis versus overall sagittal alignment. Spine , 15 (31(4)), 435-41.</ref> <ref name="Wardlaw et al.">Wardlaw et al., D. (2009). Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet , 373 (9668), 1016-24.</ref><br>This surgery has the same risk as a kyphoplasty, namely leaking fluid and potentially damaging the spinal cord.<ref name="Pradhan et al.">Pradhan et al., B. (2006). Kyphoplasty reduction of osteoporotic vertebral compression fractures: correction of local kyphosis versus overall sagittal alignment. Spine , 15 (31(4)), 435-41.</ref><br><br> | |||
== Physical Therapy Management <br> == | |||
A 2014 systematic review of exercise for age-related hyperkyphotic posture concluded that a few high-quality studies did suggest a modest benefit (1.67°-3.74° decrease of hyperkyphosis) for exercise compared to control. (Level of Evidence = 1A)<ref name="Bansal et al.">Bansal et al., S. (2014). Exercise for Improving Age-Related Hyperkyphotic Posture: A systematic Review. Arch Phys Med Rehabil , 95 (1), 129-140.</ref><br> | |||
Ideally these exercises should (initially) be supervised by a physical therapist or certified instructor in order to be effective and safe. <br>The exercise modalities and dosage should be adapted to capacities and needs of the individual patient.<br><br>The main goals of physical therapy management should be:<ref name="Katzman et al.">Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.</ref><br>• Increased back extensor strength<br>• Increased spinal extension mobility<br>• Improved postural awareness<br>• Fewer incidences of vertebral compression fractures | |||
Exercise modalities include:<br>(EVERYTHING BELOW HAS BEEN STUDIED USING RCTs: LEVEL OF EVIDENCE = 2B)<br>• (Hatha) Yoga modified for individuals with hyperkyphosis<ref name="Greendale et al.">Greendale et al., G. (2009). Yoga decreases kyphosis in senior women and men with adult-onset hyperkyphosis: results of a randomized controlled trial. J Am Geriatr Soc , 57, 1569-79.</ref><br> Postures should focus on breathing techniques, stretching tight muscle groups and strengthening weak/inhibited muscle groups (e.g. rhomboids) | |||
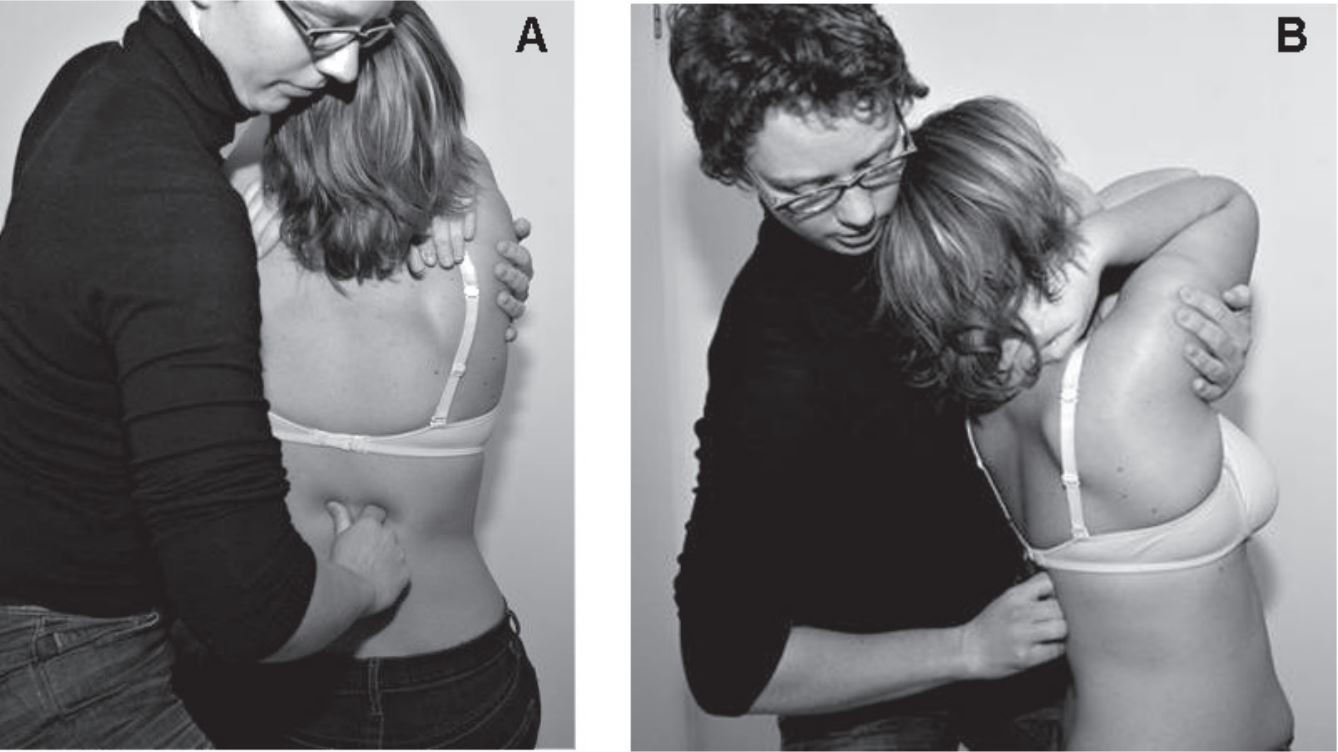
• Manual mobilisations<ref name="Bautmans et al. ">Bautmans et al., I. (2010). Rehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosis. J Rehabil Med. , 42, 129-135.</ref> <ref name="Bennell et al.">Bennell et al., K. (2010). Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC Musculoskelet Disord , 11-36.</ref>:<br> Mobilisations should be done according to [http://www.physio-pedia.com/Maitland's_Mobilisations Maitland Joint Mobilization Grading Scale] <br> | |||
[[Image:Manual_mobilisations.jpg]]<br> | |||
<br> | |||
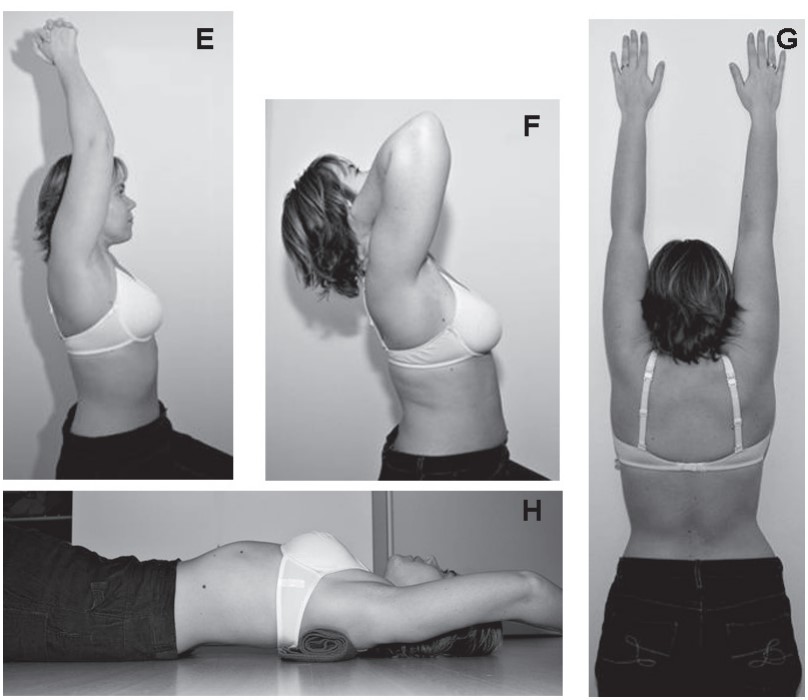
• Active mobilisations/stretches<ref name="Bautmans et al.">Bautmans et al., I. (2010). Rehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosis. J Rehabil Med. , 42, 129-135.</ref><ref name="Bennell et al.">Bennell et al., K. (2010). Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC Musculoskelet Disord , 11-36.</ref><br> | |||
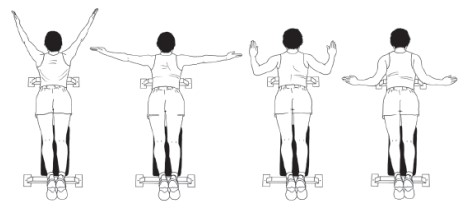
[[Image:Active_mobilisation.jpg]]<br> | |||
<br> | |||
• Muscle strengthening <ref name="Abreu et al.">Abreu et al., D. (2012). The effect of physical exercise on thoracic hyperkyphosis in elderly postmenopausal patients with osteoporosis. Osteoporosis Int. , 23, 120.</ref> <ref name="Bautmans et al.">Bautmans et al., I. (2010). Rehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosis. J Rehabil Med. , 42, 129-135.</ref> <ref name="Benedetti et al.">Benedetti et al., M. (2008). Effects of an adapted physical activity program in a group of elderly subjects wtih flexed posture: clinical and strumental assessment. J Neuroeng Rehabil , 5, 32.</ref> <ref name="Itoi et al.">Itoi et al., E. (1994). Effects of back-strengthening exercise on posture in healthy women 49 to 65 years of age. Mayo Clin Proc , 69, 1054-9.</ref><br> Thoracic extension (paravertebral muscles)<br> | |||
[[Image:Thoracic_extension.jpg]]<br> | |||
Abdominal muscles<br> Scapular adductors<br> | |||
[[Image:Scapular_adductors.jpg]]<br> | |||
Shoulder anteflexion, adduction, abduction <ref name="Abreu et al.">Abreu et al., D. (2012). The effect of physical exercise on thoracic hyperkyphosis in elderly postmenopausal patients with osteoporosis. Osteoporosis Int. , 23, 120.</ref><br> Standing elbow flexion/extension<br> | |||
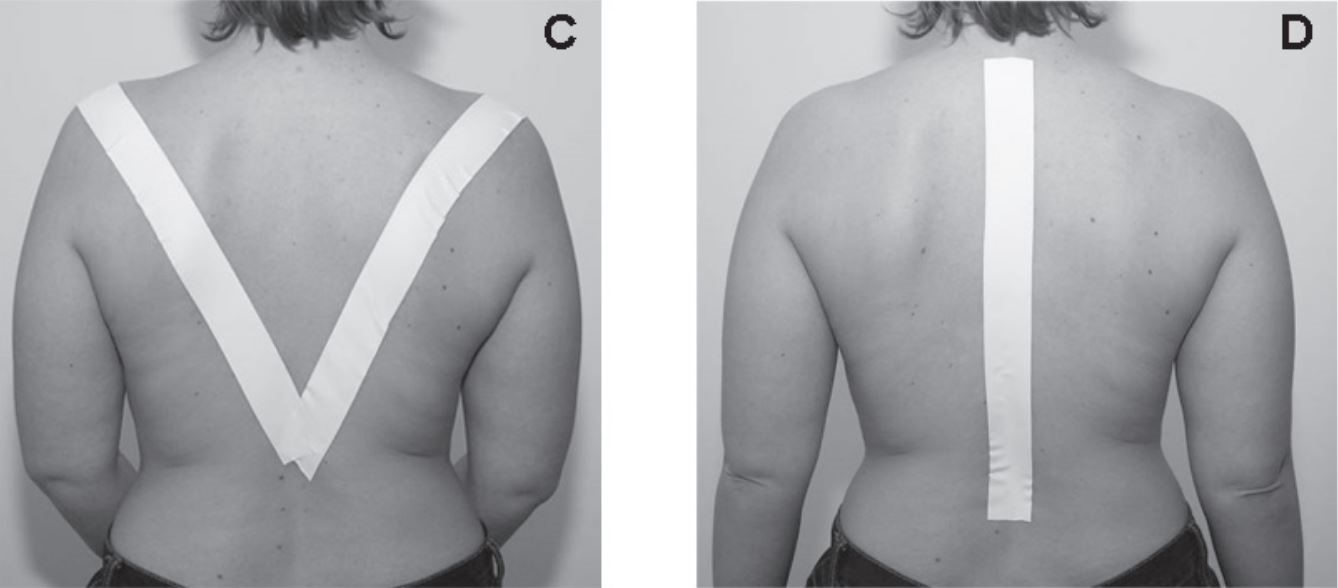
• Postural awareness training (standing, sitting), with feedback<ref name="Abreu et al.">Abreu et al., D. (2012). The effect of physical exercise on thoracic hyperkyphosis in elderly postmenopausal patients with osteoporosis. Osteoporosis Int. , 23, 120.</ref>:<br>- visual (images, mirror)<br>- and/or auditive (therapist giving cues)<br>- and/or tactile (therapist, taping <ref name="Bautmans et al.">Bautmans et al., I. (2010). Rehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosis. J Rehabil Med. , 42, 129-135.</ref> <ref name="Bennell et al. ">Bennell et al., K. (2010). Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC Musculoskelet Disord , 11-36.</ref>) | |||
Postural awareness training steps: <br>- Explaining the patient what the problematic posture is<br>- Demonstration correct posture correction, explaining every motion that should be made:<br> Belly button in & down (soft contraction)<br> Knees slightly bent<br> Shoulders back (=scapular retraction): it can help to do external rotation in the shoulder to accompany this motion<br> Chest up<br> Chin slightly tucked in<br>- Have the patient try this him/herself, the first time still going over every cue<br>- Once the patient has practiced the posture a sufficient amount of times to immediately be able to resume good posture on command, taping and random reminders (timer) can be used to ensure the posture is kept during the day.<br><br>[[Image:PostureTraining.jpg]]<br> | |||
<br> | |||
[[Image:PostureTaping.jpg]]<br> | |||
<br> | |||
== Key Research<br> == | |||
1. Systematic review of exercise therapy for thoracic hyperkyphosis by Bansal et al. (2014)<br>[http://www.ncbi.nlm.nih.gov/pubmed/23850611 http://www.ncbi.nlm.nih.gov/pubmed/23850611] <br><br>2. RCT by Bautmans et al. using exercise and mobilizations, with a relatively detailed description of the intervention.<br>[http://www.ncbi.nlm.nih.gov/pubmed/20140408 http://www.ncbi.nlm.nih.gov/pubmed/20140408 ]<br> | |||
== Resources<br> == | |||
1. [http://www.spineuniverse.com/conditions/kyphosis/anatomy-kyphosis http://www.spineuniverse.com/conditions/kyphosis/anatomy-kyphosis]<br><br>2. Zane M. Hyperkyphosis (Humpback) in Adults [Internet]. American Physical Therapy Association. 2014 [cited 8 May 2016]. Available from: [http://www.moveforwardpt.com/SymptomsConditionsDetail.aspx?cid=a26d7f6b-85dd-4461-9685-be7a8e5d5725 http://www.moveforwardpt.com/SymptomsConditionsDetail.aspx?cid=a26d7f6b-85dd-4461-9685-be7a8e5d5725]<br><br>3. Article that provides detailed instructions for various exercises: [https://www.t-nation.com/training/heal-that-hunchback https://www.t-nation.com/training/heal-that-hunchback]<br> | |||
== | == <br>Clinical Bottom Line<br> == | ||
Age-related hyperkyphosis, an excessive anterior concavity of the thoracic spine, is a condition that affects many older adults (20-40%). Hyperkyphosis can impair pulmonary<br>function3 and activities of daily living performance, reduce quality of life, and predict<br>mortality independent of underlying spinal osteoporosis.<br><br> | |||
== Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | == Recent Related Research (from [http://www.ncbi.nlm.nih.gov/pubmed/ Pubmed]) == | ||
<div class="researchbox"><rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1b5VuYnHtAIWGInUSYOs1mCpcBsRSZJTKKcKxRYfa7S77tw9mR|Short|max=10</rss></div><div class="researchbox"></div> | <div class="researchbox"><rss>http://www.ncbi.nlm.nih.gov/entrez/eutils/erss.cgi?rss_guid=1b5VuYnHtAIWGInUSYOs1mCpcBsRSZJTKKcKxRYfa7S77tw9mR|Short|max=10</rss></div><div class="researchbox"> Effect of thorax correction exercises on flexed posture and chest function in older women with age-related hyperkyphosis.<br></div><div class="researchbox"></div> | ||
== References == | == References == | ||
Revision as of 23:09, 12 June 2016
Top Contributors - Louise Burrion, Kim Jackson, Lucinda hampton, Mariam Hashem, Yuan Chuang, Evan Thomas, Stijn Van de Vondel, 127.0.0.1, Admin, Borms Killian, Gayatri Jadav Upadhyay, Oyemi Sillo, Magdalena Hytros, Ajay Upadhyay, Cedric Cludts, WikiSysop and Lauren Lopez
Definition/Description[edit | edit source]
An age-related hyperkyphosis affects 20-40% of older adults and can be described as an exaggerated anterior curvature of the thoracic spine that is associated with aging (increasing incidence 6-11% for every 10 years of increasing age).[1]
General causes of age-related hyperkyphosis that have been reported are poor posture, dehydration of the intervertebral discs and reduced back extensor muscle strength.
Age-related hyperkyphosis can:
- lead to mobility impairments of the rib cage (connected to thoracic spine) which can result in pulmonary difficulties
- increase biomechanical stress on the spine which can result in increasing risk of development vertebral compression fractures
- increase risk of falling and fractures due to poor gait
- have an impact on the basic functioning and daily living, which affects the quality of life.[2][3]
Clinically Relevant Anatomy
[edit | edit source]
The spine consists of vertebrae, intervertebral disks and spinal cord and has different regions and curves:
• Cervical spine: it contains 7 vertebrae (C1-C7) and has a lordotic curve. This region has the greatest mobility.
• Thoracic spine: it contains 12 vertebrae (T1-T12) which are connected with the ribs. And the thoracic spine has a kyphotic curve.
• Lumbar spine: it contains 5 vertebrae (L1-L5) which are the largest and strongest. The lumbar spine has a lordotic curve.
• Sacrum/coccyx: the sacrum contains 5 fused vertebrae (S1-S5) and the coccyx 4 (sometimes 5) fused vertebrae. They have a kyphotic curve.
Hyperkyphosis is most common in the thoracic spine. The thoracic spine is relatively stiff compared to the rest of the spine, because of the rib cage, ligaments and thin, rigid intervertebral discs.[4]
The thoracic spine has frontal orientated facet joints which allow flexion and extension but these movements are small because of the limitation of the rib cage. Lateralflexion and rotation needs translation in these joints. The rotation in the thoracic spine decreases with flexion, so hyperkyphosis limits the 3D movement.
There are ligaments between the ribs and vertebrae and these ligaments limits the rotation of the thorax but only in the transverse plane. Hyperkyphosis changes the posture, plane. More flexion (more hyperkyphosis) results in more instability.
So the ranges and patterns of coupled motion of the thorax appear to be strongly influenced by the posture from which the movement is initiated.[5]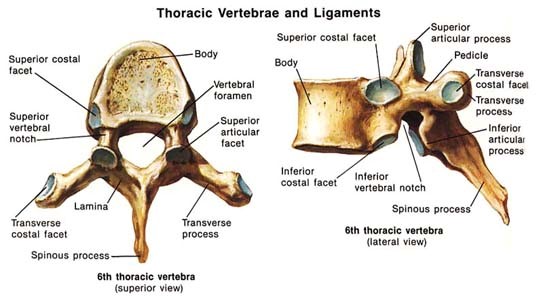
Epidemiology /Etiology[edit | edit source]
Thoracic kyphosis varies in life between 20-29 degrees. After the age of 40 the kyphosis angle begins to increase. Usually more rapidly in women than men, the angle varies between 43 to 52 degrees in women aged 55-60 years to 52 degrees in women between 76-80 years of age.
Incidence and prevalence of hyperkyphosis vary between 20% to 40% among both men and women.
[2]
Exaggeration of the normal thoracic curvature can be associated with a variety of conditions and psychosocial factors such as depression, insecurity, despondency and anxiety.
[6][7]
Different causes can lead to a thoracal hyperkyphosis, such as the gradual changes in structure and mechanics of connective tissue which in time results in a loss of elasticity and mobility, this causes the inability to counteract gravitation that pulls the body forward.
[8][2]
Hyperkyphosis may develop further with muscle weakness (often because of a weakening spinal extensor muscle)
[8]
, degenerative disc disease, low bone mineral density which in time can lead to vertebral fractures and an even worsening hyperkyphosis. Initial fractures due to a fall can precipitate the development of a hyperkyphosis.
[2]
Deficits in the somatosensory, visual and vestibular systems contribute to the loss of upright postural control. Due to a declining proprioceptive and vibratory input from the joints in the lower extremities, this results in a perception of erect vertical alignment that is impaired.
[2]
Mortality rate of Hyperkyphosis increases with the hyperkyphotic posture. With hyperkyposis, a loss of vital capacity is associated, and severe hyperkyphosis is predictive of pulmonary death among community dwelling women.
[2]
Characteristics/Clinical Presentation[edit | edit source]
Thoracal Hyperkyphosis is recognizable by different symptoms, the main one being an increase in the anterior curvature of the thoracic spine (more prominent upper back). This can come over time and isn’t always detected by the patient, but rather by his friends and family. When a person has a sudden increase of rounded back, it is necessary to go see a doctor. Sudden changes in the spine curve can be associated with other health problems.
Along with this physical characteristic, people with Hyperkyphosis tend to have more difficulty rising from a chair without their arms, have a poorer balance (they have the feeling that they might fall), slower gait velocity, wider base of support with stance and gait (to avoid falling) and decreased stair climbing speed.[2]
In severe cases of Hyperkyphosis, people can have trouble breathing, because of the loss of vital capacity of the lungs.[2]
Differential diagnosis
[edit | edit source]
•Osteoporosis
• Vertebrale fracture
• Muscle imbalance caused by neuromuscular disease
• ankylosing spondylitis
Diagnostic Procedures[edit | edit source]
There are different validated diagnostic procedures for measuring hyperkyfosis:
Radiologic measurements
• The most validated method is an orthopedic technique for assessment of thoracic kyphosis assessed from standing lateral spine radiographs. Elderly subjects can also do this in the supine position for more comfort. From these radiographs the Cobb’s angle of kyphosis can be calculated from perpendicular lines drawn on a standard thoracic spine radiograph: a line extends through the superior endplate of the vertebral body, marking the beginning of the thoracic curve (usually at T3/T4), and the inferior endplate of the vertebral body, marking the end of the thoracic curve (usually at T12).[4] When the angle is between 20-40° we consider it as a normal kyphosis, higher angles are considered as hyperkyphosis. However, there can be an overestimation of the kyphosis in the presence of vertebral body end-plate deformation or fracture. In this case there is an alternative method for measuring the Cobb’s angle. In this alternative method the cobbs angle is measured by extending lines from the mid-points of the superior and inferior end-plates of T4 and T9.[9]
Standing clinical measurement
• The kyphometer measures the angle of kyphosis, the arms of the device are placed at the top and bottom of the thoracic curve (spinous processes of T2/T3 superiorly, and T1/T12 inferiorly). Using a mathematical formula we can strongly correlated with the radiologic measured thoracic Cobb’s angle.[10]
• The flexicurve ruler is a flexible ruler that is aligned over the C7 spinous process to the L5–S1; the ruler is molded to the curvature of the spine. The kyphosis index is calculated as the width divided by the length of the thoracic curve, multiplied by 100. A kyphosis index value greater than 13 is defined as hyperkyphotic.[11]
There is reasonable correlation (ICC = 0.68) between a radiologic and standing clinical measurement of kyphosis.[12]
Outcome Measures[edit | edit source]
• Scoliosis Research Society Outcomes Instrument (SRS-22)
The SRS -22 scores function, pain, self-image, mental health, and satisfaction with management. There are findings that associate more hyperkyphosis with increased pain, lower self-image, and decreased general function and overall activity. The r values for this analysis of kyphosis (0.40–0.66) were significantly greater than those reported for scoliosis magnitude versus SRS questionnaire scores (0.16–0.26). Therefore the SRS outcomes instrument may be even better suited for the evaluation of hyperkyphosis patients. [13]
• Neck Pain and Disability Scale
Examination
[edit | edit source]
An estimation of a hyperkyphotic posture can be made by
• qualitative visual assessment:
the therapist should evaluate the anterior curvature of the spine, keeping in mind that changes in thoracic curvature can be caused by a modified posture in other regions (e.g. lumbar spine)
• and: measuring the occiput to wall distance (if greater than 0cm)
• and: measurement of the number of 1.5-cm blocks needed to support the head.
There are no studies comparing these measures to the gold-standard radiograph.[14]
Medical Management
[edit | edit source]
There are no medications that will cure the hyperkyphosis.
Pharmacological treatment is focussed on anti-resportive or bone-building medcation because many patients with age-related hyperkyphosis have low bone density or spine fractures.[2]
There are 2 surgical options: vertebroplasty and kyphoplasty.[9] These options mainly help relieve pain and decrease physical disability, but in some cases, surgery can reduce the kyphosis angle.
Kyphoplasty:
Kyphoplasty is a surgical prodecure that is used to reduce the pain in patients that have spinal fractures. This surgery can correct spine deformation like hyperkyphosis. [15] [9]
The produce involves injecting a balloon in the fractured vertebrae, which will be inflated so that it pushes the broken parts to back their initial place. When the balloon is removed, a cement gel is injected to harden and stabilize the bone. [16] [17]
The balloon is injected with a tube and the incision is made in the back, the tube passes from the back to the fractured spine.[16]
The risk of this surgery is that the cement can leak, and potentially damage the spinal cord.[15]
Vertebroplasty:
This surgery can also reduce the pain in a spine fractured patient, you can also use this surgery for reducing spine deformation. Vertebroplasty is a surgery where you inject with needle an acrylic bone cement directly into the vertebral fracture.[15] [17]
This surgery has the same risk as a kyphoplasty, namely leaking fluid and potentially damaging the spinal cord.[15]
Physical Therapy Management
[edit | edit source]
A 2014 systematic review of exercise for age-related hyperkyphotic posture concluded that a few high-quality studies did suggest a modest benefit (1.67°-3.74° decrease of hyperkyphosis) for exercise compared to control. (Level of Evidence = 1A)[3]
Ideally these exercises should (initially) be supervised by a physical therapist or certified instructor in order to be effective and safe.
The exercise modalities and dosage should be adapted to capacities and needs of the individual patient.
The main goals of physical therapy management should be:[2]
• Increased back extensor strength
• Increased spinal extension mobility
• Improved postural awareness
• Fewer incidences of vertebral compression fractures
Exercise modalities include:
(EVERYTHING BELOW HAS BEEN STUDIED USING RCTs: LEVEL OF EVIDENCE = 2B)
• (Hatha) Yoga modified for individuals with hyperkyphosis[18]
Postures should focus on breathing techniques, stretching tight muscle groups and strengthening weak/inhibited muscle groups (e.g. rhomboids)
• Manual mobilisations[19] [20]:
Mobilisations should be done according to Maitland Joint Mobilization Grading Scale
• Active mobilisations/stretches[19][20]
• Muscle strengthening [21] [19] [22] [23]
Thoracic extension (paravertebral muscles)
Abdominal muscles
Scapular adductors
Shoulder anteflexion, adduction, abduction [21]
Standing elbow flexion/extension
• Postural awareness training (standing, sitting), with feedback[21]:
- visual (images, mirror)
- and/or auditive (therapist giving cues)
- and/or tactile (therapist, taping [19] [20])
Postural awareness training steps:
- Explaining the patient what the problematic posture is
- Demonstration correct posture correction, explaining every motion that should be made:
Belly button in & down (soft contraction)
Knees slightly bent
Shoulders back (=scapular retraction): it can help to do external rotation in the shoulder to accompany this motion
Chest up
Chin slightly tucked in
- Have the patient try this him/herself, the first time still going over every cue
- Once the patient has practiced the posture a sufficient amount of times to immediately be able to resume good posture on command, taping and random reminders (timer) can be used to ensure the posture is kept during the day.
File:PostureTraining.jpg
Key Research
[edit | edit source]
1. Systematic review of exercise therapy for thoracic hyperkyphosis by Bansal et al. (2014)
http://www.ncbi.nlm.nih.gov/pubmed/23850611
2. RCT by Bautmans et al. using exercise and mobilizations, with a relatively detailed description of the intervention.
http://www.ncbi.nlm.nih.gov/pubmed/20140408
Resources
[edit | edit source]
1. http://www.spineuniverse.com/conditions/kyphosis/anatomy-kyphosis
2. Zane M. Hyperkyphosis (Humpback) in Adults [Internet]. American Physical Therapy Association. 2014 [cited 8 May 2016]. Available from: http://www.moveforwardpt.com/SymptomsConditionsDetail.aspx?cid=a26d7f6b-85dd-4461-9685-be7a8e5d5725
3. Article that provides detailed instructions for various exercises: https://www.t-nation.com/training/heal-that-hunchback
Clinical Bottom Line
[edit | edit source]
Age-related hyperkyphosis, an excessive anterior concavity of the thoracic spine, is a condition that affects many older adults (20-40%). Hyperkyphosis can impair pulmonary
function3 and activities of daily living performance, reduce quality of life, and predict
mortality independent of underlying spinal osteoporosis.
Recent Related Research (from Pubmed)[edit | edit source]
References[edit | edit source]
- ↑ Jang et al., H. (2015). Effect of thorax correction exercises on flexed posture and chest function in older women wih age-related hyperkyphosis. J. Phys. Ther. Sci. , 27, 1161-1164.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 2.6 2.7 2.8 2.9 Katzman et al., W. B. (2010). Age-related hyperkyphosis: its causes, management, and consequences. J Orthop Sports Phys Ther , 40, 352-360.
- ↑ 3.0 3.1 Bansal et al., S. (2014). Exercise for Improving Age-Related Hyperkyphotic Posture: A systematic Review. Arch Phys Med Rehabil , 95 (1), 129-140.
- ↑ 4.0 4.1 Mulligan et al., B. (2015). The Mulligan Concept of Manual Therapy: Textbook of Techniques. Chatswood, NSW, Australia: Elsevier.
- ↑ Edmondston et al., S. (2007). Influence of posture on the range of axial rotation and coupled lateral flexion of the thoracic spine. Manipulative Phys Ther , 30 (3), 193-9.
- ↑ Fon et al., G. (1980). Thoracic kyphosis: range in normal subjects. AJR Am J Roentgenol , 134 (5), 979-83.
- ↑ Lewis et al., J. (2010). Clinical measurement of the thoracic kyphosis. A study of the intra-rater reliability in subjects with and without shoulder pain. BMC Musculoskeletal Disorders , 1 (11), 39.
- ↑ 8.0 8.1 Hinman et al., M. (2004). Comparison of thoracic kyphosis and postural stiffness in younger and older women. Spine J , 4 (4), 413-7.
- ↑ 9.0 9.1 9.2 Goh et al. (2000). A comparison of three methods for measuring thoracic kyphosis: implications for clinical studies. Rheumatology , 310-315.
- ↑ Korovessis et al. (2001). Prediction of thoracic kyphosis using the Debrunner kyphometer. J Spinal Disord , 67-72.
- ↑ Teixeira et al. (2007). Reliability and validity of thoracic kyphosis measurements using the flexicurve method. Brazilian Journal of Physical Therapy , 199-204.
- ↑ Kado et al. (2006). Comparing a supine radiologic versus standing clinical measurement of kyphosis in older women: the Fracture Intervention Trial. Spine , 463-467.
- ↑ Petcharaporn et al. (2007). The Relationship Between Thoracic Hyperkyphosis and the Scoliosis Research Society Outcomes Instrument. Spine , 226-231.
- ↑ Kado DM. (2009). The rehabilitation of hyperkyphotic posture in the elderly. Eur J Phys Rehabil Med , 583-93
- ↑ 15.0 15.1 15.2 15.3 Pradhan et al., B. (2006). Kyphoplasty reduction of osteoporotic vertebral compression fractures: correction of local kyphosis versus overall sagittal alignment. Spine , 15 (31(4)), 435-41.
- ↑ 16.0 16.1 Hulme et al., P. (2006). Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine , 31 (17), 1983-2001.
- ↑ 17.0 17.1 Wardlaw et al., D. (2009). Efficacy and safety of balloon kyphoplasty compared with non-surgical care for vertebral compression fracture (FREE): a randomised controlled trial. Lancet , 373 (9668), 1016-24.
- ↑ Greendale et al., G. (2009). Yoga decreases kyphosis in senior women and men with adult-onset hyperkyphosis: results of a randomized controlled trial. J Am Geriatr Soc , 57, 1569-79.
- ↑ 19.0 19.1 19.2 19.3 Bautmans et al., I. (2010). Rehabilitation using manual mobilization for thoracic kyphosis in elderly postmenopausal patients with osteoporosis. J Rehabil Med. , 42, 129-135.
- ↑ 20.0 20.1 20.2 Bennell et al., K. (2010). Effects of an exercise and manual therapy program on physical impairments, function and quality-of-life in people with osteoporotic vertebral fracture: a randomised, single-blind controlled pilot trial. BMC Musculoskelet Disord , 11-36.
- ↑ 21.0 21.1 21.2 Abreu et al., D. (2012). The effect of physical exercise on thoracic hyperkyphosis in elderly postmenopausal patients with osteoporosis. Osteoporosis Int. , 23, 120.
- ↑ Benedetti et al., M. (2008). Effects of an adapted physical activity program in a group of elderly subjects wtih flexed posture: clinical and strumental assessment. J Neuroeng Rehabil , 5, 32.
- ↑ Itoi et al., E. (1994). Effects of back-strengthening exercise on posture in healthy women 49 to 65 years of age. Mayo Clin Proc , 69, 1054-9.